| Author | Affiliation |
|---|---|
| Samuel Ong, MD | Olive View–UCLA Medical Center, Department of Emergency Medicine, Sylmar, California |
| Gregory J Moran, MD | Olive View–UCLA Medical Center, Department of Emergency Medicine, Sylmar, California |
| Anusha Krishnadasan, PhD | Olive View–UCLA Medical Center, Department of Emergency Medicine, Sylmar, California |
| David A Talan, MD | Olive View–UCLA Medical Center, Department of Emergency Medicine, Sylmar, California |
ABSTRACT
Introduction:
Prophylactic antibiotics have not been found to have a benefit in the setting of uncomplicated lacerations. We evaluated the proportion of patients with uncomplicated lacerations who are prescribed prophylactic antibiotics in the emergency department (ED), factors that physicians considered when prescribing antibiotics, and factors associated with patient satisfaction.
Methods:
Adults and children presenting to 10 academic EDs with acute lacerations were enrolled. Enrolled patients were interviewed before and after their physician encounter in the ED and 2 weeks later. Physicians were interviewed in the ED after the patient encounter about factors that influenced their management decisions, including their perceptions of patients’ expectations. We included patients with uncomplicated lacerations (without contamination, infection, bone, tendon, or joint involvement) for analysis.
Results:
Of 436 patients enrolled, 260 had uncomplicated lacerations, and of these, 55 (21%) were treated with antibiotics in the ED or by prescription. Physicians were more likely to use antibiotics when the wound was more than 8 hours old, involved a puncture or amputation, and when the patient lacked medical insurance. A treatment course of 7 days or greater was given to 24 of 45 patients (53%) receiving outpatient prescriptions. Patient satisfaction was not associated with antibiotic use.
Conclusion:
Antibiotics were used for about one fifth of ED patients with uncomplicated lacerations despite a lack of evidence for efficacy.
INTRODUCTION
Background and Importance
Increases in antimicrobial resistance have been a growing concern, prompting a number of responses including the creation of task forces, surveillance programs, and legislation.1–5 Guidelines have been published for judicious antibiotic use in common respiratory conditions, such as bronchitis, but have resulted in only marginal success.6
Antibiotic use itself is not without some risk. A review of data from the National Electronic Injury Surveillance System-Cooperative Adverse Drug Surveillance project estimated that antibiotic use was responsible for nearly 125,000 emergency department (ED) visits annually.7 About 1 of 1,000 antibiotic prescriptions results in an ED visit because of an adverse reaction, a frequency consistent with more traditionally “high-risk” medications, such as warfarin and digoxin.8
Lacerations are among the leading complaints resulting in ED visits. In the 2006 National Hospital Ambulatory Medical Care Survey, open wounds were among the most common primary diagnosis groups and accounted for more than 6 million visits annually.9 The best way to prevent wound infection is thorough wound cleansing and appropriate closure technique.10 Clinical studies do not support routine antibiotic prophylaxis in simple wounds, yet a review of laceration management over the course of a decade found that antibiotics were prescribed to approximately 20% of patients with lacerations.11–16 Lacerations were not characterized as complicated or uncomplicated and the factors that contributed to antibiotic use were not studied. A national survey found that 38% of the responding emergency physicians reported using antimicrobial prophylaxis in noninfected wounds more than 25% of the time.17,18 Lacerations present another suitable target in the effort to decrease unnecessary antibiotic use.
Goals of the Investigation
This study was designed to examine the antibiotic-prescribing practices of physicians and the association of these practices with patient satisfaction in ED patients presenting with uncomplicated lacerations. We used surveys of both patients and treating physicians to assess the clinical and nonclinical factors associated with the decision to prescribe (or not prescribe) antibiotics. We also examined factors that may contribute to patient satisfaction, such as receipt of antibiotics, method of closure, and waiting times.
METHODS
Study Design
This was a multicenter, prospective, observational study. Patients were interviewed twice during the ED visit, directly before and after their physician encounter, followed by a telephone interview 2 weeks later. Treating physicians (residents or attending physicians) were interviewed as soon as possible after each patient encounter. The study was approved by the institutional review board at each site and at the Center for Disease Control (CDC).
