| Author | Affiliation |
|---|---|
| Kurt R. Denninghoff, MD | University of Arizona, Department of Emergency Medicine University of Alabama at Birmingham, Injury Control Research Center |
| Mervin J. Griffin, MD | University of Alabama at Birmingham, Injury Control Research Center |
| Alfred A. Bartolucci, PhD | University of Alabama at Birmingham, School of Public Health University of Alabama at Birmingham, Injury Control Research Center |
| Steven G. LoBello, PhD | University of Alabama at Birmingham, Injury Control Research Center Auburn University Montgomery, AL |
| Phillip R. Fine, PhD | University of Alabama at Birmingham, School of Public Health University of Alabama at Birmingham, Injury Control Research Center |
ABSTRACT
Introduction:
To determine the relationship between emergent intubation (emergency department and field intubation cases combined) and mortality in patients with traumatic brain injury while controlling for injury severity.
Methods:
Retrospective observational study of 981 (35.2% intubated, 64.8% not intubated) patients with TBI evaluating the association between intubation status and mortality. Logistic regression was used to analyze the data. Injury severity measures included Head/Neck Abbreviated Injury Scale (H-AIS), systolic blood pressure, type of head injury (blunt vs. penetrating), and a propensity score combining the effects of several other potential confounding variables. Age was also included in the model.
Results:
The simple association of emergent endotracheal intubation with death had an odds ratio (OR) of 14.3 (95% CI = 9.4–21.9). The logistic regression model including relevant covariates and a propensity score that adjusted for injury severity and age yielded an OR of 5.9 (95% CI = 3.2–10.9).
Conclusion:
This study indicates that emergent intubation is associated with increased risk of death after controlling for a number of injury severity indicators. We discuss the need for optimal paramedic training, and an understanding of the factors that guide patient selection and the decision to intubate in the field.
INTRODUCTION
Aggressive emergent airway management for traumatic brain injury (TBI) has become a mainstay of most prehospital emergency management system (EMS) protocols. The rationale for emergent intubation is to establish an airway and prevent secondary brain injury. Despite the widespread adoption of endotracheal intubation for head-injured patients, there is little evidence from research demonstrating its lifesaving value in prehospital care. Although numerous studies show an increase in mortality associated with prehospital intubation,1–4 some have shown an associated decrease in mortality.5Considerable efforts have been made to determine if the observed association between prehospital intubation and mortality is real, or an apparent association caused by confounding variables.
There are a number of possible explanations for the excess mortality among head-injured patients who receive prehospital intubation. The decision or ability to intubate in the field may be markers of injury severity that are currently not accounted for in the usual list of potential confounders.6 Other intrinsic physiologic variables could make intubation detrimental for some patients, or perhaps intubation is being performed on individuals who do not meet the current criteria for intubation. Misplaced endotracheal tubes may be detrimental to patients, and inadequate training or experience in intubation among paramedics has also been recognized as a problem that could contribute to mortality.1,3,7–9 In one well-developed prehospital system, there was a 13% rate of unsuccessful intubation.8 One study of field intubation reported as many as 25% of tubes are misplaced when protocols for verification of tube placement are not followed carefully.10
The use of neuromuscular blockade in the field could ease some of the difficulty in placing endotracheal tubes and reduce tube misplacements.11–13 Several studies of neuromuscular blockade (NMB) assisted intubation in some aero-medical and ground EMS services suggest greater intubation success rates in patients where NMB is employed.11,13–15 Bulger et al.16 have demonstrated that NMB is associated with increased survival and improved outcomes among TBI cases. However, the use of NMB agents in the field has been criticized elsewhere, and data in support of the protocol’s effectiveness in decreasing mortality risk are regarded as inconclusive.17–19
Hyperventilation is another factor related to increased mortality among field-intubated patients with TBI. Although hyperventilation decreases intracranial pressure by cerebral vasoconstriction, the practice also may diminish cerebral blood flow to ischemic levels.20Ghajar21 notes that decreased mortality and improved outcomes are the result of practices such as increasing cerebral perfusion, which would reduce the impact of secondary injury. Chestnutt22 also provides an extensive review of the problem of secondary brain injury
Enumeration of the many possible causes of the relationship between field intubation and mortality is beyond the scope of this paper. Many studies have focused on improving field practice with the ultimate aim of reducing mortality. The present study is a retrospective observational study of the association of emergent intubation and mortality while controlling for a range of potential confounding variables associated with injury severity. We hypothesized that the excess of mortality among emergently intubated cases would be effectively eliminated when accounting for injury severity.
