| Author | Affiliation |
|---|---|
| John C. Stein, MD, MAS | University of California, San Francisco |
| Vanessa L. Jacoby, MD, MAS | University of California, San Francisco |
| Eric Vittinghoff, PhD | University of California, San Francisco |
| Ralph Wang, MD | University of California, San Francisco |
| Elizabeth Kwan, MD | University of California, San Francisco |
| Teri Reynolds, MD | University of California, San Francisco |
| Ian McAlpine, BA | University of California, San Francisco |
| Ralph Gonzales, MD, MPH | University of California, San Francisco |
ABSTRACT
Introduction:
Survey data over the last several decades suggests that emergency department (ED) access to diagnostic ultrasound performed by the radiology department is unreliable, particularly outside of regular business hours. To evaluate the association between the time of day of patient presentation and the use of diagnostic ultrasound services in United States (U.S.) EDs.
Methods:
This was a cross-sectional study of ED patient visits using the National Hospital Ambulatory Medical Care Survey for the years 2003 to 2005. Our main outcome measure was the use of diagnostic ultrasound during the ED patient visit as abstracted from the medical record. We performed multivariate analyses to identify any association between ultrasound use and time of presentation for all patients, as well as for two subgroups who are more likely to need ultrasound as part of their routine workup: patients at risk of deep venous thrombosis, and patients at risk for ectopic pregnancy.
Results:
During the three-year period, we analyzed 110,447 patient encounters, representing 39 million national visits. Of all ED visits, 2.6% received diagnostic ultrasound. Presenting to the ED “off hours” (defined as Monday through Friday 7pm to 7am and weekends) was associated with a lower rate of ultrasound use independent of potential confounders (odds ratio [OR] 0.73, 95% confidence interval [CI]: 0.65 – 0.82). Patients at increased risk of deep venous thrombosis who presented to the ED during “off hours” were also less likely to undergo diagnostic ultrasound (OR 0.34, 95% CI: 0.15 – 0.79). Similarly, patients at increased risk of ectopic pregnancy received fewer diagnostic ultrasounds during “off hours” (OR 0.56, 95% CI 0.35 – 0.91).
Conclusion:
In U.S. EDs, ultrasound use was lower during “off hours,” even among patient populations where its use would be strongly indicated.
INTRODUCTION
Important concerns are emerging regarding disparities in processes and outcomes of care depending on the time of day or day of week a patient seeks healthcare; poorer outcomes among weekend or evening presentations have been reported for a wide range of conditions including myocardial infarction, gastrointestinal bleeding, and stroke.1–9 Potential explanations for this disparity have focused on decreased availability of resources, expertise, and diagnostics on weekends and evenings compared with weekdays.1–9 The emergency department (ED) is a clinical environment subject to variations in access to resources, expertise, and diagnostics at different times during the week due to the continuous nature of its operation.
Ultrasonography is a diagnostic resource that has increasingly been used in the emergent diagnosis and management for a wide variety of conditions during the past two decades, with findings that led the American College of Emergency Physicians to issue resolutions calling for 24-hour availability of ultrasonography for ED patients.10,11 Yet, survey data during subsequent years suggests that ED access to radiology department ultrasonography continues to be unreliable, particularly outside of regular business hours.10–18
The objective of this study was to conduct the first national quantitative evaluation of ED ultrasound use to measure the extent of any disparity in use attributable to arrival time. We hypothesized that patients who present to EDs on evenings and weekends would undergo ultrasound examination at a lower rate compared with similar patients who present during regular business hours, and that this difference would persist even among patients with conditions for which ultrasound is strongly indicated.
METHODS
Study Design
This cross-sectional study explores the relationship between ED arrival time and ultrasound use using the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS is an annual cross-sectional survey of ED visits in the United States (U.S.) The survey, conducted by the National Center for Health Statistics, is a four-stage probability sample survey of visits to general and short-stay hospitals, excluding federal, military and Veterans Affairs hospitals. A detailed description of the NHAMCS methodology is available from the National Center for Health Statistics.19 We conducted the study with the publicly available dataset from NCHS; it was exempt from review by the University of California, San Francisco Human Subjects Committee.