Setting
Study sites comprised 10 members of a research network of geographically diverse US EDs (EMERGEncy ID NET), supported by the CDC.19 All sites are located in urban areas and have a combined annual census of over 800,000 ED visits. Each site supports an emergency medicine residency training program and is closely affiliated with a medical school.
Selection of Participants
Subjects were eligible for inclusion in the study if they were adult patients or guardians of children who presented to the ED triage area with a chief complaint involving a laceration. Subjects provided consent to undergo 2 brief interviews during the ED visit and a brief telephone follow-up interview 2 weeks later.
Two 2-week enrollment periods were conducted during the winter of 1999 into 2000 and the summer of 2000. Using standardized videos, each participating site trained a group of research associates to identify and screen patients, perform structured interviews, and record data. No on-duty medical staff performed interviews. Research associates approached patients for consent while the patients were awaiting physician evaluation.
Data Collection and Processing
Research associates interviewed each patient before and immediately after the physician encounter. Data collected on the previsit questionnaire included patient demographic characteristics, medical history, and characteristics of the injury, including the timing. Patients were asked about their expectations for medical care during the ED visit (eg, blood tests, radiographs, prescriptions for antibiotics, and hospitalization) and whether they believed that any medications would be important in the care and management of their laceration.
A second questionnaire was administered to patients after their physician encounter but before leaving the ED. The postvisit survey included an estimate of the patient’s waiting time and time spent with the treating physician. Patients were asked if they had received an antibiotic prescription, if they believed antibiotics were beneficial in the management of their laceration, and if they were “very satisfied,” “satisfied,” “uncertain,” “dissatisfied,” or “very dissatisfied” with their ED visit.
A final, follow-up questionnaire was administered by telephone to patients 2 weeks after their initial visit. Each patient was questioned as to whether or not the antibiotic prescription, if provided, was filled; if the wound had healed as expected; if additional care was sought or required; and the level of satisfaction with their initial ED visit.
Each patient’s treating physician was interviewed as soon as possible after the patient encounter, generally immediately after the research associate had completed the postvisit patient interview. The research associate told the physician that the survey was intended to study factors related to patient care but did not give any details about the study goals or provide the physician with any study information obtained from the patient. The physician was asked whether the patient seemed to expect medication for treatment of his or her illness and whether the patient requested any medication. If either response was affirmative, the physician was asked what type of medication was expected. The physician was asked whether an antibiotic was prescribed and to describe the factors related to that decision. The research associate next asked the physician to state the importance of a number of specific factors in the decision whether to prescribe an antibiotic, including wound characteristics (eg, wound length, location, and depth; presence of contaminants; bone, joint, or tendon involvement), underlying patient characteristics, and results of any tests performed in the ED. The physician was further asked to judge the wound as a “simple laceration” or a “high-risk wound.” Because physicians were not asked to provide informed consent, interview data were gathered anonymously; moreover, we did not perform analyses clustered by physician.
We developed the survey instrument by using the nominal group technique. A group of authors (D.A.T., G.J.M., S.O.) developed the study questions after a detailed review of prior studies and guidelines for appropriate use of antimicrobials in lacerations. After discussion of the survey questions during meetings of all study group members, we made revisions to the data collection instrument. The instrument then underwent pilot testing at a single study site, and we further modified questions as necessary to address ambiguities. We did not include data from the testing phase in the analysis.
Outcome Measures
The primary outcome measure was the rate of antibiotic use in uncomplicated lacerations. Secondary outcomes of interest included patient expectation, physician-perceived patient expectation, and patient satisfaction. In our a priori theoretic model, we anticipated that receipt of antibiotics would be associated with clinical factors and patients’ expectations and satisfaction.
Primary Data Analysis
We excluded patients with complicated lacerations from primary data analysis. Complicated lacerations were defined as those due to bites, with tendon or joint involvement, fracture, infection, or contaminated by dirt or foreign body. We generated descriptive statistics for categorical (frequencies) and continuous variables (medians and interquartile ranges). Bivariate analyses comparing patients who were prescribed antibiotics with and without certain demographics, wound characteristics, and other factors were expressed as unadjusted odds ratios (OR) with 95% confidence intervals (CI). We dichotomized patient satisfaction reports as “satisfied” (including “very satisfied” or “satisfied” responses) and “not satisfied” (including “uncertain,” “dissatisfied,” and “very dissatisfied” responses).
