| Author | Affiliation |
|---|---|
| Reetta Marciano, MD, MSN | University of Maryland, Department of Psychiatry, Baltimore, Maryland |
| Diana M. Mullis, MD | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
| Edward C. Jauch, MD, MS | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
| Christine M. Carr, MD | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
| Larry Raney, MD | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
| Renee’ H. Martin, PhD | Medical University of South Carolina, Division of Biostatistics and Epidemiology, Charleston, South Carolina |
| Brenda J. Walker, BS | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
| Steven H. Saef, MD, MSCR | Medical University of South Carolina, Division of Emergency Medicine, Charleston, South Carolina |
ABSTRACT
Introduction:
We determined if targeted education of emergency physicians (EPs) regarding the treatment of mental illness will improve their comfort level in treating psychiatric patients boarding in the emergency department (ED) awaiting admission.
Methods:
We performed a pilot study examining whether an educational intervention would change an EP’s comfort level in treating psychiatric boarder patients (PBPs). We identified a set of psychiatric emergencies that typically require admission or treatment beyond the scope of practice of emergency medicine. Diagnoses included major depression, schizophrenia, schizoaffective disorder, bipolar affective disorder, general anxiety disorder, suicidal ideation, and criminal behavior. We designed equivalent surveys to be used before and after an educational intervention. Each survey consisted of 10 scenarios of typical psychiatric patients. EPs were asked to rate their comfort levels in treating the described patients on a visual analogue scale. We calculated summary scores for the non intervention survey group (NINT) and intervention survey group (INT) and compared them using Student’s t-test.
Results:
Seventy-nine percent (33/42) of eligible participants completed the pre-intervention survey (21 attendings, 12 residents) and comprised the NINT group. Fifty-five percent (23/42) completed the post-intervention survey (16 attendings, 7 residents) comprising the INT group. A comparison of summary scores between ‘NINT’ and ‘INT’ groups showed a highly significant improvement in comfort levels with treating the patients described in the scenarios (P = 0.003). Improvements were noted on separate analysis for faculty (P = 0.039) and for residents (P = 0.012). Results of a sensitivity analysis excluding one highly significant scenario showed decreased, but still important differences between the NINT and INT groups for all participants and for residents, but not for faculty (all: P = 0.05; faculty: P = 0.25; residents: P = 0.03).
Conclusion:
This pilot study suggests that the comfort level of EPs, when asked to treat PBPs, may be improved with education. We believe our data support further study of this idea and of whether an improved comfort level will translate to a willingness to treat.
INTRODUCTION
Crowding of emergency departments (EDs) and lack of acceptable available inpatient beds has resulted in increasing numbers of patients being held in the EDs after admission. Among this group are an increasing number of psychiatric boarder patients (PBPs) who await inpatient psychiatric treatment. These patients often languish in the EDs for days without receiving appropriate medication or behavioral therapy, while remaining in an environment not conducive to their recovery. The American College of Emergency Physicians, in collaboration with the American Psychiatric Association and the National Alliance for the Mentally Ill conducted an online survey to determine the number of psychiatric patients who were boarded in EDs in March 2004. Of 340 participating EDs, two thirds of the respondents reported increasing numbers of PBPs.1 A National Health Policy Forum in August 2007 noted that crowding of EDs continues to be a significant problem and the ED lengths of stay of psychiatric patients were noted to be 42% longer than that for medical/surgical patients.2 Slade et al3 reported that the duration of EDs visit increased by 2.3% overall while that of mental health-related visits have increased 42%. A survey conducted at the University of Utah ED showed that psychiatric patients were more likely to be readmitted than medical patients within 30 days (21% versus 13.4%).5 There was a 21.1% increase in state mental health admissions between 2002 and 2005 in 8 key states in the United States.4 A recent study from California revealed a mental health system in crisis where increasing demand for inpatient psychiatric beds is being met with a diminishing supply. This has resulted in wait times for adult psychiatric patients exceeding 16 hours.11 These phenomena may have been augmented by recidivism, emphasizing the urgency of finding a solution for this expanding problem.
