| Author | Affiliation |
|---|---|
| Michael A. Yokell, ScB | Stanford University School of Medicine, Department of Emergency Medicine, Stanford, California |
| Carlos A. Camargo, MD | Massachusetts General Hospital, Department of Emergency Medicine, Boston, Massachusetts |
| N. Ewen Wang, MD | Stanford University School of Medicine, Department of Emergency Medicine, Stanford, California |
| M. Kit Delgado, MD, MS | University of Pennsylvania, Department of Emergency Medicine, Philadelphia, Pennsylvania |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Emergency department (ED) screening and counseling for alcohol misuse have been shown to reduce at-risk drinking. However, barriers to more widespread adoption of this service remain unclear.
Methods
We performed a secondary analysis of a nationwide survey of 277 EDs to determine the proportion of EDs that routinely perform alcohol screening and counseling among patients presenting with alcohol-related complaints and to identify potential institutional barriers and facilitators to routine screening and counseling. The survey was randomly mailed to 350 EDs sampled from the 2007 National Emergency Department Inventory (NEDI), with 80% of ED medical directors responding after receiving the mailing or follow-up fax/email. The survey asked about a variety of preventive services and ED directors’ opinions regarding perceived barriers to offering preventive services in their EDs.
Results
Overall, only 27% of all EDs and 22% of Level I/II trauma center EDs reported routinely screening and counseling patients presenting with drinking-related complaints. Rates of routine screening and counseling were similar across geographic areas, crowding status, and urban-rural status. EDs that performed routine screening and counseling often offered other preventive services, such as tobacco cessation (P<0.01) and primary care linkage (P=0.01). EDs with directors who expressed concern about increased financial costs to the ED, inadequate follow-up, and diversion of nurse/physician time all had lower rates of screening and counseling and also more frequently reported lacking the perceived capacity to perform routine counseling and screening. Among EDs that did not routinely perform alcohol screening and counseling, more crowded than non-crowded (P<0.01) and more metro than rural (P<0.01) EDs reported lacking the capacity to perform routine screening and counseling. The capacity to perform routine screening also decreased as ED visit volume increased (P=0.04).
Conclusion
To increase routine alcohol screening and counseling for patients presenting with alcohol-related complaints, ED directors’ perceived barriers related to an ED’s capacity to perform screening, such as limited financial and staff resources, should be addressed, as should directors’ concerns regarding the implementation of preventive health services in EDs. Uniform reimbursement methods should be used to increase ED compensation for performing this important and effective service.
INTRODUCTION
Alcohol misuse and abuse represent a major cause of morbidity, mortality, and healthcare costs in the United States (U.S.).1–3 Each year, there are approximately 2 million emergency department (ED) visits associated with alcohol.4 Annual alcohol-related visits to EDs may account for as many as 28.7 visits for every 1,000 people in the U.S. population.5 In one study in an urban setting, nearly one-quarter of all patients presenting to the ED were identified as dependent on alcohol through the use of brief screening tools.6
Emergency departments present a unique opportunity to address alcohol-related morbidity and mortality by identifying patients with at-risk drinking or alcohol dependence, performing a brief intervention, and referring appropriate patients to treatment. This process is referred to as SBIRT (screening and brief intervention, referral to treatment). Numerous studies have demonstrated the clinical efficacy of SBIRT for alcohol misuse. SBIRT has been shown to decrease ED utilization,7 alcohol consumption by participants,8–10 inpatient utilization,11 Medicaid costs,11 and arrest rates for driving under the influence (DUI),12 while simultaneously increasing rates of entry into formal chemical dependency programs.13 Since 2007, Level I and II trauma centers have been required by American College of Surgeons to screen for problem drinking, and Level I trauma centers must have mechanisms to provide intervention to appropriate patients.14 The American College of Emergency Physicians issued a policy statement in 2005 to support the use of alcohol screening and interventions in U.S. EDs.15
Two previous studies have surveyed EDs to determine the extent of SBIRT use in U.S. EDs.16,17 However, these studies have focused on Level I or Level I/II trauma centers, which are often also academic teaching hospitals. No efforts to date have documented the extent of SBIRT’s use among all levels of EDs in the U.S., nor has any study attempted to identify specific characteristics of EDs that may make them more or less likely to routinely screen for alcohol misuse.