RESULTS
Subject Characteristics
During two 2-week periods, 436 patients were enrolled. The median age was 29 years (interquartile range [IQR], 21–40 years). Patients were predominantly male (68%), 42% were black, 30% were white, and 19% were Hispanic. Two hundred and thirteen patients (49%) had some form of insurance (private, Medicare, Medicaid, or other).
Forty-seven of 436 patients (11%) were excluded because of lacerations that were the result of bites (14) or complicated by the presence of tendon or joint involvement (12), fracture (12), or infection (9). Thirty-six of these 47 patients (77%) received antibiotics. One hundred twenty-nine of 436 patients (30%) were excluded because they presented with lacerations that were complicated by the presence of a foreign body or contaminant. The most common contaminants or foreign bodies were dirt in 61 cases (47%), glass in 37 (29%), and metal in 27 (21%). Forty-one of these 129 patients (29%) received antibiotics. The number of subjects enrolled, excluded with complicated lacerations, and comprising the study population of patients with uncomplicated lacerations is summarized in the Figure.
Two hundred sixty patients had uncomplicated lacerations. The median time from injury to ED presentation in these patients was 1.5 hours (IQR, 0.5–5 hours). Thirty-eight patients (20%) presented to the ED 8 hours or more from time of injury. Subject characteristics did not differ from the group as a whole. Thirty-four percent of subjects were evaluated by medical students and interns, 22% by first- and second-year residents, 27% by third- and fourth-year residents or fellows, and 18% by attending physicians.
Most lacerations (163 [63%]) were closed by sutures. Steri-strip or tape closure was used in 20 lacerations (7.7%), skin staples in 17 (6.5%), and skin adhesives in 14 (5.4%). Deep sutures were used in 23 of the patients with skin sutures, in 1 patient with skin staples, and as the sole method of closure in 3 patients (1.2%).
Fifty-three wounds were left open (20%). Patients who presented to the ED more than 6 hours after sustaining injury were more likely to have their wounds left open than sutured (OR, 5.1; 95% CI, 2.5–10.3). Patients whose wounds were left open were also more likely to receive antibiotics (OR, 2.7; 95% CI, 1.4–5.2). Two of 53 patients with open wounds reported receiving additional care after this ED visit. Sutures were placed more than 12 hours after injury in 7 patients (5 to face or scalp, 1 to the hand, and 1 to the leg, which was approximately 15 cm in length).
Antibiotic Usage
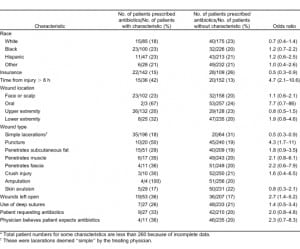
Fifty-five of 260 patients (21%) were treated with antibiotics (Table). Ten patients (4%) received antibiotics only in the ED, 31 (12%) received only antibiotic prescriptions, and 14 (5%) received both. Among those receiving prescriptions, first-generation cephalosporins were prescribed to 27 (60%), followed by trimethoprim/sulfamethoxazole to 6 (13%). Of the 45 patients with antibiotic prescriptions, 10 (22%) were given a 10-day treatment course; 14 (31%), a 7-day course; 11 (24%), a 5-day course; 2 (4%), a 3-day course; and 1 (2%) was given a 1-day course. In 7 patients (16%), the antibiotic course was not recorded.
Antibiotics were more likely to be used when the wound was more than 8 hours old, involved a puncture, or involved a skin or subcutaneous fat amputation (Table). Thirty of 55 patients (55%) treated with antibiotics did not possess any of the above-mentioned wound characteristics. Antibiotics were also more likely to be used when the patient lacked insurance. Wound length was not associated with antibiotic use.
Patient Expectations
Eighty-three of 260 patients (32%) expected antibiotics, believing that antibiotics would expedite wound healing. After their medical encounter, 63 of these 83 patients (76%) no longer believed that antibiotics were necessary. One hundred ninety-six (75%) expected to receive stitches, 112 (43%) expected pain medications, and 51 (20%) expected some form of radiographic evaluation.