METHODS
Study Design, Setting and Data Collection
Data for this study were obtained from the University of Alabama Birmingham Injury Control Research Center (UAB-ICRC) as an ongoing, prospective, longitudinal study of persons with various injuries including cohort with traumatic brain injury (TBI). Medical record information was abstracted for all individuals admitted to any of eight participating hospitals in the central and northern Alabama area with TBI. From this database of potential participants, those who met the inclusion criteria were asked to participate in the longitudinal study. Criteria for inclusion in this study were: a) having sustained TBI between 1989 and 1992, b) residing and having been injured in Alabama, c) being at least 18 years of age when injured, and d) participating in regularly scheduled telephone follow-up interviews conducted by UAB-ICRC personnel.
Participants: Selection and Characteristics
All data used in this intubation outcome study were found and recorded during the initial hospital record abstraction performed during the recruitment period from 1989 to 1992. Missing data are not the result of longitudinal follow-up loss. The study base began with the 1,204 persons with TBI. Case identification was based on ICD-9 codes for skull fracture or intracranial injury (ICD-9 codes 800–803 and 851–854). Missing values on some variables (Head/Neck Abbreviated Injury Scale [n= 19], mortality status [n=31], and propensity score [n= 173]) caused the loss of 223 participants in the analysis of the relationship between intubation status and mortality. To determine if the remaining cohort of 981 participants was biased by the loss of these participants, we compared this group to the original sample of 1,204 on the outcome variable (death). All variables included in the logistic regression model are summarized in Table 2. There were no significant differences in the distributions of any of these variables between the original sample of 1,204 and theTBI. Although remaining cohort of 981 participants. The two groups also did not differ in the distribution of mortality outcome or gender.

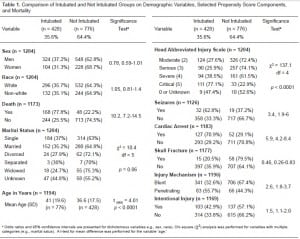
Table 1 presents the demographic characteristics for this initial sample. Missing values accounted for the loss of some participants in the initial cohort, and Table 1 indicates the number of participants with valid data for each variable. Intubated cases were older, more seriously injured, and were more likely to have had a penetrating injury. The remaining variables associated with intubation status are components of the propensity score discussed below. Mortality outcome was known for 1,173 participants, and 216 (18.4%) died before hospital discharge.
Methods of Measurement
Each participant was assessed on the Head/Neck Abbreviated Injury Scale (H-AIS), with scores ranging from 1 (minor) to 6 (unsurvivable).23–24 There were no cases of minor injury (H-AIS=1) or unsurvivable injury (H-AIS=6) in the database. Nineteen cases with H-AIS coded as missing were excluded from the primary analysis. Therefore, the effective range of H-AIS for this study was 2 (Moderate) to 5 (Critical). Mortality events were counted if death occurred before the time of regular discharge from the hospital.
Intubation status was collected from hospital admission records, but the abstract summary does not distinguish between field and emergency department intubations. Paramedics in Alabama at the time of the study did not then, and do not now, use neuromuscular blocking agents to permit intubation of difficult cases. Participants who were not at any time intubated during prehospital or emergency department care made up the ‘not intubated’ group (N= 636, 64.8%). This group also included any cases that were intubated following hospital admission because the intubation occurred outside the time frame under consideration. There were 345 (35.2%) intubated cases in the database. No data were collected on other less common forms of intubation, such as a temporary surgical airway.
Statistical Power
Power analysis calculations indicated that a logistic regression with a sample size of 981 achieves power of .91 at an alpha level of .05. This corresponds to an odds ratio (OR) of 1.7 for the association between intubation and death.
RESULTS
A simple bivariate analysis examining the relationship of intubation and mortality showed that the odds of dying before hospital discharge for those who were intubated were 14 times higher than the odds for those who were not intubated (OR = 14.3, 95% CI = 9.4–21.9). The next step was to determine if factors related to injury severity and age would eliminate this association. We constructed a multivariate logistic regression model to determine the impact of potential confounders on the association between intubation and mortality. The variables included in the model were H-AIS score (range =2–5), injury type (blunt vs. penetrating), systolic blood pressure (categorical), endotracheal intubation status, and a propensity score. These variables were chosen because they are frequently included in similar studies, were available in the database, and are known correlates of mortality.