We aimed to fill the current knowledge gap by examining ED factors associated with the routine use of alcohol screening and counseling and by identifying potentially modifiable barriers that could be addressed to increase the adoption of screening and counseling in U.S. EDs. We performed a secondary analysis on data collected in 2008–9 in a national survey of ED directors regarding preventive health services in EDs. We hypothesized that crowded (defined by criteria used by Centers for Disease Control and Prevention [CDC] researchers),18 publicly-owned, urban, and critical access hospitals (rural hospitals that are certified to receive Medicare cost-based reimbursement) would have higher rates of routine screening and counseling, since they are often safety-net hospitals most likely to see patients at high risk for alcohol-related complaints; however, since resources are generally limited in these settings, it has been unclear how the need for screening and scarcity of resources would be balanced. We also hypothesized that lower rates of screening and counseling would be reported by EDs whose directors cited barriers to the provision of preventive services in their EDs. Our research findings are particularly important for policy makers and ED directors seeking to implement or expand SBIRT in U.S. EDs, and for researchers who plan to perform ED SBIRT research, particularly in non-academic center EDs.
METHODS
Study Design
We performed a secondary analysis of data collected for a national survey of preventive services in U.S. EDs; the survey was conducted from September 2008 to April 2009. The local institutional review board approved all aspects of this study. The full methods of the survey have been previously described.19
Study Population
Briefly, we randomly selected 350 EDs from the 2007 National Emergency Department Inventory (NEDI-USA; developed and maintained by the Emergency Medicine Network),20 representing 7% of the 4,874 EDs in the inventory. The sample size was selected to attain a minimum sample of 5% of national EDs, assuming a 70% response rate. In total, 277 ED medical directors (80%) responded to the mail survey that was followed-up by email/fax, and there were no significant differences between responders and non-responders.19
Outcomes and Measurements
The cross-sectional analysis presented here examined potential factors associated with routine alcohol screening and counseling for patients presenting with drinking-related complaints in U.S. EDs; among EDs that did not routinely provide screening and counseling, we also examined factors associated with having the capacity to routinely perform screening and counseling. Our primary outcome of interest was the routine provision of alcohol screening and counseling for patients with drinking-related complaints and the secondary outcome was having the capacity to perform screening and counseling if not currently performed. We used a 2-part survey question to evaluate these outcomes: regarding “alcohol risk screening, counseling, and referral for all patients with drinking-related complaints,” (1) “is there a system in place that routinely performs this service in your ED?” (primary outcome) and (2) “if not, could you offer this service routinely with existing staff and funding?” (secondary outcome). Independent variables of interest included teaching hospital status, region, trauma level, urban influence code, volume, public ownership, crowding, and the director’s opinions regarding preventive services in EDs.
Urban-rural status (metropolitan, micropolitan, rural, frontier) was based on urban influence codes, which are a county-based measure of urban-rural status from the U.S. Department of Agriculture. We defined ED crowding by asking key surrogate questions for crowding, which have been used and validated by CDC researchers.18 Specifically, we asked about the average time from triage sign-in to being placed in an ED treatment bed, the percentage of registered patients who left without being seen by a clinician, and the percentage of time spent in ambulance diversion status.
Data Analysis
We generated tabulations and descriptive statistics using Stata 11.0 (StataCorp, College Station, TX). Chi-Square (χ2) tests were performed for discrete variables, with Fisher exact tests performed when sample or sub-sample sizes were small. We performed 2-sided t-tests for continuous variables. Two-sided p–values <0.05 were considered statistically significant.
RESULTS
Overall, 277 ED directors responded to the survey, representing a response rate of 80%. Respondents included ED directors from 46 states. A summary of respondent ED characteristics is presented in Table 1.
Table 1. Characteristics of 277 respondent emergency departments regarding routine alcohol screening.
