| Author | Affiliation |
|---|---|
| John C. Sakles, MD | University of Arizona College of Medicine, Department of Emergency Medicine |
| John M. Deacon, MD | University of California, Davis School of Medicine, Department of Emergency Medicine |
| Aaron E. Bair, MD, MSc | University of California, Davis School of Medicine, Department of Emergency Medicine |
| Samuel M. Keim, MD, MS | University of Arizona College of Medicine, Department of Emergency Medicine |
| Edward A. Panacek, MD, MPH | University of California, Davis School of Medicine, Department of Emergency Medicine |
ABSTRACT
Introduction:
Airway management is a critical procedure performed frequently in emergency departments (EDs). Previous studies have evaluated the complications associated with this procedure but have focused only on the immediate complications. The purpose of this study is to determine the incidence and nature of delayed complications of tracheal intubation performed in the ED at an academic center where intubations are performed by emergency physicians (EPs).
Methods:
All tracheal intubations performed in the ED over a one-year period were identified; 540 tracheal intubations were performed during the study period. Of these, 523 charts (96.9%) were available for review and were retrospectively examined. Using a structured datasheet, delayed complications occurring within seven days of intubation were abstracted from the medical record. Charts were scrutinized for the following complications: acute myocardial infarction (MI), stroke, airway trauma from the intubation, and new respiratory infections. An additional 30 consecutive intubations were examined for the same complications in a prospective arm over a 29-day period.
Results:
The overall success rate for tracheal intubation in the entire study group was 99.3% (549/553). Three patients who could not be orally intubated underwent emergent cricothyrotomy. Thus, the airway was successfully secured in 99.8% (552/553) of the patients requiring intubation. One patient, a seven-month-old infant, had unanticipated subglottic stenosis and could not be intubated by the emergency medicine attending or the anesthesiology attending. The patient was mask ventilated and was transported to the operating room for an emergent tracheotomy. Thirty-four patients (6.2% [95% CI 4.3 – 8.5%]) developed a new respiratory infection within seven days of intubation. Only 18 patients (3.3% [95% CI 1.9 – 5.1%]) had evidence of a new respiratory infection within 48 hours, indicating possible aspiration pneumonia secondary to airway management. Three patients (0.5% [95% CI 0.1 – 1.6%]) suffered an acute MI, but none appeared to be related to the intubation. One patient was having an acute MI at the time of intubation and the other two patients had MIs more than 24 hours after the intubation. No patient suffered a stroke (0% [95% CI 0 – 0.6%]). No patients suffered any serious airway trauma such as a laryngeal or vocal cord injury.
Conclusion:
Emergency tracheal intubation in the ED is associated with an extremely high success rate and a very low rate of delayed complications. Complication rates identified in this study compare favorably to reports of emergency intubations in other hospital settings. Tracheal intubation can safely be performed by trained EPs.
INTRODUCTION
Tracheal intubation is a critical, often lifesaving, procedure performed frequently in emergency departments (EDs) across the world. Due to the often critical condition that patients requiring intubation present with, the nature and incidence of potential complications is important to consider. Several studies have reported immediate complications associated with ED intubations.1–4 These studies, with the exception of rare case reports, have focused only on complications apparent during the ED visit. In the same teaching hospital ED, we previously reported a series of 610 consecutive intubations that occurred over a one-year period to determine the type and incidence of immediate complications.5 We found an immediate complication rate of 8.0%, most of which were minor. Tayal et al.6 also studied intubations in an emergency medicine (EM) training program and found an immediate complication rate of 3.4%. Immediate complications that have been consistently identified include esophageal intubation, mainstem bronchus intubation, aspiration, oxygen desaturation and hypotension. Unfortunately, emergency airway management potentially can result in very serious complications that are not immediately apparent or recognized in the ED. For example, significant cardiac, neurological and respiratory complications may occur but may not become evident until several days later in the intensive care unit (ICU).7–10 The objective of this study is to determine the incidence and nature of delayed complications of tracheal intubation performed in the ED of a teaching hospital where intubations are performed by emergency physicians (EPs).
METHODS
Study Design
This was a one-year retrospective study of all intubated ED patients with an accompanying prospective 30 consecutive intubation cohort study. All patients intubated were eligible for enrollment. Structured data forms were cross-referenced to professional billing services to ensure a 100% capture rate. In the retrospective arm, all patients intubated in the ED during the academic year from July 01, 1997 to June 30, 1998 were included in the study and for the prospective arm all patients intubated in the one month period from January 03, 1999 to January 31, 1999 were included.
