| Author | Affiliation |
|---|---|
| Jonathan Walker, DO | York Hospital, Department of Emergency Medicine, York, PA |
| Michael Galuska, MD | York Hospital, Department of Emergency Medicine, York, PA |
| David Vega, MD | York Hospital, Department of Emergency Medicine, York, PA |
ABSTRACT
Introduction:
Cardiac stress tests for diagnosis of coronary artery disease (CAD) are incompletely sensitive and specific. We examined the frequency of significant CAD in patients presenting to the emergency department (ED) with chest pain who have had a recent negative or inconclusive (<85% of predicted maximum heart rate) cardiac stress test.
Methods:
This was a retrospective chart review of patients identified from ED and cardiology registries at the study hospital. We included patients presenting to the ED with a chief complaint of chest pain, with a negative cardiac stress test in the past three years as the last cardiac test, and hospital admission. One-hundred sixty-four patients met the inclusion criteria. Their admission was reviewed for diagnosis of CAD by positive serum troponin, percutaneous coronary intervention, or positive stress test while an inpatient.
Results:
Of 164 patients, 122(74.4%, 95% CI 67.7, 81.1) had a negative stress test prior to the index admission, while 42 (25.6%, 95% CI 18.9, 32.3) had otherwise normal but inconclusive stress tests. Thirty-four (20.7%, 95% CI 14.4,27.0) of the included patients were determined to have CAD. Twenty-five of the 122 patients (20.5%, 95% CI 13.3, 27.7) had negative pre-admission stress tests and nine of 42 patients (21.4%, 95% CI 9.0, 33.8) had inclusive stress tests of CAD. A statistical comparison between these two proportions showed no significant difference (p = .973).
Conclusion:
Due to inadequate sensitivity, negative non-invasive cardiac stress tests should not be used to rule out CAD. Patients with negative stress tests are just as likely to have CAD as patients with inconclusive stress tests.
INTRODUCTION
In 2007 the Centers for Disease Control and Prevention (CDC) reported chest pain as the second most common reason for emergency department (ED) visits (5%) in the United States (U.S.). Almost six million patients presented to the ED in 2005 complaining of chest pain.1 The CDC also reports that heart disease accounted for over four million admissions to U.S. hospitals in 2005.2
It can be difficult to determine whether or not a patient with chest pain needs hospital admission. Greater accuracy in identifying chest pain patients who can be safely discharged home might help to reduce hospital and ED crowding. Unfortunately, discharging chest pain patients carries risk. One large multicenter study by Pope found that 2.1% of acute myocardial infarctions (AMI) were mistakenly discharged home from the ED, as were another 2.3% of patients with proven unstable angina (USA).3
Disposition decisions can be more difficult in patients with a recent negative cardiac stress test. Cardiac stress tests for diagnosing coronary artery disease (CAD) range in sensitivity from 67% to 85% and specificity from 70% to 95% depending on the study referenced and the type of stress test performed.4 This sensitivity and specificity may not be sufficient to make disposition decisions on patients presenting to the ED with chest pain.
A few recent studies have further examined this clinical dilemma. Nerenberg et al found no difference between ED admission rates and 30-day cardiovascular event rates in patients with and without a prior normal stress test. Also, while patients with a prior abnormal stress test were admitted more frequently, there was no statistically significant difference in adverse outcomes among patients with a previous abnormal stress test, a previous normal stress test, or no previous stress test.5 Smith et al studied the incidence of AMI, defined by an elevated troponin in patients presenting to the ED within three years after a documented normal stress test with subsequent admission and found that 4.8% of the patients had an AMI.6
The purpose of this study was to examine the frequency with which significant CAD is found in patients presenting to the ED with chest pain who have had a negative cardiac stress test within three years.
METHODS
This was an IRB-approved retrospective chart review of patients presenting to the ED with a chief complaint of chest pain and a negative cardiac stress test in the three years preceding presentation. This timeframe was chosen because consensus opinion of cardiologists at our institution viewed older stress test results as unreliable. We reviewed charts for adverse cardiac events in the 30 days after ED presentation as described below.