| Characteristic | n (%) |
|---|---|
| Teaching hospital | 21 (8) |
| Region | |
| Northeast | 35 (13) |
| Midwest | 79 (29) |
| South | 113 (41) |
| West | 50 (18) |
| Crowded | 127 (46) |
| Trauma center | 53 (19) |
| Trauma level | |
| I | 22 (8) |
| II | 14 (5) |
| III | 17 (6) |
| Urban influence code | |
| Metropolitan | 159 (57) |
| Micropolitan | 66 (24) |
| Rural | 18 (7) |
| Frontier | 34 (12) |
| Critical access hospital* | 73 (26) |
| Volume | |
| Less than 10,000 | 87 (31) |
| 10,000–19,999 | 46 (17) |
| 20,000–39,999 | 84 (30) |
| 40,000 and greater | 60 (22) |
| Publicly owned hospital | 79 (29) |
| Routinely performs alcohol screening† | 75 (27) |
*Critical access hospital: Medicare designation as being a “necessary provider” of health care services and location greater than 35 miles from nearest hospital †for patients presenting with alcohol-related complaints
Characteristics of EDs performing and not performing routine alcohol screening and counseling are reported in Table 2. Seventy-five of the 277 respondents (27%, 95% confidence interval 22–32%) reported performing routine alcohol screening and counseling for patients presenting with alcohol-related complaints. Rates of screening and counseling were similar across geographic areas, crowding status, and urban-rural status. Among the 21 teaching hospitals, 7 (33%) performed routine screening and counseling versus 27% of non-teaching hospitals (P=0.5), and only 12 out of 53 (22%) Level I/II trauma centers performed routine screening and counseling. There was no statistical difference in screening rates of trauma centers vs. non-trauma centers, or among different levels of trauma care. EDs that offered tobacco cessation programs or primary care linkage reported significantly higher rates of routine alcohol screening and counseling.
Table 2. Characteristics of emergency departments performing and not performing routine alcohol screening.
| Characteristic | Performs routine alcohol screening | Does NOT perform routine alcohol screening | Total | p-value |
|---|---|---|---|---|
| n (%) | n (%) | n | ||
| Total | 75 (27) | 202 (73) | 277 | |
| Region | ||||
| Northeast | 10 (29) | 25 (71) | 35 | 0.99 |
| Midwest | 21 (27) | 58 (73) | 79 | |
| South | 30 (27) | 83 (74) | 113 | |
| West | 14 (28) | 36 (72) | 50 | |