The experience of our psychiatric faculty who frequently receive PBPs from outlying hospitals lead us to believe there is a significant subset of psychiatric patients who would benefit from earlier intervention. We believed that the increasing numbers of PBPs could be moderated by emergency physicians (EPs); however, we hypothesized that this was dependent on the “comfort level” of the EPs treating them. Comfort level is a vague quantity and one difficult to describe. For the purposes of this study we defined it as a feeling of ease and security on the part of the treating EPs when tasked with initiating care. It may already be within the scope of practice of emergency medicine (EM) to start appropriate medication for PBPs, who are boarding or will receive close follow up; however, the ability of an EP to act within this scope may depend on their level of comfort with these patients.
We performed a pilot study testing whether an educational intervention could improve an EP’s comfort level in managing these patients. Our hypothesis was that focused instruction would improve the comfort level of EPs in caring for PBPs and thereby facilitate the care for this group of patients.
METHODS
The setting was a Southeastern, urban, academic medical center. We formed a study group consisting of faculty members from the departments of emergency medicine and psychiatry and a medical student with a career interest in emergency psychiatry. The psychiatric faculty member is dedicated to the treatment of PBPs and is considered an expert in their management at our institution. We designed 2 equivalents Data Collection Instruments (DCI) to be used before and after an educational intervention. Each DCI consisted of a survey describing the presentation of 10 emergency psychiatric patients designed to measure EPs’ comfort levels in providing care to psychiatric patients in need of treatment that was beyond the ordinary scope of practice of EPs (see pre-intervention Survey: Appendix I, and post-intervention Survey: Appendix II). Scenarios described in the surveys referred to treatment of major depressive disorder, schizophrenia, schizoaffective disorder, bipolar affective disorder, generalized anxiety disorder, suicidal ideation, and criminal behavior (CB). Our scenarios were derived from our daily practice and represented the most common types of psychiatric emergencies one was likely to see in our busy academic practice. After administration of the pre-intervention survey we provided an educational intervention (Appendix III) designed to educate EPs about the nuances of treating the patients described in the scenarios. This consisted of a Microsoft PowerPoint 2010 presentation that explained the correct treatment of all patients described in the pre-intervention survey. The intervention was presented in a department conference and distributed to all eligible participants by email. After completion of the pre-intervention survey and the educational intervention, the post-intervention survey was distributed by email. Opportunity was provided for study participants to ask questions during the conference and via email to the investigators.
All practicing EPs at the study site were eligible to participate (42 EPs: 18 EM residents and 24 faculty). Because the participants who took the pre-intervention survey were not matched to those taking the post-intervention survey we decided that the most effective way to analyze our results would be to treat the pre-intervention and post-intervention groups as 2 cohorts: a non-intervention group (NINT) and an intervention (INT) group. Hence, though the samples comprising the 2 cohorts were drawn from the same population of EPs at our academic medical center, for the purposes of this pilot study we considered them as independent samples. Therefore, all comparisons were performed using Student’s t-test. Our design was kept simple for practical reasons and we used convenience samples for both surveys. The participants did not receive an incentive to participate.
EPs were asked to rate their comfort levels in treating the patients described in the DCI on a visual analogue scale (VAS). We automated the surveys using a survey construction tool (REDCap Survey Software – Version 1.3.5 – 2010 Vanderbilt University) and distributed them by email to all eligible participants with a letter assuring the voluntary and anonymous nature of the survey. Results were automatically collated by REDCap and uploaded into SAS, Cary, NC for analysis.
We calculated summary scores for the NINT and INT groups by adding the VAS scores for all individual scenarios in each survey. Summary scores for all participants were averaged to obtain an overall summary score for each group. We calculated separate summary scores for residents and faculty. The study was exempted by the Institutional Review Board of the Medical University of South Carolina.
RESULTS
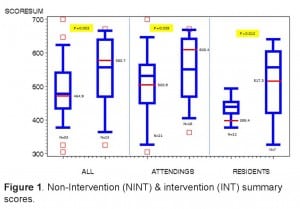
Thirty-three of forty-two (79%) eligible participants completed the pre-intervention survey (21 attendings, 12 residents) and comprised the NINT group. Twenty-three of forty-two (55%) completed the post-intervention survey (16 attendings, 7 residents) and comprised the INT group. Comparison of overall summary scores between the NINT and INT groups showed a highly significant improvement in comfort levels (NINT mean 464.9, INT mean 580.7, P = 0.003). There were also significant improvements in summary scores noted for faculty (NINT mean 500.9, INT mean 608.4, P = 0.039) and for residents (NINT mean 399.4, INT mean 517.3, P = 0.012) (Figure 1).