We controlled for multiple potential confounding variables by the use of propensity scores.2 Propensity scores are estimates of the conditional probability of receiving the treatment (intubation) given its relationship to potential confounding variables. The variables included in the creation of the propensity scores were selected because of their potential relationship to intubation status and mortality, as well as their relative completeness in the data set. The propensity score was developed using logistic regression with endotracheal intubation status as the outcome variable. The variables included in the propensity score model were race (white vs. nonwhite), intentionality (intentional vs. unintentional injury), alcohol use at the time of injury (present vs. absent), seizure activity (present vs. absent), skull fracture (present vs. absent), and cardiac arrest (present vs. absent). Five variables included in the propensity score were significantly related to endotracheal intubation status in the multivariate analysis and were retained in the calculation of the propensity scores. Intentional injury (OR = 1.9, 95% CI = 1.3 – 2.7), seizure activity (OR = 3.9, 95% CI = 2.0 – 7.5), and cardiac arrest (OR = 8.4, 95% CI = 5.5 –12.8) were associated with an increased likelihood of intubation. Skull fracture (OR = 0.3, 95% CI = 0.18 – 0.68) was associated with a decreased likelihood of intubation.
Table 2 summarizes the results of the logistic regression model where the inclusion of covariates and the propensity score affects a downward adjustment on the risk of death associated with intubation as compared to the crude odds ratio. However, contrary to the hypothesis, the risk of death associated with intubation is not eliminated. The risk of death was almost six times greater for the intubated TBI patient (OR = 5.9, 95% CI =3.2–10.9). Significant covariates in the model include age, injury severity, systolic blood pressure, and the propensity score. Blunt trauma was associated with decreased mortality compared to penetrating injury. Greater age, lower systolic blood pressure (between 61–100 mm Hg), and H-AIS = 5 (critical) were all associated with greater mortality.
DISCUSSION
We began with a simple odds ratio of 14.3 between intubation status and mortality. In a multivariate model adjusted for injury severity, the association drops to an almost six times increase in mortality among intubated patients. Clearly, accounting for a broad range of injury severity factors reduces, but does not eliminate, the mortality risk associated with intubation. Because many studies that control for the same injury severity factors have achieved similar results, the possibility that the results are due to inadequate statistical control of injury severity factors is unlikely. Before considering factors that may account for the association between emergent intubation and mortality, the relationship between mortality and H-AIS score deserves comment. In this study, the proportionate odds of death indicate that the critically injured group (H-AIS =5) accounted for most of the effect. There was no difference in risk of death among those with lesser degrees of injury (H-AIS = 2, 3, 4), but the odds of death were 19 times greater for the critically injured intubated cases than for those who were not intubated. The H-AIS alone obviously would not have provided adequate control for the effects of increasing injury severity in this model and did not optimally stratify the mortality risk of patients with TBI.
Batchelor et al.24 indicated that it is not yet possible to determine which of several systems developed after the H-AIS is superior because of limitations in current methods used to assess goodness-of-fit (eg, Hosmer-Lemeshow statistic). Nevertheless, trauma-scoring models such as International Classification of Diseases Injury Severity Score (ICISS) have shown promise, especially when combined with age and other trauma measures. Although much work remains in the classification of trauma and prediction of outcomes, it is also clear that the field is advancing beyond the H-AIS and Injury Severity Score (ISS) models. Better systems are available, but it will take time for registries to change over to these systems and to develop sufficient numbers of cases for analysis.
The lack of a neuromuscular blockade protocol for ground emergency medical technicians (EMTs) or emergency physicians in Alabama during the recruitment phase of this study means that every intubated case, regardless of H-AIS, would have had a blunted gag reflex, itself an indicator of serious injury. Those who were intubated in the moderate, serious, and severe injury groups were probably more seriously injured than the H-AIS suggests. Mortality increased only slightly among the injury severity groups until a dramatic increase was observed for the critically injured group. Similar patterns of the relationship of H-AIS and mortality have been reported elsewhere.23,25
Even if the H-AIS were a better predictor of mortality, it could not inform paramedic practice because it is determined long after the initial presentation observed by the EMT in the field. Further, along with Wang et al.2 and others, our study relied on the ICD-9 code to include patients. This information is also unavailable to the paramedic in the field. Unless all patients who meet criteria for intubation based on field observations, and not just those with ICD-9 codes consistent with TBI, are found to have increased morbidity and mortality when intubated emergently, it will remain difficult for the EMS community to significantly change practices based on these results, however compelling.