| Crowded | ||||
| Yes | 34 (27) | 93 (73) | 127 | 0.92 |
| No | 41 (27) | 109 (73) | 150 | |
| Urban influence code | ||||
| Metropolitan | 45 (28) | 114 (72) | 159 | 0.84 |
| Micropolitan | 18 (27) | 48 (73) | 66 | |
| Rural | 5 (28) | 13 (72) | 18 | |
| Frontier | 7 (21) | 27 (79) | 34 | |
| Teaching hospital | ||||
| Teaching | 7 (33) | 14 (67) | 21 | 0.50 |
| Non-teaching | 68 (27) | 188 (73) | 256 | |
| Trauma level | ||||
| I or II | 8 (2) | 28 (78) | 36 | 0.48 |
| III or non-trauma center | 67 (28) | 174 (72) | 241 | |
| Trauma level | ||||
| I | 3 (14) | 19 (86) | 22 | 0.43 |
| II | 5 (36) | 9 (64) | 14 | |
| III | 4 (24) | 13 (77) | 17 | |
| Non-trauma center | 63 (28) | 161 (72) | 224 | |
| Offers tobacco cessation | ||||
| Yes | 25 (45) | 31 (55) | 56 | <0.01 |
| No | 50 (23) | 171 (77) | 221 | |
| Offers linkage to PCP | ||||
| Yes | 51 (34) | 99 (66) | 150 | 0.01 |
| No | 24 (19) | 103 (81) | 127 | |
| Critical access hospital | ||||
| Yes | 16 (22) | 57 (78) | 73 | 0.25 |
| No | 59 (29) | 145 (71) | 204 | |
| Volume | ||||
| Less than 10,000 | 19 (22) | 68 (78) | 87 | 0.19 |
| 10,000–19,999 | 18 (39) | 28 (61) | 46 | |
| 20,000–39,999 | 21 (25) | 63 (75) | 84 | |
| 40,000 and greater | 17 (28) | 43 (72) | 60 | |
| Percentage of uninsured patients† | ||||
| <5% | 1 (9) | 10 (91) | 11 | 0.61 |
| 5–14% | 19 (25) | 56 (75) | 75 | |
| 15–24% | 26 (29) | 63 (71) | 89 | |
| 25–34% | 15 (25) | 44 (75) | 59 | |
| >35% | 12 (33) | 24 (67) | 36 | |
| Publicly owned hospital | ||||
| Yes | 25 (32) | 54 (68) | 79 | 0.25 |
| No | 49 (25) | 148 (75) | 197 | |
| Social workers | ||||
| Yes | 59 (28) | 151 (72) | 210 | 0.5 |
| No | 16 (24) | 51 (76) | 67 | |
| Stratified: | ||||
| 0 hr/wk | 16 (24) | 51 (76) | 67 | 0.39 |
| 1–23 hr/wk | 42 (26) | 119 (74) | 161 | |
| 24 hr/wk | 17 (35) | 32 (65) | 49 |
PCP, primary care provider Percentages add across rows †Director’s estimate; n=270 for this variable only
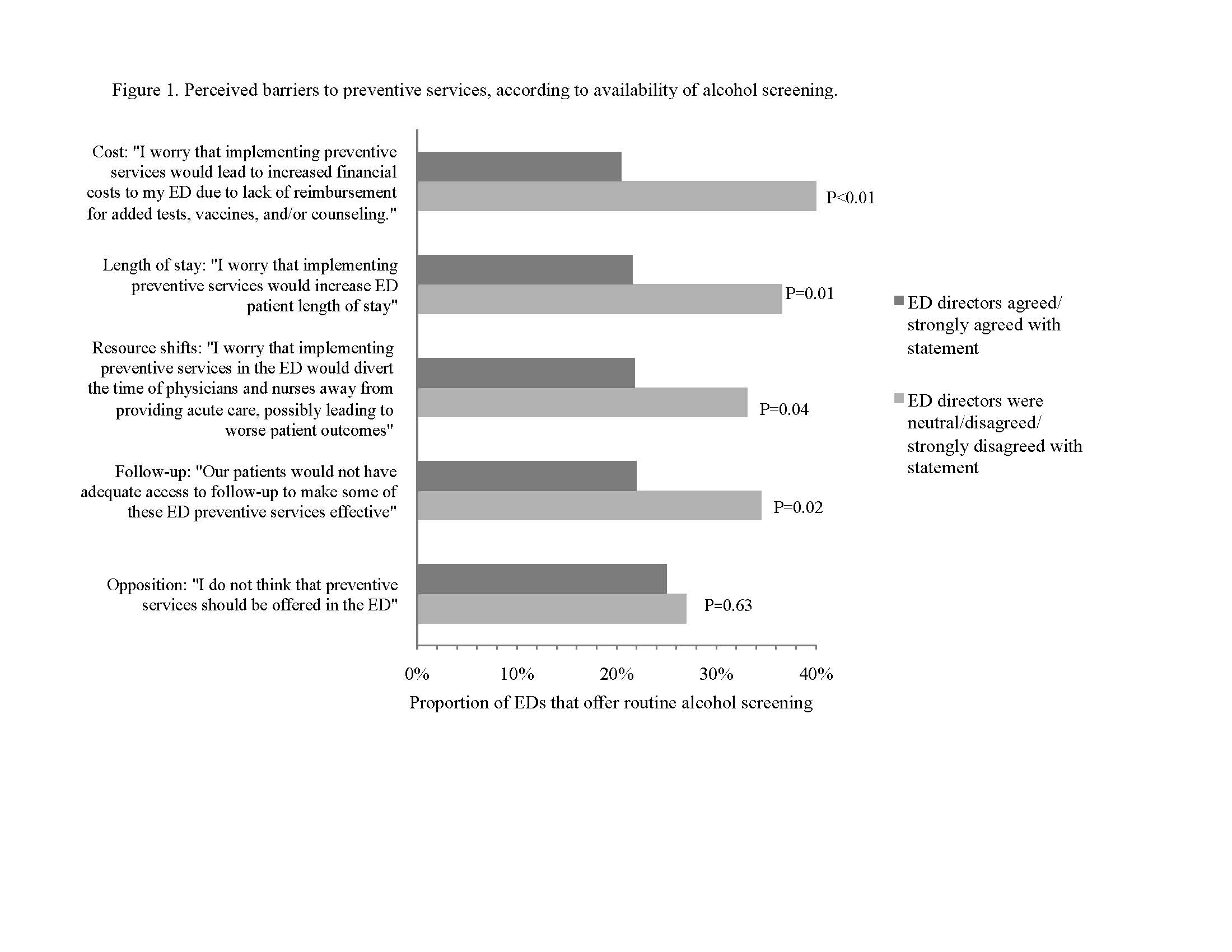
Directors’ concerns regarding preventive services were largely associated with not performing routine screening and counseling; EDs with directors who expressed concern about increased length of stay, increased financial costs to the ED, inadequate follow-up, and diversion of nurse/physician time all had lower rates of screening and counseling
.