Study Setting
The University of California, Davis, Medical Center is an urban Level 1 Trauma Center with an annual ED census of approximately 60,000 patients. The ED is staffed full-time with EM residents and attending physicians. Approximately 30% of all patients arrive by ground ambulance or aeromedical transport. About 300 patients per year arrive by ambulance already intubated. These patients were not included in the study unless they required reintubation in the ED. The overall acuity of patients is high; 28% presenting to the ED are admitted to the hospital. Roughly half of all ED intubations are performed on patients with medical disorders and half on patients with trauma. Nearly all of these intubations are conducted by EM residents supervised by EM faculty. All intubations are entered into an airway registry with standardized data entry.
Airway management at the institution is the ultimate responsibility of the attending EP, who determines which resident will perform the intubation and what technique is used. The senior resident (third year post-graduate resident) usually manages all the trauma intubations and the most difficult medical airways. Routine medical intubations are typically managed by the second-year resident, and occasionally by the first-year resident. Rarely, medical students and residents from other specialties intubate patients under the direct supervision of the attending physician.
Airway equipment includes conventional straight and curved blade laryngoscopes. A cart with additional airway equipment is available for difficult airways; however, this study was performed before the introduction of videolaryngoscopes. The majority of patients in need of intubation undergo rapid sequence intubation (RSI). If they are considered a difficult airway, they undergo awake intubation without the use of a paralytic agent. Succinylcholine, vecuronium, and rocuronium are the immediately available neuromuscular blocking agents for RSI. Etomidate, midazolam and ketamine are the readily available sedative-hypnotic agents. For all intubations, patients are placed on a cardiac monitor, an automated non-invasive blood pressure monitor and a pulse oximeter. Patients are routinely preoxygenated prior to intubation attempts. Bag-valve mask ventilation is avoided before intubation unless necessitated by hypoxemia or inadequate ventilation. All patients undergoing oral intubation have cricoid pressure applied to prevent passive regurgitation and minimize gastric distension. All patients with blunt trauma are intubated with cervical spine in-line cervical stabilization maintained throughout the procedure. Tracheal intubation is confirmed by colorimetric end-tidal carbon dioxide detection in patients with a pulse. An aspiration syringe esophageal detector device is also used if the patient is in cardiac arrest. Auscultation of the chest is performed and a chest radiograph is obtained after intubation to determine the position of the tip of the endotracheal tube.
Residents receive a structured curriculum on airway management. The technique of surgical cricothyrotomy is also taught, and all EM interns attend a procedure lab and perform cricothyrotomies on cadavers under the supervision of an attending physician. The intern does a mandatory one-month rotation in anesthesia during the first year and performs approximately 50 intubations on stable patients in the operating room. During the second year, residents expand upon their airway experience by performing intubations in the ED, in the ICU, and in the prehospital setting during their EMS rotation. During their last year, each senior resident performs an average of 40 difficult intubations on trauma patients and unstable medical patients.
Data Collection and Analysis
A structured data collection form was developed prior to the collection of both retrospective and prospective data. It was first pilot tested and refined prior to use in the study. Information collected included demographic data, past medical history, prior history of RSI in the previous six months, and the induction agent used (if any).
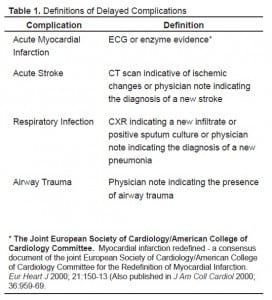
Delayed complications were pre-determined to fall into four major categories: cardiac, neurologic, respiratory and airway. An attempt was made to identify patients that suffered from an acute myocardial infarction, an acute stroke, aspiration pneumonia or upper airway trauma. Complications that occurred within seven days of intubation were considered potentially related to the intubation. Complications that occurred within two days of intubation were considered as possibly related. All medical records, including radiology reports, culture results, and progress notes were reviewed to seek evidence of complications. The time of onset of an infection was determined by when the earliest sign of infection became apparent. Definitions for each of the variables that could have subjective interpretation were prospectively developed and are summarized in Table 1. All data collection was by a single abstractor, with quality review of selected charts by the senior author.