Returning to other factors that may account for the increased mortality among intubated cases, it is suggested that factors prompting a decision to intubate should be included in future studies. The guidelines for intubation, as well as the observations and evaluations of the emergency responder, should be carefully studied as a means of improving criteria useful in rapidly assessing the need for intubation. A framework for understanding the cognitive processing demands on paramedics confronting potential intubation cases has been proposed.26 Their model highlights the complex host of interacting variables that enter into the decision to intubate. Algorithms that standardize and inform practices are essential in approaching relatively uncomplicated cases, but probably would not extend to ambiguous cases that send conflicting signals to the paramedic about the advisability of intubation.27
Interest in cognitive processes indicates a shift in research emphasis away from post-intubation factors that affect mortality (i.e., injury severity) and toward pre-intubation factors that influence the decision to intubate at the scene. A small focus group study of paramedics indicated that paramedics view intubation as a key component of their professional identity, suggesting that it is a highly valued professional activity.28 Thus, paramedics who place a high value on intubation may be more likely to intubate hopeless and unsalvageable cases. The emergency responder who encounters very seriously injured cases recognizes that many will die regardless of treatment. Under these circumstances, there is a very low risk of further harm while there may be a very large potential benefit if an airway is established and the person survives. There is no comparable set of circumstances at the lower end of the injury severity spectrum, so the most seriously injured, and perhaps a very large proportion of the mortally injured, would receive endotracheal intubation. Bulger et al.16 reported that 95% of the severe TBI cases in their study were intubated, a proportion high enough to contain more than a few cases beyond rescue. The key to understanding the relationship between intubation and mortality is in the appearance of the case to the emergency responder at the time the decision to intubate is made. Despite the large number of studies that have been conducted, calls for the restriction or elimination of field intubation seem premature given that research into on-the-scene decision-making processes is beginning to emerge.29
LIMITATIONS
This study has the drawbacks of a retrospective study on an existing dataset and cannot be used to imply causality. Our data set only confirms emergent intubation status by the time of hospital admission. An unknown number of these cases occurred in the field, and some undoubtedly occurred in the ED. We do not have the ability to extract the site of intubation, the number of attempts, the body habitus of the patient or more detail about the causes of morbidity or mortality from the database. Because data were collected from multiple hospitals, a retrospective review of the charts from as many as 17 years ago at all of these hospitals is prohibitive. Moreover, these data were collected in Alabama where rapid sequence intubation (RSI) protocols are not in use by ground EMT services. The most recent research shows that in 2004–2005, less than 12% of Alabama EMTs licensed to perform intubation actually did so during the year. Of the almost 1400 intubations performed in the field, about 92% required more than one attempt.30 Thus, current intubation success rates in Alabama are low, and it is difficult to imagine that field performance was any better when our data were collected.
Several investigators have reported that hyperventilation is a significant contributor to increased mortality noted in patients with TBI who are intubated. Because prehospital and the ED patients in our database were all hyperventilated by protocol this remains an important potential confounder in our data set. Patients intubated in the field are still hyperventilated at least 70% of the time, even though it is no longer part of the regular treatment protocol.31
CONCLUSION
Results of this study indicate that emergent intubation is associated with an increased risk of death even after controlling for potential confounders related to injury severity. Future research that combines factors that influence patient selection with injury severity measures will more adequately determine the degree of relationship between emergent intubation and mortality. The effectiveness of field and emergent intubation should ultimately determine if this practice continues to have a place in the paramedic armamentarium.
Footnotes
This study was supported in part by Grant No. R49-CE000191 from the US Department of Health and Human Services Centers for Disease Control and Prevention, National Center for Injury Prevention and Control to the University of Alabama at Birmingham, Injury Control Research Center.
Supervising Section Editor: Tareg Bey, MD
Submission history: Submitted November 13, 2007; Revision Received May 13, 2008; Accepted May 23, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Kurt R. Denninghoff, MD., Department of Emergency Medicine, University of Arizona School of Medicine, 1501 N. Campbell Avenue, P.O. Box 245057, Tucson, AZ 85724-5057
Email: kdenninghoff@aemrc.arizona.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Davis DP, Peay J, Sise MJ, et al. The impact of prehospital endotracheal intubation on outcome in moderate to severe traumatic brain injury. J Trauma. 2005;58:933–939.[PubMed]
2. Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain. Ann Emerg Med.2004;44:439–450. [PubMed]
3. Bocchichio GV, Ilahi O, Joshi M, Bocchichio K, Scalia TM. Endotracheal intubation in the field does not improve outcome in trauma patients who present without an acutely lethal traumatic brain injury. J Trauma. 2003;54:307–311. [PubMed]
4. Arbabi S, Jurkovich GJ, Wahl WL, et al. A comparison of prehospital and hospital data in trauma patients . J Trauma. 2004;56:1029–1032. [PubMed]
5. Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Arch Surg. 1997;132:592–597. [PubMed]
6. Floccare DJ, Cushman JT. Endotracheal intubation in the field: Pro position. Hosp Med.2005;66:89–91. [PubMed]
7. Wang HE, Lave JR, Sirio CA, Yealy DM. Paramedic intubation errors: Isolated events or symptoms of a larger problem? . Health Affairs. 2006;25:501–509. [PubMed]
8. Wang HE, Kupas DF, Paris PM, Bates RR, Costantino JP, Yealy DM. Multivariate predictors of failed prehospital intubation. Acad Emerg Med. 2003;10:717–724.[PubMed]
9. Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emeg Med.2005;45:497–503.
10. Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emeg Med. 2001;37:32–37.
11. Murray JA, Demetriades D, Berne TV, et al. Prehospital intubation in patients with severe head injury. J Trauma. 2000;49:1065–1070. [PubMed]
12. Silverstone P. Pulse oximetry at the roadside: A study of pulse oximetry in immediate care. Br Med J. 1989;298:711–13. [PMC free article] [PubMed]
13. Sloane C, Vilke GM, Chan TC, et al. Rapid sequence intubation in the field versus hospital in trauma patients. J Emerg Med. 2000;19:443–444.
14. Cooper A, Discala C, Foltin G. Pre-hospital endotracheal intubation for severe head injury in children: A reappraisal. Sem Pediatr Surg. 2001;10:3–6.
15. Bulger EM, Copass MK, Maier RV, Larsen J, Knowles J, Jurkovich GJ. An analysis of advanced prehospital airway management. J Emerg Med. 2002;23:183–89. [PubMed]
16. Bulger EM, Copass MK, Sabath D, Maier RV, Jurkovich GJ. The use of Neuromuscular Blocking Agents to Facilitate Prehospital Intubation does not Impair Outcome following Traumatic Brain Injury. J Trauma. 2005;58:718–24. [PubMed]
17. Wang HE, Yealy DM. Out-of-hospital rapid sequence intubation: Is this the “success” we envisioned? . Ann Emerg Med. 2002;40:168–171. [PubMed]
18. Wang HE, Davis DP, O’Connor RE, Domeier RM. Drug-assisted intubation in the prehospital setting (Resource document to the NAEMSP position statement) Prehosp Emerg Care. 2006;10:261–271. [PubMed]
19. Davis DP. Prehospital intubation of brain-injured patients. Curr Opin Crit Care.2008;14:142–148. [PubMed]
20. Stocchetti N, Maas AIR, Chieregato A, van der Plas AA. Hyperventilation in head injury: A review. Chest. 2005;127:1812–1827. [PubMed]
21. Ghajar J. Traumatic brain injury. The Lancet. 2000;256:923–929.
22. Chestnut RM. Care of Central Nervous System Injuries. Surg Clin North Am.2007;87:119–156. [PubMed]
23. Demetriades D, Kuncir E, Murray J, Velmahos GC, Rhee P, Chan L. Mortality prediction of Head Abbreviated Injury Score and Glasgow Coma Scale: Analysis of 7,764 head injuries. J Am Coll Surg. 2004;199:216–222. [PubMed]
24. Batchelor JS, McGuinness A, Ryan J. Adult trauma scoring systems: A critical review.Trauma. 2001;3:175–180.
25. Gennarelli TA, Champion HR, Copes WS, Sacco WJ. Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J Trauma. 1994;37:962–968. [PubMed]
26. Wang HE, Katz S. Cognitive control and prehospital endotracheal intubation. Prehosp Emerg Care. 2007;11:234–239. [PubMed]
27. Wang HE, Kupas DF, Greenwood MJ, Pinchalk ME, Mullins T, Gluckman W, Sweeney TA, Hostler D. An algorithmic approach to prehospital airway management. Prehosp Emerg Care. 2005;9:145–155. [PubMed]
28. Thomas JB, Abo BN, Wang HE. Paramedic perceptions of challenges in out-of-hospital endotracheal intubation. Prehosp Emerg Care. 2007;11:219–223. [PubMed]
29. Zink BJ, Maio RF. Out-of-hospital endotracheal intubation in traumatic brain injury: Outcomes research provides us with an unexpected outcome. Ann Emeg Med.2004;44:451–453.
30. Stephens SW, Brown TB. Field intubation by out-of-hospital rescuers: The Alabama experience. Acad Emerg Med. 2006;13(Suppl 1):S85.
31. Warner KJ, Bulger EM. Does pre-hospital ventilation effect outcome after significant brain injury? . Trauma. 2007;9:283–289.