Among respondents who reported not performing routine alcohol screening and counseling, we compared the characteristics of EDs with and without the reported capacity to perform routine screening and counseling (Table 3). Among EDs not routinely performing alcohol screening and counseling, more crowded EDs than non-crowded EDs (P<0.01) reported lacking the capacity to perform routine screening and counseling, as did more metro EDs than rural ones (P<0.01). The capacity to perform routine screening also decreased as volume increased (P=0.04 for trend). More private hospitals than public hospitals reported lacking the capacity to perform routine screening and counseling. A larger proportion of critical access hospitals reported having the capacity to perform routine screening and counseling in comparison to non-critical access hospitals.
Table 3. Characteristics of emergency departments (EDs) that have and do not have the capacity to perform routine alcohol screening*, n=202.
| Characteristic | Has capacity for alcohol screening | Lacks capacity for alcohol screening | Total | p-value |
|---|---|---|---|---|
| n (%) | n (%) | n | ||
| Total | 55 (27) | 147 (73) | 202 | |
| Region | ||||
| Northeast | 4 (16) | 21 (84) | 25 | 0.07 |
| Midwest | 23 (40) | 35 (60) | 58 | |
| South | 18 (22) | 65 (78) | 83 | |
| West | 10 (28) | 26 (72) | 36 | |
| Crowded | ||||
| Yes | 16 (17) | 77 (83) | 93 | <0.01 |
| No | 39 (36) | 70 (64) | 109 | |
| Urban influence code | ||||
| Metropolitan | 21 (18) | 93 (82) | 114 | <0.01 |
| Micropolitan | 15 (31) | 33 (69) | 48 | |
| Rural | 8 (62) | 5 (39) | 13 | |
| Frontier | 11 (41) | 16 (59) | 27 | |
| Teaching hospital | ||||
| Yes | 5 (36) | 9 (64) | 14 | 0.54 |
| No | 50 (27) | 138 (73) | 188 | |
| Trauma level I or II | ||||
| Yes | 9 (32) | 19 (68) | 28 | 0.53 |
| No | 46 (26) | 128 (74) | 174 | |
| Trauma level | ||||
| I | 6 (32) | 13 (68) | 19 | 0.89 |
| II | 3 (33) | 6 (67) | 9 | |
| III | 3 (23) | 10 (77) | 13 | |
| Non-trauma center | 43 (27) | 118 (73) | 161 | |
| Offers tobacco cessation | ||||
| Yes | 12 (39) | 19 (61) | 31 | 0.12 |
| No | 43 (25) | 128 (75) | 171 | |
| Capacity for tobacco cessation | ||||
| Yes | 33 (58) | 24 (42) | 57 | <0.01 |
| No | 22 (15) | 123 (85) | 145 | |
| Offers linkage to PCP | ||||
| Yes | 33 (33) | 66 (67) | 99 | 0.06 |
| No | 22 (21) | 81 (79) | 103 | |
| Critical access hospital | ||||
| Yes | 24 (42) | 33 (58) | 57 | <0.01 |
| No | 31 (21) | 114 (79) | 145 | |
| Volume | ||||
| Less than 10,000 | 27 (40) | 41 (60) | 68 | 0.04 |
| 10,000–19,999 | 7 (25) | 21 (75) | 28 | |
| 20,000–39,999 | 13 (21) | 50 (79) | 63 | |
| 40,000 and greater | 8 (19) | 35 (81) | 43 | |
| Percentage of uninsured patients‡ | ||||
| <5% | 5 (50) | 5 (50) | 10 | 0.29 |
| 5–14% | 11 (20) | 45 (80) | 56 | |
| 15–24% | 20 (32) | 43 (68) | 63 | |
| 25–34% | 11 (25) | 33 (75) | 44 | |
| >35% | 6 (25) | 18 (75) | 24 | |
| Publicly owned hospital | ||||
| Yes | 21 (39) | 33 (61) | 54 | 0.03 |
| No | 34 (23) | 114 (77) | 148 | |
| Social workers | ||||
| Yes | 14 (28) | 37 (73) | 51 | 0.97 |
| No | 41 (27) | 110 (73) | 151 | |
| Stratified: | ||||
| 0 hr/wk | 14 (28) | 37 (73) | 51 | 0.95 |
| 1–23 hr/wk | 33 (28) | 86 (72) | 119 | |
| 24 hr/wk | 8 (25) | 24 (75) | 32 |
PCP, primary care provider percentages add across rows *Table 3 only includes EDs that do not routinely perform alcohol screening for patients presenting with drinking-related complaints ‡Director’s estimate; n=197 for this variable only.