This study was conducted at a community teaching hospital with an ED census of 70,610 visits in 2007. Of these visits, 5,591 (7.9%, 95% CI 7.7, 8.1) were for chest pain. Of the 19,501 patients admitted from the ED in 2007, 17.5% (95% CI 17.0, 18.0) were for patients > 18 years who presented with a chief complaint of chest pain. From August 2005 through February 2008 (31 months), 2910 stress tests were performed locally. There was a single large cardiology group in our region, allowing data capture from all locally-performed stress tests (both in our hospital and outside the institution). The negative stress tests performed on the 164 patients included in the study represent 5.6% of the total stress tests performed. Included patients could have had a positive stress test at an outside institution, but this was felt unlikely because of the long distance to the nearest outside facilities that perform stress tests.
We used the hospital’s cardiology registry, which began in August 2005, to obtain a list of patients to evaluate for inclusion. The database only recorded patients who had stress echocardiograms (both treadmill and pharmaceutical). No database for electrocardiogram (ECG)-only stress tests or nuclear stress tests was available. The stress test recorded in the study, however, was the most recent study on record, so some nuclear stress tests and ECG-only studies were included if the patients from the cardiology database had one of these types of stress tests closer to the ED encounter. For patients who had multiple past stress tests, we also collected data on the most recent stress test. Thus, for all patients in the study, only results from the most recent stress test on record prior to admission were used for analysis.
We then used an ED patient registry to obtain a second database of patients who were > 18 years old and presented to the ED during this same time frame with a recorded chief complaint of “chest pain,” “CP,” “chest tightness,” or “chest pressure,” and the patient was admitted to the hospital. If one of these patients presented multiple times during the time period with the above chief complaints, each visit was counted as a separate encounter, as each visit would represent the same disposition dilemma to the emergency physician.
The stress test database and ED database were then compared to identify study patients. We found that 337 patients >18 years old who presented to the ED with chest pain had undergone a stress test (regardless of result) prior to their ED visit and were admitted.
Each of the patient encounters in the final database underwent a thorough chart review by a single reviewer (MG). Patients were excluded if their most recent stress test within three years was positive, or if they had cardiac catheterization or coronary artery bypass grafting (CABG) between the stress test and their ED visit.
A positive stress test was defined as any positive individual aspect of the test, as reported by the interpreting cardiologist. This included clinically positive studies with chest pain, as well as ischemic changes on ECG, echocardiogram, or nuclear imaging. Official stress test reports provided at our institution include a summary statement of the cardiologist’s interpretation of the test. Tests were considered positive for the purposes of this study if the cardiologist interpretation included a description of possible ischemic changes or other evidence of CAD. All other stress tests results were considered negative. Of note, those stress tests that did not meet any of the positive criteria but were considered inconclusive because they did not reach the 85% maximum heart rate target were included in the negative group, and analyzed as a separate subgroup.
For our patients, the type of stress test performed, the time between stress test and admission, and evidence of CAD within 30 days of admission were recorded using a standardized data collection sheet. We defined significant CAD within 30 days as a myocardial infarction identified by positive cardiac markers, subsequent positive stress test of any type, cardiac catheterization requiring intervention (angioplasty or medical management but no stent placed as reported on catherization report), CABG, or death due to medical cardiac arrest.
RESULTS
We reviewed 337 patient encounters; 173 patients were excluded due to positive stress test (111 patients), history of another previous positive cardiac stress test within three years of admission, or interval cardiac catheterization or CABG (62 patients). The remaining 164 met all inclusion criteria. The mean age was 55 years old (range of 27–93; SD 15). There were 82 males. Of the 164 patients included, 122 (74.4%, 95% CI 67.7, 81.1) had a prior negative stress test and the remaining 42 (25.6%, 95% CI 18.9,32.3, ±6.68%) had a prior inconclusive stress test. Table 1 provides a summary of this data.