For the retrospective portion of the study, all patients intubated in the ED from July 01, 1997 to June 30, 1998 were identified by using the airway registry database of patients at our institution and the database from the professional billing service. For the prospective portion of the study, all patients intubated in the ED from January 03–31, 1999 were identified within 24 hours of intubation. These patients were then prospectively followed as inpatients for seven days to identify any complications. All aspects of the medical record were reviewed including initial demographic data, past medical history, past steroid use history, peri-intubation vital signs, medication use and potential complications. If the patient was discharged prior to seven days, the medical record was obtained to evaluate for any further visits within the seven-day period. Data from the prospective arm of the study was used to validate the complication model created from the retrospective arm.
Summary descriptive statistics were performed. For selected complication rates, 95% confidence intervals were performed using Stata statistical software (Release 6, Stata Corporation, 1999). This study was approved by the University of California, Davis Institutional Review Board (IRB).
RESULTS
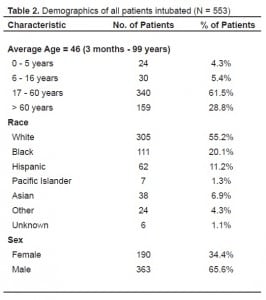
During the retrospective study period, 540 tracheal intubations were performed in the ED. Of these, 523 (96.9%), were included in the study. The medical record could not be obtained for the remaining 17. For the prospective arm of the study, 30 intubations were identified and had data collection forms completed. The total number of intubations with data forms in both the retrospective and prospective groups is 553 (entire study group). Table 2 summarizes the demographics of the study patients.
The overall success rate for ED endotracheal intubation was 99.8%. Only one patient (0.02%) could not be successfully intubated. This patient was a seven-month-old infant with subglottic stenosis. He was mask ventilated and went to the operating room for an emergent tracheostomy. Three other patients required surgical management of the airway by cricothyrotomy in the ED. All were successful. Eighty patients (14.5%) were intubated without the use of sedative-hypnotic agents, 453 patients (81.9%) received etomidate, 10 patients (1.8%) were induced with midazolam, one (0.2%) with lorazepam, one (0.2%) with fentanyl, five (0.9%) with ketamine, and in three (0.5%) the induction agent is unknown.
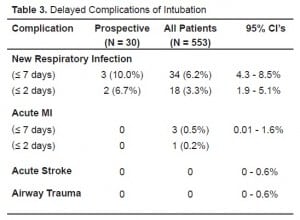
Table 3 summarizes the long-term complications for the entire study group. Thirty-four patients (6.2%) developed a new respiratory infection within seven days of intubation and determined to be potentially related to the intubation. This does not include patients who were admitted with a diagnosis of pneumonia. In the prospective group, three patients (10%) developed a new respiratory infection. Eighteen patients (3.3%) for the entire study group and two (6.7%) for the prospective group developed respiratory infections that became apparent within forty-eight hours possibly related to the ED intubation. For the entire study group, no patient suffered a cerebrovascular accident, but three patients (0.5%) suffered an acute myocardial infarction within seven days of intubation. None of these patients was in the prospective group. Only one patient ruled in for a myocardial infarction within 48 hours of intubation without cardiac symptoms closely antecedent to the intubation. No patient had evidence of major airway trauma (defined as a traumatic injury to the pharynx, larynx, vocal cords or trachea).
DISCUSSION
Several large prospective studies have reported their rates of successful intubation and acute complications with ED intubation.5,11 These studies have concluded that RSI in the hands of trained EPs is a safe and effective procedure with a low rate of immediate complications. EP rates of complications compare favorably to those done by anesthesiologists or critical care medicine attendings.12,13 This study confirms that endotracheal intubation by EPs is a highly successful procedure. Only one patient (0.2%) experienced failed airway management in the ED.
Prior studies, with the exception of scattered case reports, have not examined the rate of long-term or non-immediate complications from ED intubations by EPs.3,7–10,14,15 We found that long-term complications, as defined as occurring within seven days, are also uncommon. This study found a low incidence of new respiratory infections within the first seven days (6.2%). The rate of new respiratory infections occurring within 48 hours and more likely to be intubation related (aspiration) was only 3.3%. Our results are also similar to another study of emergent intubations outside the operating room.2 In that study of 297 patients intubated in an ICU, 12 (4%) were felt to have probably suffered an aspiration during airway management.
Three of our study patients suffered myocardial infarctions within seven days of intubation, but none were felt to be associated with the intubation. One patient was likely having an infarct at the time of intubation. He expired within 24 hours of intubation. One patient was intubated secondary to severe blunt trauma. His infarction occurred five days after intubation and is likely unrelated. The last patient had a myocardial infarction between 24 and 48 hours of intubation. His electrocardiogram did not become ischemic until more than 24 hours after intubation. Therefore, this is also unlikely to be secondary to intubation. No cases of major airway trauma were found in either the retrospective or prospective arms of the study.