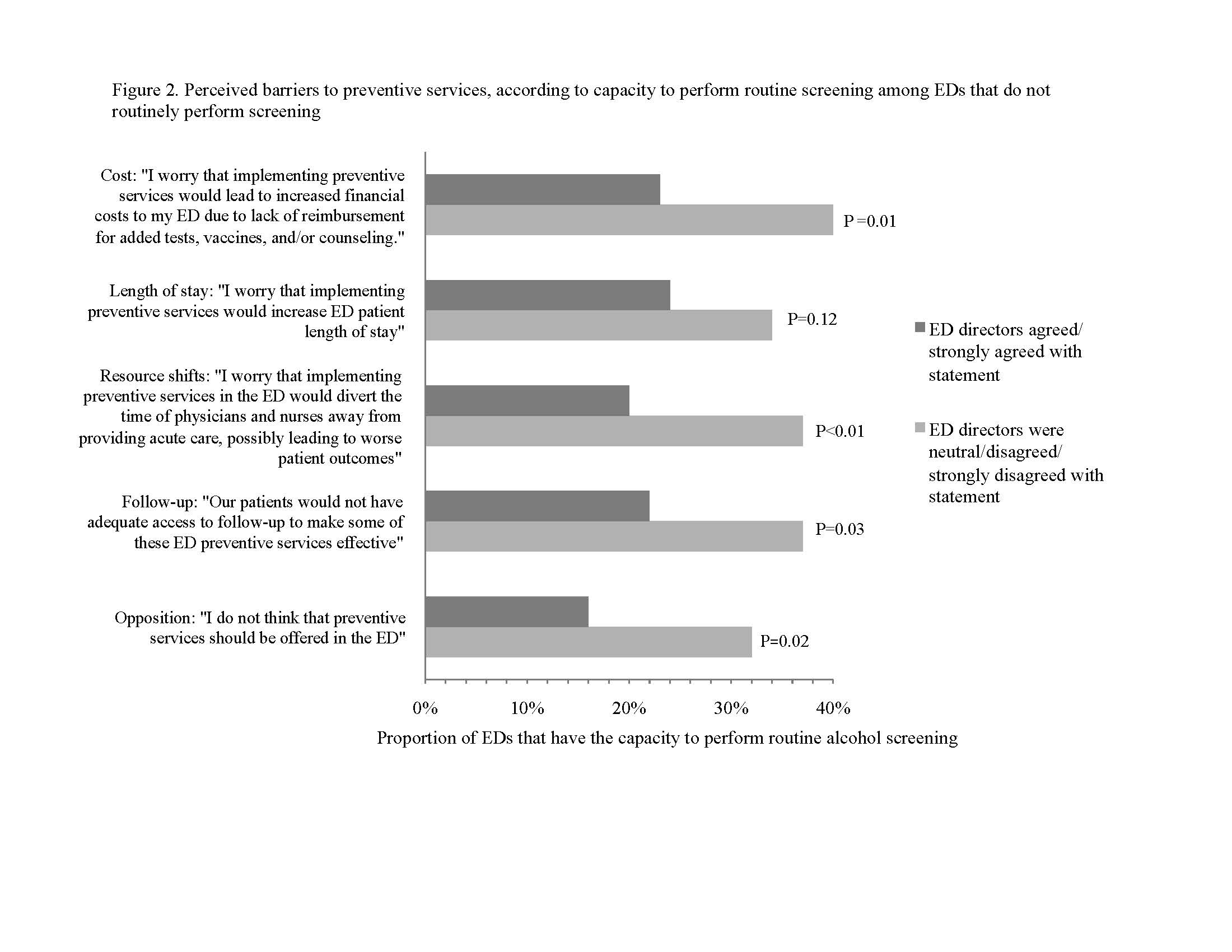
Additionally, many ED directors’ concerns regarding preventive services were associated with lacking the perceived capacity to perform screening and counseling, including concerns about increased financial costs to the ED, inadequate follow-up, and diversion of nurse/physician time. Also, among EDs whose directors thought that preventive services should not be offered in EDs, 84% reported lacking the capacity to perform routine screening, in comparison to 68% of EDs whose directors did not report that belief (P=0.02).
Figure 2
Perceived barriers to preventive services, according to capacity to perform routine screening among emergency departments (EDs) that do not routinely perform screening.
DISCUSSION
Availability of Routine Alcohol Screening and Counseling
Twenty-seven percent (27%) of all EDs in our sample and only 22% of Level I/II trauma center EDs reported performing routine alcohol screening and counseling for patients presenting with alcohol-related complaints. We found that EDs that offered a range of preventive services were most likely to routinely perform alcohol screening and counseling for these patients.