Of the 83 patients who expected antibiotics, physicians correctly identified only 4 of them (5%). Of the 11 patients identified as expecting antibiotics by physicians, only 4 reported that they actually did expect to receive antibiotics. Overall, physicians correctly identified the antibiotic expectations of 174 of 260 patients (67%).
Satisfaction with Medical Care
Of the 241 responding patients, 214 (89%) were satisfied with the care they received in the ED. Patients with waiting times of less than 1 hour were more likely to be satisfied with their ED visit (OR, 4.5; CI, 1.8–10.2). Satisfaction was not associated with receipt of an antibiotic prescription (OR, 0.6; CI, 0.2–1.4). Satisfaction was also not associated with closure method.
DISCUSSION
Although recommendations for antibiotic use for complicated lacerations in the setting of bites, open fractures, tendon or joint involvement, and obvious infection have been published, no conclusive evidence exists to support routine antibiotic prophylaxis in uncomplicated lacerations.10,20 A meta-analysis of 7 placebo-controlled trials and 1,734 subjects with nonbite, simple wounds found prophylactic antibiotics were not associated with a reduced likelihood of infection (OR, 1.2; CI, 0.8–1.8).15 Inappropriate antibiotic use leads to avoidable adverse events and costs and may promote bacterial resistance.8 Lacerations were carefully characterized so as to exclude complicating conditions that have been acknowledged as potential indications for antibiotics. We found that 21% of patients presenting to various university-affiliated US EDs with uncomplicated lacerations were treated with antibiotics that would appear to have been inappropriately prescribed.
Among the many factors that were examined in relation to antibiotic prescription, only a few appeared to be associated with their use. Punctures, which were present in 8% of uncomplicated lacerations in this study, may be more infection prone and were associated with more frequent antibiotic use.20 Wounds older than 8 hours (15% of uncomplicated lacerations) were also associated with more frequent antibiotic use, although the literature suggests that wounds can be safely closed up to 18 hours.14,21 We found a trend toward greater antibiotic use in oral and lower-extremity injuries (present in 1% and 10% of uncomplicated wounds, respectively), which may also be more prone to infection.22,23 Since the infection rate of uncomplicated lacerations in general is approximately 5% or less, it is unlikely that there will be studies large enough to assess meaningful reductions in infection rates attributable to antibiotics when subgroup analyses are done of patients with otherwise uncomplicated lacerations who have these potential higher-risk wound characteristics. While this uncertainty may explain a portion of the apparent inappropriate antibiotic prescribing for uncomplicated lacerations, the benefit of antibiotics for wounds with these characteristics is probably small at best, and not greater than the potential associated risks. Patients with open wounds were also more likely to receive antibiotics that may have been given when delayed primary closure was considered, but this explanation seems less likely given that only 2 of the 53 patients with open wounds actually received additional medical care.
Patients who explicitly request antibiotics can influence physicians’ prescribing practices, even in conditions such as bronchitis in which there is no benefit.19,24 Physicians also overprescribe antibiotics when they believe the patient expects them,24,25 although their performance in predicting patients’ expectations may be inaccurate.24,25 In this study we again found that physicians performed poorly in identifying the patients who expected antibiotics. We did find a trend toward greater antimicrobial use to fulfill patient requests and physician perception of patient expectation. Directing education efforts toward both patients and physicians may be more effective. It may be helpful and instructive for physicians to know that patient satisfaction is not related to the receipt of antibiotics.
We found that more than half of the patients were given a 7-day (or longer) course of antibiotics, regimens more consistent with treatment rather than prophylaxis. Shorter antibiotic regimens may be less likely to result in the selection of resistant strains.26–29 Antibiotics are clearly indicated in the management of open fractures but even then treatment for more than 3 days provides no marginal benefit in preventing infection.30 We excluded most high-risk wounds, making it difficult to justify an antibiotic regimen significantly longer than that for open fractures. Encouraging the use of shorter prophylactic regimens, when they are deemed appropriate, may provide a viable secondary strategy for reducing overall selection pressure for antimicrobial resistance.