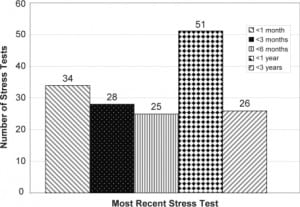
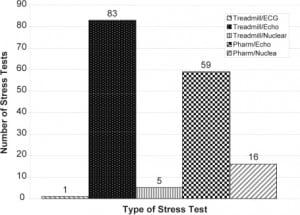
The distribution of time between the most recent stress test and ED visit is shown in Figure 1. The majority of patients had a treadmill echocardiogram as their most recent stress test (83 patients, 50.6%, 95% CI 43.0, 58.3). Other types of stress tests included pharmacologic echocardiograms (59 patients, 35.9%, 95% CI 28.6, 43.2), pharmacologic nuclear studies (16 patients, 9.8%, 95% CI 5.3, 14.4), treadmill nuclear studies (5 patients, 3.0%, 95% CI 0.4, 5.6), and a treadmill ECG only study (1 patient, 0.6%, 95% CI −0.6, 1.8). [Figure 2]
Of the 164 patients, 34 (20.7%, 95% CI 14.4, 27.0) had significant CAD within 30 days of admission. Twenty-five (20.5%, 95% CI 13.3, 27.7) of the 122 s who had a negative stress test had CAD, while nine (21.4%, 95% CI 14.1, 28.7) of 42 who had an inconclusive stress test had CAD.
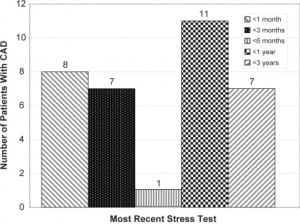
When examining the time between the most recent stress test and hospital admission for patients who had significant CAD, and of the 34 patients who developed CAD, eight (23.5%, 95% CI 9.3, 37.8) had their most recent stress test within one month of admission. Seven were (20.6%, 95% CI 7.0, 34.2) between one and three months, one (2.9%, 95% CI −2.7, 8.5) between three and six months, 11 (32.4%, 95% CI 16.7, 48.1) between six months and one year, and seven (20.6%, 95% CI 7.0, 34.2) within one to three years. [Figure 3]
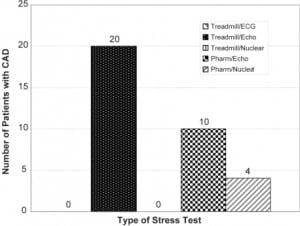
Of patients with significant CAD, 20 (58.5%, 95% CI 41.9, 75.1) had a treadmill echocardiogram as their most recent stress test, 10 (29.4%, 95% CI 14.1, 44.7) had a pharmacologic echocardiogram, and four (11.8%, 95% CI 1.0, 22.6) had a pharmacologic nuclear study. None had a treadmill nuclear or treadmill ECG only study. [Figure 4]
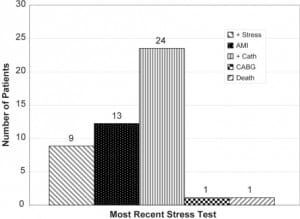
Of the 164 patients with negative stress test prior to admission, 24 (14.6%, 95% CI 9.2,20.0) had a heart catheterization in which an intervention was performed, 13 (7.9%, 95% CI 3.8,12.0) had an AMI, nine (5.5%, 95% CI 2.0,9.0) had a positive stress test, one (0.6%, 95% CI −0.6,1.8) had a CABG and one (0.6%, 95% CI −0.6,1.8) died [Figure 5]. Some patients had more than one indicator of CAD. Table 2 shows the different combinations of CAD indicators found in the 34 patients with CAD.