We initially hypothesized that a larger proportion of urban, publicly owned, and crowded hospitals would report routine screening and counseling and this was indeed the case, except for publicly owned hospitals, where the relationship was not statistically significant. We also hypothesized that critical access hospitals would have higher rates of screening and counseling, but the inverse was true (these hospitals were less likely to perform screening). Finally, we hypothesized that lower rates of screening and counseling would be reported by EDs whose directors cited barriers to the provision of preventive services in their EDs. Our data support this hypothesis and also demonstrate that ED director opinions may be important for the perceived capacity to offer routine screening and counseling.
Of particular note, rates of routine screening and counseling were low among Level I/II trauma centers (22%), which are required by the American College of Surgeons (ACS) to perform routine alcohol screening for indicated patients. However, Level I/II trauma centers may be performing screening and counseling in inpatient wards or outpatient clinics, which could account for low rates of alcohol screening in their EDs. If this is indeed occurring, trauma centers may be missing a significant opportunity to screen patients who are not admitted. Only Level I trauma centers are required to have protocols to provide brief intervention to patients with alcohol-related complaints, while all Level I/II must be able to identify problem drinkers. Importantly, some trauma centers are certified by state agencies, not the ACS, and therefore may not adhere to the ACS screening and intervention requirements.
Our findings regarding the overall level of routine alcohol screening are similar to those of other studies that focused primarily on academic and urban EDs.16,17 For example, Cunningham and colleagues16 reported that 21% of Level I/II trauma centers used the CAGE instrument to screen for alcohol abuse in the ED; the authors also noted similar perceived barriers to performing routine screening (provider time and financial resources). Terrell et al17 found that 39% of Level I trauma centers routinely used a screening instrument for alcohol abuse, and provided informal or formal counseling to roughly one-quarter of patients who screened positive.
Our current study adds to the existing literature by presenting a diverse, nationwide sample of EDs, which supplements the existing literature on ED-based alcohol screening in academic and urban hospitals. To our knowledge, there are no published studies examining national rates of screening, particularly in non-trauma center EDs. Since the vast majority of U.S. EDs are non-trauma centers, it is particularly important to understand alcohol screening practices in these settings.
Capacity to routinely perform alcohol screening and counseling
Among EDs that did not routinely offer screening, EDs that had directors with concerns about preventive services or that were crowded, urban, or privately owned more often perceived lacking the capacity (as defined by a lack of existing staff and funding) to perform routine screening, as defined by a lack of existing staff and funding. This implies that extra resources for routine alcohol screening and counseling (or better knowledge of existing resources) in these settings would be necessary to increase overall utilization of this service in these EDs.
Addressing potential barriers to routine screening and counseling for alcohol misuse in EDs could increase the number of EDs that use this important preventive health measure. For example, addressing ED director-identified potential barriers to implementing preventive services—such as increased length of stay, increased financial costs to the ED, lack of adequate follow up, and diversion of nurse/physician time—may facilitate the adoption of alcohol screening and counseling in more EDs. Our research suggests that uniform reimbursement for SBIRT services and performing these services in a way that does not prolong ED length of stay would be particularly promising avenues for increasing adoption of these services. Finally, prior research has demonstrated that SBIRT can reduce subsequent ED usage.7 Therefore, routine screening could be considered as a way to decrease ED volume and crowding in the long term, which would address some of the directors’ concerns regarding these types of interventions.
Future research directions
Further research is indicated to examine the role of ED directors’ opinions in offering preventive services and to understand directors’ and physicians’ perceived benefits, barriers, and facilitators for ED-based alcohol screening. In particular, reasons for not offering alcohol screening and counseling despite having the existing staffing and funding to do so should also be investigated further. Research aimed at implementing alcohol screening and counseling without increasing ED length of stay or crowding should be explored. Further research is also indicated to understand whether patients presenting to trauma centers are receiving SBIRT as recommended by the American College of Surgeons, since trauma center EDs are offering these services at rates lower than the national average.