LIMITATIONS
We performed simple bivariate analyses without performing multivariate adjustments because of the number and heterogeneity of variables examined. Because we did not adjust for confounding or interaction, we may have overestimated or underestimated some associations. Some sites used convenience samples based on study-assistant availability, which may have subjected the results to some selection bias. Our study was based in urban, academic EDs; prescribing practices in other ED settings may differ. We performed a pilot study of the survey instrument but did not perform any formal assessment of the survey’s validity or reliability. While we could assess factors associated with physicians’ prescribing practices, we could not know what the doctors were actually thinking at the time and we did not assess their prior knowledge. Although the purported focus of the study was patient satisfaction, it is possible that participating physicians may have discovered that antibiotic use was under scrutiny and thus may have restricted antibiotic use accordingly. Similarly, our previsit survey asked patients about many facets of their medical visit, possibly affecting their expectations and prompting them to request antibiotics more frequently.
The time-from-injury data were not recorded for 102 patients. We also chose to exclude from further analysis patients with contaminated wounds because we could not ascertain the extent of contamination that could affect the need for prophylaxis. Prescribing practices may have changed in the 10 years since this study was conducted, particularly in light of the emergence of community-associated methicillin-resistant Staphylococcus aureus. This was not a randomized, placebo-controlled study, and therefore, we could not assess the efficacy of antibiotic use in general, or in specific subgroups of patients with uncomplicated lacerations.
CONCLUSION
Although a minority of uncomplicated lacerations in this investigation appeared to have been treated inappropriately with antibiotics, because of the vast numbers of patients who present to EDs with these injuries, more judicious use of antibiotics could result in a substantial number of patients avoiding antibiotic risk and costs. Awareness that patient satisfaction does not appear to be related to an antibiotic prescription—and of the results of existing studies that do not indicate a benefit of this practice—may reduce inappropriate antibiotic use in uncomplicated lacerations.
Footnotes
The following investigators participated in the EMERGEncy ID NET Study Group: F. M. Abrahamian (Olive View–University of California at Los Angeles Medical Center, Sylmar, California); E. Gross (Hennepin County Medical Center, Minneapolis, Minnesota); L. Lester (University of New Mexico Health Sciences Center, Albuquerque, New Mexico); W. K. Chiang (Bellevue Hospital Center, New York, New York); L. M. Dunbar (Louisiana State University Health Science Center, New Orleans, Louisiana; F. Lovecchio (Maricopa Medical Center, Phoenix, Arizona); B. Salhi (Emory University School of Medicine, Atlanta, Georgia); J. Jui (Oregon Health Sciences University, Portland, Oregon); D. J. Karras (Temple University School of Medicine, Philadelphia, Pennsylvania); M. T. Steele (University of Missouri–Kansas City, Kansas City, Missouri); D. M. Sullivan (Carolinas Medical Center, Charlotte, North Carolina); R. Rothman (Johns Hopkins Medical Center, Baltimore, Maryland). (EMERGEncy ID NET Study Group Members are available in the Appendix; online only).
Supervising Section Editor: Sukhjit S. Takhar, MD
Submission history: Submitted October 13, 2010; Revision received January 25, 2011; Accepted February 21, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.2.2115
Address for Correspondence: Samuel Ong, MD
Olive View–UCLA Medical Center, Department of Emergency Medicine, 14445 Olive View Dr, Sylmar, CA 91342
E-mail: samong@ucla.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. American Society for Microbiology. Report of the ASM task force on antibiotic resistance.Antimicrob Agents Chemother. 1995;;39:1–23. [PMC free article] [PubMed]
2. Goodman J, Murphy D. Key recommendations and report, December 2000. FDA Task Force on Antimicrobial Resistance Web site. Available at:http://www.fda.gov/oc/antimicrobial/taskforce2000.html. Accessed December 2008.
3. White AR; BSAC Working Parties on Resistance Surveillance. The British Society for Antimicrobial Chemotherapy Resistance Surveillance Project: a successful collaborative model. J Antimicrob Chemother. 2008;;62:ii3–14. [PubMed]
4. European Centre for Disease Prevention and Control. Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) The European Antimicrobial Resistance Surveillance System Web site. Available at: http://www.rivm.nl/earss/. Accessed December 2008.