DISCUSSION
The disposition of patients presenting to the ED with the chief complaint of chest pain is complex. When no definitive diagnosis can be made, the decision to admit or discharge is often based on the physician’s level of suspicion of acute coronary syndrome (ACS). One study found that 2.1% of patients with AMI and 2.3% with USA were inappropriately discharged home.3 The goal of the emergency physician is to minimize the number of patients discharged home with ACS. At the same time, limited hospital resources may place pressure on physicians to minimize the number of patients admitted for possible ACS.
Cardiac stress testing is one modality used to screen patients for CAD. The goal of the stress test is to identify a fixed obstruction to coronary blood flow, such as in stable angina. However, in ACS including AMI and USA, the underlying pathophysiology is plaque rupture and thrombus formation. The lesion may not have been significant enough to be detected on stress testing.5 Therefore, the use of a negative stress test to determine the disposition of ED chest pain patients is questionable.
In our study, 20.7% of patients presenting to the ED with a negative stress test within three years of presentation still had significant CAD. A fraction of these were technically inconclusive based on not achieving 85% of the maximum predicted heart rate for age (25.6%). However, there was no difference between patients whose stress test was negative compared to those whose tests were negative but technically inconclusive based on heart rate (20.5% vs. 21.4% respectively).
Our results suggest that a negative stress test is unreliable in ruling out CAD. In a similar study, Smith found that 4.8% of patients presenting to the ED within three years after a normal stress test had an AMI.6 While there is some discrepancy between the total percentage of AMI found in Smith’s study and ours (4.8% versus 7.9%), both studies call into question the use of prior negative stress test results in ED disposition of patients with chest pain.
In a cohort study Nerenberg evaluated the disposition decisions of ED physicians on1,853 patients presented to the ED with chest pain, 291 of whom had a negative prior stress test. A previous negative stress test did not significantly change the rate of admission to the hospital. The study also measured secondary outcomes of 30-day cardiac events in both admitted and discharged patients. There was no significant difference in adverse events between patients who had a positive stress test, a negative stress test, or no previous stress test; 5.2% of the patients who had a previous negative stress test had an adverse cardiac event. The study defined adverse cardiac events in similar terms as our study, including AMI, catheterization requiring intervention, CABG, or death.4
The most likely explanation for the difference in 30-day adverse events between the Nerenberg study (5.2%) and ours (20.7%) is that their study included both admitted and discharged patients, while ours only included patients admitted from the ED. Patients discharged from the ED would be expected to have a lower occurrence of adverse events than those admitted. Thus, our study would be expected to find more patients with indicators of significant CAD. Also, both studies were performed with data from a single institution in different geographic and economic areas, which could indicate different subsets of the population with different prevalence of CAD. Ultimately, however, both studies find significant numbers of patients with previous negative stress testing who were found to have CAD.
LIMITATIONS
The design of the study as a retrospective chart review from a single institution has inherent limitations. Unique characteristics of our patient population or our institutional standards in decision-making may not make our findings applicable to other settings. Because of the retrospective nature of the study, only admitted patients could be assessed for adverse cardiac events, which likely introduces selection bias, as admitted patients would be expected to have a higher prevalence of CAD than those discharged home. Also, if a patient presented multiple times, we considered each visit separately. If the indicator of CAD was only found on the last visit, this could have slightly diluted the true frequency of CAD.
The relatively small sample size in our study produces additional limitations. We do not have enough samples in each group to determine statistically significant differences between the types of stress tests and between the various time frames from the most recent stress test and admission. It is possible that some types of stress tests may be better than others as a negative predictor of CAD. Likewise, the time between the last stress test and presentation to the ED could have a more significant role than our study would indicate. A much larger data sample is needed to detect significant differences in these subgroups.
Another limitation is that we used a positive stress test after admission as a marker of CAD. Since a positive stress test prior to admission was used as an exclusion criterion for the study, the use of a positive stress test as a marker of CAD after admission may be reasonable. However, it is possible that patients with a positive stress test after admission did not have CAD demonstrated by other means. A positive stress test, however, is almost always followed by further evaluation and possibly intervention.