LIMITATIONS
There are some limitations to this study. First, the instrument used to collect data has not been previously validated with observation of EDs’ actual practices. The original survey instrument was intended to assess general attitudes about preventive services and was not solely focused on alcohol screening. The survey did not assess specific reasons why alcohol screening was not performed in trauma centers, as required by ACS. It is possible that some EDs performed screening but not counseling or referral for patients with alcohol-related complaints, which would artificially lower our estimate of routine screening. While the survey asked ED medical directors if their ED had a system in place to perform “risk screening, counseling, and referral,” we did not measure whether these services were actually delivered. Selection bias may have occurred, especially if EDs that did not offer preventive services represented a large proportion of non-responders. However, selection bias was likely averted with a high (80%) response rate, and the characteristics of our respondents were representative of EDs nationally (data not shown, full details have been published previously).19 There may be additional variables not included in our analysis that could be confounding or modifying our results. Finally, our sample size limited our ability to perform subgroup analyses and colinearity of some of the variables prevented multivariate analysis. Despite these limitations, this study provides valuable information on the current rates of routine alcohol screening in a large variety of EDs and also reveals important potential barriers and facilitators for offering routine alcohol screening.
CONCLUSION
To improve the rate of routine alcohol screening and counseling among patients presenting with alcohol-related complaints in U.S. EDs, perceived barriers related to an ED’s capacity to perform screening, such as limited financial and staff resources, should be addressed, as should directors’ concerns regarding the implementation of preventive health services in EDs. In particular, our research suggests that enabling the uniform reimbursement of routine ED-based alcohol screening and counseling and ensuring that these services do not prolong ED length of stay may increase adoption of this service. Future research is needed to better understand the role of specific facilitators and barriers in the use of routine alcohol screening, including the role of ED directors’ concerns about routine screening, the role of directors’ perceived capacity to perform routine screening, and the importance of reimbursement mechanisms for routine screening and counseling. Such knowledge could play a critical role in increasing the number of EDs that routinely screen and counsel indicated patients for alcohol misuse, ultimately leading to better identification of at-risk patients and referral to appropriate resources, such as substance abuse treatment.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michael A. Yokell, ScB. Stanford University School of Medicine, 291 Campus Dr.., Stanford, CA 94305. Email: myokell@stanford.edu. 7 / 2014; 15:438 – 445
Submission history: Revision received June 30, 2013; Submitted October 17, 2013; Accepted December 19, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 . Healthy People 2010. ;
2 Rehm J, Gmel G, Sempos C . NIAA Publications: Alcohol-related morbidity and mortality. 2003; :2
3 . Results from the 2010 national survey on drug use and health (NSDUH): summary of national findings. ;
4 . National ambulatory medical care survey– emergency department summary tables. 2008; :31
5 McDonald AJ, Wang N, Camargo CA US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Arch Intern Med. 2004; 164:531-537
6 Whiteman PJ, Hoffman RS, Goldfrank LR Alcoholism in the emergency department: an epidemiologic study. Acad Emerg Med. 2000; 7:14-20
7 Bray JW, Cowell AJ, Hinde JM A systematic review and meta-analysis of health care utilization outcomes in alcohol screening and brief intervention trials. Med Care. 2011; 49:287-294
8 The impact of screening, brief intervention and referral for treatment in emergency department patients’ alcohol use: a 3-, 6- and 12-month follow-up. Alcohol. 2010; 45:514-519
9 Bazargan-Hejazi S, Bing E, Bazargan M Evaluation of a brief intervention in an inner-city emergency department. Ann Emerg Med. 2005; 46:67-76
10 Madras BK, Compton WM, Avula D Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009; 99:280-295
11 Estee S, Wickizer T, He L Evaluation of the Washington state screening, brief intervention, and referral to treatment project: cost outcomes for Medicaid patients screened in hospital emergency departments. Med Care. 2010; 48:18-24
12 Schermer CR, Moyers TB, Miller WR Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. J Trauma. 2006; 60:29-34
13 Krupski A, Sears JM, Joesch JM Impact of brief interventions and brief treatment on admissions to chemical dependency treatment. Drug Alcohol Depend. 2010; 110:126-136
14 . Resources for Optimal Care of the Injured Patient. 2006;
15 Alcohol screening in the emergency department. Ann Emerg Med. 2005; 46:214-215
16 Cunningham RM, Harrison SR, McKay MP National survey of emergency department alcohol screening and intervention practices. Ann Emerg Med. 2010; 55:556-562
17 Terrell F, Zatzick DF, Jurkovich GJ Nationwide survey of alcohol screening and brief intervention practices at US Level I trauma centers. J Am Coll Surg. 2008; 207:630-638
18 Burt CW, McCaig LF Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003–04. Advance Data. 2006; 376:1-23
19 Delgado MK, Acosta CD, Ginde AA National survey of preventive health services in US emergency departments. Ann Emerg Med. 2011; 57:104-108