One scenario, the CB scenario, showed highly significant results for all categories of participants. We therefore performed a sensitivity analysis to determine if our results were driven by this 1 scenario. Results of the sensitivity analysis excluding the CB scenario showed decreased, but still important differences between the scenarios for the total group and for the residents; however, the data for faculty became non-significant (All: NINT mean 449.2, INT mean 520.5, P = 0.05; faculty: NINT mean 487.1, INT mean 544.1, P = 0.25; residents: NINT mean 379.3, INT mean 466.6, P = 0.03) (Figure 2). Tables showing the data for individual scenarios, summary score data, and data from the sensitivity analysis are provided in Appendix IV.
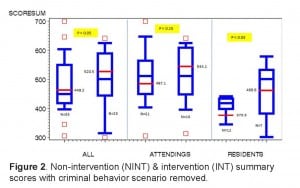
Non-intervention (NINT) & intervention (INT) summary scores with criminal behavior scenario removed.
DISCUSSION
The increasing demands placed on ED resources by PBPs suggest a need to review the current practice of EM. If PBPs received appropriate treatment while waiting for inpatient beds, many of them could improve sufficiently for discharge. Not only is this desirable for the patient, it is operationally crucial to EDs. National EM leaders have expressed serious concerns about the problem of boarder patients in the EDs, pointing out the compromised care and safety of these patients.6 The demand for treatment of behavioral emergencies already exceeds the availability of services in many areas of the U.S. and with further cutback of mental health funding this problem will likely worsen.7
One solution we explored was the feasibility of training ED staff to manage PBPs. Previous studies have shown that ED staff and physicians can provide limited psychiatric care. Patel et al8 demonstrated the effectiveness of a mental health risk-assessment tool that can be used in the EDs to organize the care of mentally ill patients more efficiently. Wulsin et al 9 found that EPs could successfully manage psychiatric patients and initiate therapy.
The financial impact of caring for PBPs is important for the patient and for the EDs. In many cases the ED is unable to bill for holding PBPs. One model to recover cost could be that of an ED psychiatric observation unit. Marchand et al10 showed an ED Psychiatric Observation Unit to be cost-effective, resulting in reduced length of stay, without an increase in suicides and also facilitated rapid decision making and rapid referrals.
Our data suggest that it may be possible to improve the comfort level of EPs in caring for PBPs. The residents’ comfort level showed a significant improvement in response to the educational intervention and, while faculty data did not show a statistically significant change, the direction of the data was in favor of a benefit from the educational intervention. This suggests that, regardless of its ability to change practice, our presentation may be an effective teaching tool worthy of further study.
The improvement seen in the faculty data was driven by the results of the CB scenario. This scenario may represent an area where EPs have a particular need for additional instruction. The highly significant difference between the NINT and INT group scores for this scenario suggests a need for further training of EPs on how to manage patients with criminal behavior.
Our experience seems to show that one may successfully implement this educational intervention in an academic ED and that the potential exists for improving the comfort level of EPs in caring for PBPs. However, based on our findings we believe a future study of our idea with an improved design would be worthwhile. What is needed is a matched, controlled study that will allow us to differentiate the impact of our intervention from a placebo effect. Therefore, a future design should include pairing of participants between the NINT and INT groups. This would enable use of the paired t-test, providing a more effective comparison.
The survey instruments should be validated prior to the study using standard survey validation techniques. Despite their apparent equivalence, item pairs from the 2 surveys should be randomly assigned between the 2 data collection instruments to avoid introducing bias that may be inherent to the individual items. A larger sample obtained from multiple institutions would increase the generalizability of the data. Stratification of results by participants’ years of training and practice would enable one to determine the effect of prior experience on our findings and help define subsets of EP who may experience particular benefit. Also, future studies should examine the relationship between EP’s comfort levels and their willingness to expand their scope of practice to treat PBPs.
In theory, an EP willing to initiate care of psychiatric patients as they would for medical patients who are boarding in the ED could expedite care for these patients, improve ED flow, and reduce cost. We believe that further investigation of our idea using an improved design has the potential to benefit PBPs and streamline ED operations.