We were limited by the data available. Our cardiology database of stress tests only dated back to August 2005 and only included exercise and pharmaceutical echocardiograms. This certainly reduced the number of included patient encounters in our study and may have been an unavoidable source of selection bias. Twenty-two of the 164 (13.4%) included patient encounters had a most recent stress test that was one other than a pharmaceutical or treadmill echocardiogram. Four of the 22 patients (18.8%) had CAD on admission (Figure 4), which is consistent with the overall incidence of the study. Therefore, it is uncertain how the results would be affected if more nuclear studies had been included.
Finally, abstractors were not blinded to the hypothesis of the study so we did not follow the guidelines set for by Worster et al.13
CONCLUSION
A previous negative stress test cannot be used alone to rule out CAD in patients presenting to the ED with chest pain. In this study, 20.7% of patients with negative stress tests within three years prior to presentation had significant CAD within 30 days of admission. Further studies are needed to determine the role that previous stress testing should play in determining the disposition of chest pain patients.
Footnotes
Supervising Section Editor: Shahram Lotfipour, MD, MPH
Submission history: Submitted July 10, 2009; Revision Received February 12, 2010; Accepted April 7, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jonathan Walker, DO, Department of Emergency Medicine, Phoenix Indian Medical Center, 2953 E. Melrose St, Gilbert, AZ, 85297
Email: walkerdo@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Nawar E, Niska R, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary Advance Data from Vital and Health Statistics. CDC. 2007.http://www.cdc.gov/nchs; Last accessed Jan 18, 2008.
2. DeFrances C, Hall M. National Hospital Discharge Survey Advance Data from Vital and Health Statistics. CDC. 2005. 2007. http://www.cdc.gov/nchs; Last accessed Jan 18, 2008.
3. Pope J, Aufderheide T, Ruthazer R, et al. Missed Diagnosis of Acute Cardiac Ischemia in the Emergency Department. N Engl J Med. 2000;342:1163–70. [PubMed]
4. Fletcher G, Balady G, Amsterdam E, et al. AHA Exercise Standards for Testing. Circulation.104:1694. 201: [PubMed]
5. Nerenberg R, Shofer F, Robey J, et al. Impact of a negative prior stress test on emergency physician disposition decision in ED patients with chest pain syndromes. Am J of Emerg Med.2007;25:39–44. [PubMed]
6. Smith S, Jackson E, Bart B, et al. Incidence of Myocardial Infarction in the Emergency Department Chest Pain Patients with a Recent Negative Stress Imaging Test. Acad Emerg Med. 2005;12(5)(suppl 1):51. pg:
7. Macaciel R, Mesquita E, Vivacqua R, et al. Safety, Feasibility, and Results of Exercise Testing for Stratifying Patients with Chest Pain in the Emergency Room. Arq Bras Cardiol. 2003;81:174–81.[PubMed]
8. Prina L. Outcome of Patients with a Final Diagnosis of Chest Pain of Undetermined Origin Admitted under the Suspicion of Acute Coronary Syndrome: A Report from the Rochester Epidemiology Project. Annals of Emerg Med. 2004 Jan;43(1):59–67.
9. Hollander J. Risk Stratification of Emergency Department Patients with Chest Pain: The Need for Standarized Reporting Guidelines. Annals of Emerg Med. 2004 Jan;43(1):68–70.
10. Conti A. Assessment of patients with low-risk chest pain in the emegerncy department: Head-to-head comparison of exercise stress echocardiography and exercise myocardial SPECT. Am Heart J.2005 May;149(5):894–901. [PubMed]
11. Kuo D. Emergency Cardiac Imaging: State of the Art. Cardiol Clin. 2006;24:53–65. [PubMed]
12. Bedetti G. Stress echo in chest pain unit: the SPEED trial. Inter J of Cardio. 2005;102:461–67.
13. Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448–51. [PubMed]