LIMITATIONS
One study limitation is that the majority of data is obtained from a retrospective review of registry data and is dependent upon the quality of registry data entry and also medical chart documentation. It is possible that not all long-term complications were recorded in the progress notes or discharge summary, or that some were missed by the data abstractor. For these reasons, a prospective arm of the study was included to try for a validation of the rate of complications. The rate and pattern of complications were very similar in both arms of the study. This supports the validity of the larger retrospective data set. Another limitation is that these data are 10 years old. However, emergency airway management practices, with the exception of the recent use of videolaryngoscopes, have changed little over the last decade. Most patients still undergo direct laryngoscopy in the ED and receive the commonly used RSI drugs succinylcholine and etomidate.
CONCLUSION
In summary, we found that tracheal intubation was performed in our ED with an extremely high success rate and is associated with a very low rate of long-term complications. These rates compare favorably to reports of emergency intubations in other settings. This further supports the safety of rapid sequence intubation, and emergent tracheal intubation by EPs.
Footnotes
Supervising Section Editor: Tareg Bey, MD
Submission history: Submitted December 6, 2007; Revision Received September 1, 2008; Accepted September 12, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: John C. Sakles, MD. PO Box 245057, Department of Emergency Medicine, University of Arizona, USA
Email: sakles@aemrc.arizona.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Talucci RC, Shaikh KA, Schwab CW. Rapid sequence induction with oral endotracheal intubation in the multiply injured patient. Am Surgeon. 1988;54:185–187. [PubMed]
2. Schwartz DE, Matthay MA, Cohen NH. Death and other complications of emergency airway management in critically ill adults. A prospective investigation of 297 tracheal intubations. Anesthesiology. 1995;82:367–376. [PubMed]
3. Ooi GC, Irwin MG, Lam LK, Cheng SW. An unusual complication of emergency tracheal intubation. Anaesthesia. 1997;52:154–158. [PubMed]
4. Slobodkin D, Topliff S, Raife JH. Retrograde intubation of the pharynx: an unusual complication of emergency cricothyrotomy. Ann Emerg Med. 1992;21:220–222.[PubMed]
5. Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med.1998;31:325–332. [PubMed]
6. Taryle DA, Chandler JE, Good JT, Jr, Potts DE, Sahn SA. Emergency room intubations–complications and survival. Chest. 1979;75:541–543. [PubMed]
7. Fan CM, Ko PC, Tsai KC, Chiang WC, Chang YC, Chen WJ, Yuan A. Tracheal rupture complicating emergent endotracheal intubation. Am J Emerg Med. 2004;22:289–293.[PubMed]
8. Besmer I, Schupfer G, Stulz P, John M. [Tracheal rupture: delayed diagnosis with endobronchial intubation] Anaesthesist. 2001;50:167–170. [PubMed]
9. Miller JS, Itani KM, Oza MD, Wall MJ. Gastric rupture with tension pneumoperitoneum: a complication of difficult endotracheal intubation. Ann Emerg Med. 1997;30:343–346.[PubMed]
10. Gray B, Huggins NJ, Hirsch N. An unusual complication of tracheal intubation.Anaesthesia. 1990;45:558–560. [PubMed]
11. Tayal VS, Riggs RW, Marx JA, Tomaszewski CA, Schneider RE. Rapid-sequence intubation at an emergency medicine residency: success rate and adverse events during a two-year period. Acad Emerg Med. 1999;6:31–37. [PubMed]
12. Ma OJ, Bentley B, II, Debehnke DJ. Airway management practices in emergency medicine residencies. Am J Emerg Med. 1995;13:501–504. [PubMed]
13. Kovacs G, Law JA, Ross J, Tallon J, MacQuarrie K, Petrie D, Campbell S, Soder C. Acute airway management in the emergency department by non-anesthesiologists. Can J Anaesth. 2004;51:174–180. [PubMed]
14. Harris R, Joseph A. Acute tracheal rupture related to endotracheal intubation: case report. J Emerg Med. 2000;18:35–39. [PubMed]
15. Moschini V, Losappio S, Dabrowska D, Iorno V. Tracheal rupture after tracheal intubation: effectiveness of conservative treatment. Minerva Anestesiol. 2006;72:1007–1012. [PubMed]