5. Preservation of Antibiotics for Medical Treatment Act of 2007, S 549/HR 962 (2007.
6. Linder JA. Antibiotics for treatment of acute respiratory tract infections: decreasing benefit, increasing risk, and the irrelevance of antimicrobial resistance. Clin Infect Dis. 2008;;47:744–746.[PubMed]
7. Budnitz DS, Pollock DA, Weidenbach KN, et al. National surveillance of emergency department visits for outpatient adverse drug events. JAMA. 2006;;296:1858–1866. [PubMed]
8. Shehab N, Patel PR, Srinivasan A, et al. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008;47:735–743. [PubMed]
9. Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. National health statistics reports; No. 7. Hyattsville, MD: National Center for Health Statistics; 2008.
10. Moran GJ, Talan DA, Abrahamian FM. Antimicrobial prophylaxis for wounds and procedures in the emergency department. Infect Dis Clin N Am. 2008;;22:117–143.
11. Day TK. Controlled trial of prophylactic antibiotics in minor wounds requiring suture. Lancet.1975;;2:1174–1176. [PubMed]
12. Hutton PAN, Jones BM, Law DJW. Depot penicillin as prophylaxis in accidental wounds. Br J Surg. 1978;;65:549–550. [PubMed]
13. Grossman JA. Prophylactic antibiotics in simple hand lacerations. JAMA. 1981;;245:1055–1056.[PubMed]
14. Baker MD, Lanuti M. The management and outcome of lacerations in urban children. Ann Emerg Med. 1990;;19:1001–1005. [PubMed]
15. Cummings P, Del Beccaro MA. Antibiotics to prevent infection of simple wounds: a meta-analysis of randomized studies. Am J Emerg Med. 1995;;13:396–400. [PubMed]
16. Zehtabchi S. Evidence-based emergency medicine/critically appraised topic: the role of antibiotic prophylaxis for prevention of infection in patients with simple hand lacerations. Ann Emerg Med. 2007;;49:682–689. [PubMed]
17. Singer AJ, Thode HC, Hollander JE. National trends in ED lacerations between 1992 and 2002.Am J Emerg Med. 2006;;24:183–188. [PubMed]
18. Howell JM, Chisholm CD. Outpatient wound preparation and care: a national survey. Ann Emerg Med. 1992;;21:976–981. [PubMed]
19. Talan DA, Moran GJ, Mower WR, et al. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Ann Emerg Med. 1998;;32:703–711. [PubMed]
20. Nakamura Y, Daya M. Use of appropriate antimicrobials in wound management. Emerg Med Clin N Am. 2007;;25:159–176.
21. Berk WA, Osbourne DD, Taylor DD. Evaluation of the ‘golden period’ for wound repair: 204 cases from a third world emergency department. Ann Emerg Med. 1988;;17:496–500. [PubMed]
22. Lammers RL, Hudosn DL, Seaman ME. Prediction of traumatic wound infection with a neural network-derived decision model. Am J Emerg Med. 2003;;21:1–7. [PubMed]
23. Steele MT, Sainsbury CR, Robinson WA, et al. Prophylactic penicillin for intraoral wounds. Ann Emerg Med. 1989;;18:847–852. [PubMed]
24. Ong S, Nakase J, Moran GJ, et al. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med. 2007;;50:213–220. [PubMed]
25. Mangione-Smith R, McGlynn EA, Elliott MN, et al. The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics. 1999;;103:711–718.[PubMed]
26. D’Agata EMC, Magal P, Olivier D, et al. Modeling antibiotics resistance in hospitals: the impact of minimizing treatment duration. J Theor Biol. 2007;;249:487–499. [PMC free article] [PubMed]
27. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of β-lactam—risk factors for carriage of penicillin-resistant streptococcus pneumoniae. JAMA. 1998;;279:365–370.[PubMed]
28. Guillemot D, Varon E, Bernede C, et al. Reduction in antibiotic use in the community reduces the rate of colonization with penicillin G-nonsusceptible Streptococcus pneumoniae. Clin Infect Dis.2005;;41:930–938. [PubMed]
29. Hillier S, Roberts Z, Dunstan F, et al. Prior antibiotics and risk of antibiotic-resistant community-acquired urinary tract infection: a case control study. J Antimicrob Chemother. 2007;;60:92–99.[PubMed]
30. Gustilo RB, Merkow RL, Templeman D. The management of open fractures. J Bone Joint Surg Am.1990;;72:299–304. [PubMed]