Study Sample
To examine variation in ED ultrasound use, we used all patient data from the 2003–2005 NHAMCS ED surveys. We defined two a priori subgroups for secondary analyses: patients with increased risk of deep venous thrombosis (DVT), and patients with increased risk of ectopic pregnancy. We identified patients at increased risk of DVT as those who presented with a primary or secondary complaint (using reason for visit classification – RVC) of unilateral leg swelling (1920.5). We defined patients at increased risk of ectopic pregnancy as those who presented with either primary or secondary complaint of pain during pregnancy (RVC – 1790.1), or spotting/bleeding during pregnancy (RVC – 1709.2). Because many patients are unaware they are pregnant upon arrival to an ED, we also defined patients at increased risk of ectopic pregnancy as those who had International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9) codes at discharge for threatened abortion/hemorrhage in early pregnancy (640), or unspecified complications of pregnancy (646.8, 646.9).
Outcome Variable
The primary outcome variable was the use of diagnostic ultrasound during the ED visit. NHAMCS ultrasound use is based on medical record documentation, and not billing information. (Service Record: 1-53842273: communication with Center for Disease Control ambulatory and hospital statistics division). Use thus included both studies performed by the department of radiology as well as those performed by a non-radiologist (i.e. emergency physician or obstetrics/gynecologist).
Predictor Variables
The primary predictor variable was arrival time to the ED. Arrival time was divided into “regular hours” defined as Monday through Friday 7am to 7 pm, and “off hours” defined as Monday through Friday nights 7 pm to 7 am and weekends.
We obtained secondary predictors from predefined NHAMCS variables, including patient characteristics and hospital characteristics. Patient characteristics included both demographics (age, sex, race/ethnicity, method of payment), and clinical data (triage score, triage vital signs, triage pain score). Hospital characteristics included region, hospital ownership type, and Standard Metropolitan Statistical Area (SMSA). Region (Northeast, Midwest, South, and West), and SMSA categories represent standardized geographic divisions defined by the U.S. Census Bureau.19
Data Analysis
We used the weights, strata, and primary sampling unit design variables provided by NHAMCS for all analyses. Due to the large sample size, we included all potential predictors in the survey multivariate logistic regression models. To test the regression model, we used a goodness-of-fit test for survey data, analogous to the Hosmer-Lemeshow statistic for independent data. All odds ratios are presented with 95% confidence intervals. We performed all analyses using STATA statistical software (Version 10, StataCorp LP, College Station, Texas). P values less than 0.05 were considered statistically significant.
RESULTS
During the three survey years (2003–2005), NHAMCS collected data on 110,447 encounters, representing an estimated 339 million national visits to EDs. Table 1 shows the overall patient and hospital characteristics of the study sample divided into “regular hours” and “off hours.” The distribution of “regular hours” and “off hours” visit characteristics is similar across all patient and hospital categories (Table 1). Additional summary data has been reported previously.20

In multivariable analysis (Table 2), presenting to the ED during “off hours” was associated with a lower rate of ultrasound use independent of other potential confounders (odds ratio [OR] 0.73, 95% confidence interval [CI]: 0.65 – 0.82, p < 0.001). All subcategories of “off hours” times were associated with a significant decrease in use compared with “regular hours” (Table 2). The goodness-of-fit test for survey data indicated acceptable fit (p = 0.29).
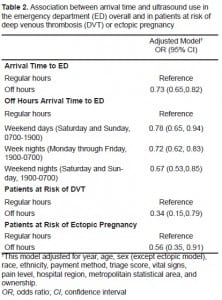
Table 2 also shows the association for “off hours” ultrasound use in our two subpopulations. For the population at increased risk of DVT, presenting to the ED during “off hours” yielded an adjusted odds ratio of undergoing an ultrasound of 0.34 (95% CI: 0.15 – 0.79, p = 0.012). For the population at increased risk of ectopic pregnancy, the adjusted odds of undergoing ultrasound during “off hours” was 0.56 (95% CI 0.35, 0.91, p = 0.02).