LIMITATIONS
Limitations of this study include the small sample size and its confinement to a single academic medical center. Not having validated the surveys using established survey validation techniques limits their ability to measure that which they claim. A lack of randomization in the order of administration of the survey items to participants in the NINT and INT groups introduced bias inherent to idiosyncrasies of the scenarios. Not matching the participants from the NINT and INT groups resulted in a lack of control for variation among participants regarding their practice styles, personalities, knowledge, and experience. Matching participants would permit us to differentiate the effect of the intervention from a placebo effect and improve accuracy by using a paired t-test. A failure to stratify responses by years of training and practice limits our ability to note the impact of these factors on the effectiveness of our intervention. Furthermore, “comfort level” must be distinguished from “willingness” when considered in terms of asking EPs to change their scope of practice.
We were concerned that one scenario, the CB scenario, which showed extremely high significance, might have skewed the overall data. We therefore performed a sensitivity analysis to address this problem. This showed that although one group, the faculty, was strongly influenced by this scenario, the overall findings still suggested that the intervention had merit. A larger sample and a better response rate may have produced more significant results. In future studies an incentive to participate may improve response rate.
Although our study instruments were not validated prior to their use in this study, our scenarios were developed through collaboration between an expert in emergency psychiatry who has practiced EM and is board certified in psychiatry and members of the EM faculty. Further studies are needed to corroborate our findings in a larger more varied setting.
CONCLUSION
This pilot study suggests that it may be possible to improve the comfort level of EPs when asked to treat psychiatric patients, such as those described in our scenarios, by using a focused educational tool. Whether our findings will stand up to more rigorous study and whether a change in comfort level will translate to an expansion of EPs’ scope of practice remains to be seen. We believe that further study of this idea using an improved design is justified given the expanding population of PBPs.
Our findings also support further study of the effectiveness of our educational intervention as a teaching tool, particularly with regard to the CB scenario. The management of patients with criminal behavior appears to be an area where EPs would benefit from additional graduate medical education.
Appendix 1, Appendix 2, Appendix 3, Appendix 4
Footnotes
Supervising Section Editor: Leslie Zun, MD, MBA
Submission history: Submitted December 26, 2010; Revisions received September 20, 2011; Accepted April 17, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.6899
Address for Correspondence: Reetta Marciano MD, MSN, University of Maryland, 701 W. Pratt Street, 4th Floor, Baltimore, MD 21201
Email: reettam@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Mulligan K. ER docs report large increase in psychiatric patients. Psychiatric News.2004;39:10.
2. Salinsky E, Loftis C. National Health Policy Forum website. Available at:http://www.nhpf.org/library/issue-briefs/IB823_InpatientPsych_08-01-07.pdf. Accessed December 18, 2010.
3. Slade EP, Dixon LB, Semmel S. Trends in the duration of emergency department visits.Psychiatric Services. 2010;61:878–884. [PubMed]
4. Mandersheid RW, Atay JE, Crider RA. Changing trends in state psychiatric hospital use from 2002–2005. Psychiatric Services. 2009;60:29–34. [PubMed]
5. Madsen TE, Bennett A, Groke S, et al. Emergency department with psychiatric complaints return at higher rates than controls. Western Journal of Emergency Medicine.2009;10:268–272. [PMC free article] [PubMed]
6. Schneider S. Boarding: perils and solutions. American College of Emergency Physicians website. Available at: http://www.acep.org/MeetingInfo.aspx?id=49674. Accessed December 18, 2010.
7. American Psychiatric Association Emergency departments see dramatic increase in people with mental illness seeking care. American Psychiatric Association website. Available at:http://www.psych.org/MainMenu/Newsroom/NewsReleases/2004NewsReleases/emergencystudy06032004.aspx. Accessed December 18, 2010.
8. Patel AS, Harrison A, Bruce-Jones W. Evaluation of the risk assessment matrix: a mental health triage tool. Emergency Medicine Journal. 2009;26:11–14. [PubMed]
9. Wulsin L, Liu T, Storrow A, et al. A randomized, controlled trial of panic disorder treatment initiation in and emergency department chest pain center. Annals of Emergency Medicine. 2002;39:139–143. [PubMed]
10. Marchand W, Hart M, Carter A, et al. Utilization and outcome in an overnight psychiatric observation program at the Veterans Affairs Medical Center. Psychiatric Services. 2000;51:92–95. [PubMed]
11. Stone A, Rogers D, Kruckenber S, et al. Impact of the mental healthcare delivery system on California emergency department. West J Emerg Med. 2012;13(1):51–56.Available at http://escholarship.org/uc/item/5k4