DISCUSSION
Our principal finding was that in U.S. EDs, the overall use of ultrasound was lower during “off hours” compared to “regular hours.” This finding persisted in subgroups at increased risk for DVT and ectopic pregnancy.
Ultrasound is critical to the evaluation of a wide variety of conditions managed in the ED and is considered the imaging modality of choice for DVT and ectopic pregnancy.21–26 Over the last two decades, expanding patient volume, downsizing of hospital capacity, and an increase in the number of uninsured patients have contributed to growing ED crowding.27–30 Holding patients overnight in the ED for ultrasound studies to be completed during regular hours of operation, a common practice, has become increasingly untenable. Rather than finding an increase in access to ultrasound services, a recent ED survey noted that there was a perception of a persistent lack of access to this technology.12 In fact, strategies are commonly used to work around the lack of ultrasound availability in “off hours,” such as initiating anticoagulant therapy for presumed DVT without an ultrasound diagnosis and discharging patients with suspected ectopic pregnancy prior to pelvic ultrasound.31 However, inappropriate therapy or delays in diagnosis can lead to substantial morbidity in both conditions.21, 31–37
Our results quantify the difference in use of diagnostic ultrasound by time of presentation in U.S. EDs. This type of disparity is likely to play a role in differential health outcomes based on patients’ time of presentation, although our findings cannot directly address this topic. While further study is required in the area of assessing the patient outcomes with regard to this disparity, the decision to obtain an ultrasound should not depend on the time of day or day of the week that the patient arrives in the ED.
LIMITATIONS
NHAMCS offers limited clinical details about each patient encounter. As a result, we were unable to evaluate whether the use of ultrasound was appropriate based on patient presentation. Thus, it is possible that our overall results reflect over-use of ultrasound during “regular hours.” To address this concern, we analyzed two a priori subgroups that more likely presented with a problem for which ultrasound is strongly indicated in the evaluation. Among these subgroups, the association persists. Although this subgroup approach could lead to misclassification bias, such misclassification would almost certainly be non-differential, which would bias the results towards the null.
CONCLUSION
Our results support the hypothesis that there is a difference in the use of diagnostic ultrasound based on time and day of presentation and this disparity may play a role in differential health outcomes. In practice settings where access to diagnostic ultrasound services is limited, increased training and placement of ED physicians who are credentialed in the use of limited ultrasonography may help to address this disparity.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted: January 27, 2010; Revision received April 6, 2010; Accepted April 19, 2010.
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: John Stein, MD, Department of Emergency Medicine, University of California, San Francisco, 505 Parnassus Ave., San Francisco, CA 94143
Email jstein@medicine.ucsf.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–8. [PubMed]
2. Cram P, Hillis SL, Barnett M, et al. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151–7. [PubMed]
3. Saposnik G, Baibergenova A, Bayer N, et al. Weekends: a dangerous time for having a stroke?Stroke. 2007;38:1211–5. [PubMed]
4. Ensminger SA, Morales IJ, Peters SG, et al. The hospital mortality of patients admitted to the ICU on weekends. Chest. 2004;126:1292–8. [PubMed]
5. Shaheen AA, Kaplan GG, Myers RP. Weekend versus weekday admission and mortality from gastrointestinal hemorrhage caused by peptic ulcer disease. Clin Gastroenterol Hepatol. 2008
6. Kostis WJ, Demissie K, Marcella SW, et al. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099–109. [PubMed]
7. Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117:175–81. [PubMed]
8. Arias Y, Taylor DS, Marcin JP. Association between evening admissions and higher mortality rates in the pediatric intensive care unit. Pediatrics. 2004;113:530–4. [PubMed]
9. Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294:803–12. [PubMed]
10. American College of Emergency Physicians: Council Resolution on Ultrasound. ACEP News. Nov, 1990.
11. Use of ultrasound by emergency physicians. Ann Emerg Med. 2001;38:469–70. [PubMed]
12. Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–53. [PubMed]
13. Tandy TK, Hoffenberg S. Emergency department ultrasound services by emergency physicians: model for gaining hospital approval. Ann Emerg Med. 1997;29:367–74. [PubMed]
14. Schlager D, Whitten D, Tolan K. Emergency department ultrasound: impact on ED stay times. Am J Emerg Med. 1997;15:216–7. [PubMed]
15. Schlager D, Lazzareschi G, Whitten D, et al. A prospective study of ultrasonography in the ED by emergency physicians. Am J Emerg Med. 1994;12:185–9. [PubMed]
16. Medicine ACoE Use of Ultrasound Imaging by Emergency Physicians. 2001.
17. Heller M, Crocco T, Patterson J, et al. Emergency ultrasound services as perceived by directors of radiology and emergency departments. Am J Emerg Med. 1995;13:430–1. [PubMed]
18. Saketkhoo DD, Bhargavan M, Sunshine JH, et al. Emergency department image interpretation services at private community hospitals. Radiology. 2004;231:190–7. [PubMed]
19. NHAMCS description US Centers for Disease Control and Prevention Web site. Available at:http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm. Accessed June 5, 2009.
20. Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007:1–32. [PubMed]
21. Clinical policy: critical issues in the evaluation and management of adult patients presenting with suspected lower-extremity deep venous thrombosis. Ann Emerg Med. 2003;42:124–35. [PubMed]
22. Tay JI, Moore J, Walker JJ. Ectopic pregnancy. BMJ. 2000;320:916–9. [PMC free article][PubMed]
23. Dialani V, Levine D. Ectopic pregnancy: a review. Ultrasound Q. 2004;20:105–17. [PubMed]
24. Kirk E, Papageorghiou AT, Condous G, et al. The diagnostic effectiveness of an initial transvaginal scan in detecting ectopic pregnancy. Hum Reprod. 2007;22:2824–8. [PubMed]
25. Kaplan BC, Dart RG, Moskos M, et al. Ectopic pregnancy: prospective study with improved diagnostic accuracy. Ann Emerg Med. 1996;28:10–7. [PubMed]
26. Nama V, Manyonda I. Tubal ectopic pregnancy: diagnosis and management. Arch Gynecol Obstet. 2009;279:443–53. [PubMed]
27. Hospital-Based Emergency Care: At the Breaking Point. National Academies Press. 2006
28. Kellermann AL. Crisis in the emergency department. N Engl J Med. 2006;355:1300–3. [PubMed]
29. Olshaker JS, Rathlev NK. Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the Emergency Department. J Emerg Med. 2006;30:351–6. [PubMed]
30. Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity.Ann Emerg Med. 2002;39:430–2. [PubMed]
31. Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007;35:S126–30. [PubMed]
32. Qaseem A, Snow V, Barry P, et al. Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians. Ann Intern Med. 2007;146:454–8. [PubMed]
33. Clinical policy for the initial approach to patients presenting with a chief complaint of vaginal bleeding. American College of Emergency Physicians. Ann Emerg Med. 1997;29:435–58. [PubMed]
34. Clinical policy: critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann Emerg Med. 2003;41:123–33. [PubMed]
35. Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009;361:379–87. [PubMed]
36. Abbott J, Emmans LS, Lowenstein SR. Ectopic pregnancy: ten common pitfalls in diagnosis. Am J Emerg Med. 1990;8:515–22. [PubMed]
37. Dalen JE. Pulmonary embolism: what have we learned since Virchow? Natural history, pathophysiology, and diagnosis. Chest. 2002;122:1440–56. [PubMed]


