| Author | Affiliation |
|---|---|
| Michael Urdang, MD | University of Southern California, Department of Emergency Medicine, Los Angeles, California |
| Jennifer T Mallek, MS | University of Southern California, Keck School of Medicine, Los Angeles, California |
| William K Mallon, MD, DTMH | University of Southern California, Department of Emergency Medicine, Los Angeles, California |
ABSTRACT
Tattoos and piercings are increasingly part of everyday life for large sections of the population, and more emergency physicians are seeing these body modifications (BM) adorn their patients. In this review we elucidate the most common forms of these BMs, we describe how they may affect both the physical and psychological health of the patient undergoing treatment, and also try to educate around any potential pitfalls in treating associated complications.
INTRODUCTION
Tattoos and piercings (T&P) are ancient practices of body modification. The word tattoo comes from Polynesia and was first described by Captain Cook in 1769. The art form was named for the tapping noise made by a tattoo needle on the skin, which in the native tongue was tatau or tatu.1 Piercing, including the ear lobe, is also an ancient process, defined as the insertion of a needle to create a fistula for decorative ornaments. First recorded in the Middle East more than 5 thousand years ago, the practice is mentioned in Genesis 24:22 when Abraham asks his older servant to find a wife for his son Isaac. One of the gifts given to Rebecca, Isaac’s new wife, by the servant was a golden earring. Since then, ear piercing has become so well accepted that most scientific literature excludes the ear lobe in the definition of body piercing.
Social acceptability of these practices varies widely from culture to culture. Catholicism and Judaism have banned the practice of tattooing.2 Esthetics, personal expression, religious views, communication, and style are all motivations for obtaining a tattoo or a piercing. Once relegated to the margins of society (bikers, military, sailors), tattoos and piercings are now common across all ages and both genders in what has been described as an epidemic. For the emergency physician (EP), tattoos and piercings have become important nonverbal clues about the patient’s lifestyle and, furthermore, are increasingly the cause of an emergency department visit.3,4
This review provides EPs with the tools to be able to assess the lifestyle or social background of their patients, to be able to understand the medical complications that may arise as a result of body modification, and to have a deeper understanding of the psychologic associations of tattooing and, when necessary, the relevance of the body modification to the current chief complaint.
EPIDEMIOLOGY
Within Western society there has been a shift from the stereotype of the tattooed sailors, who used tattoos to communicate their travel and services, the outsider biker of the 1960s (Hell’s angels), and the gang members of the 1980s to the ornamental tattoo, which is now part of a collection of body modifications among women as much as men. Recent surveys completed in 2002 and again in 2006 have shown an increase in prevalence in tattoos within the US population.5,6 In 2002, a Harris poll showed a tattoo prevalence of 16%, whereas in 2006 a North American survey of 18 to 50 year olds found that 24% had tattoos and 14% had body piercings (excluding the ear). The surveys found that those who were tattooed were more likely to be less well educated, to have a high recreational drug use, and were less likely to show any religious affiliation.
Tattooing can be used to camouflage intravenous drug abuse, where it involves the antecubital fossa, and has an important place within generalized medical therapy. Its use is seen as a camouflage for dermatologic disease, can be added as a final stage in many plastic reconstructive procedures, and is also used for guidance in radiation therapy, endoscopic surgery, and ophthalmologic procedures.
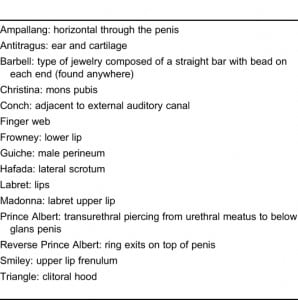
Studies, which have looked at the epidemiology of piercings, have found that 2% of Americans report having piercings (not including the ear lobe) and that females get more piercings than men. Among young adults who have piercings there is a high rate of associated eating disorders.7 Studies also show that persons who get piercings are more likely to partake in risky activities, including drug taking and sexual promiscuity, and have a higher risk of incarceration. The educational status and income of persons with T&P are generally lower, although these educational and economic disparities are lessening as T&P becomes more mainstream (Table 1).8,9
MEDICAL RELEVANCE FOR THE EMERGENCY PRACTITIONER
There are several ways that T&P are relevant to the practicing emergency practitioner (Table 2).
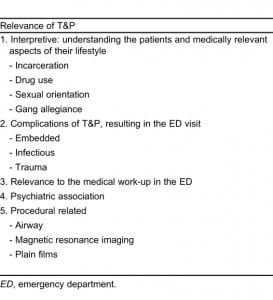
Interpretive Relevance
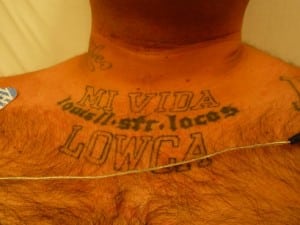
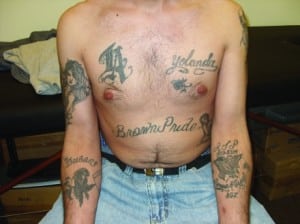
For the EP, T&P presents a window to the lifestyle and life experience of the patient. Many questions relevant to the history can be answered by a review of the T&P present. Figures 1 through 4 show examples of information obtained from T&P. While interpretation is not as simple as it was 30 years ago, when sailors, military members, and gangs had the most tattoos, relevant information is often within reach of the observant EP.

“LW” is a gang affiliation meant to be seen when wearing sandals.
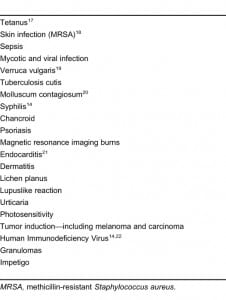
Complications of Tattoos
Tattoo complication rates show a prevalence of approximately 2% to 3%. Table 3 summarizes the complications associated with tattoos, many of which will be encountered by EPs. Most complications are related to infection that can be traced back to individual tattooist practicing a nonsterile technique. In particular, the jail and intravenous drug-using population is at risk for hepatitis B and C and methicillin-resistant Staphylococcus aureus infection.10–12. Even syphilis has been transmitted by a tattoo artist licking the tattoo needle.13 Failure to recognize a tattoo as the source of a complication leads to incorrect therapy. In many cases the tattoo is not correctly linked to the medical problem because the patient may have multiple risky behaviors.
Complications of Piercings
Complications of piercings are more common than those of tattoos and studies show rates as high as 9%. The types of complications include local or systemic infections, traumatic insertion, poor cosmesis, and rejection of foreign body, as well as migration and embedding.14 These are summarized in Table 4.
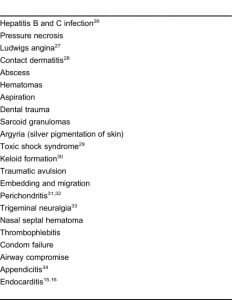
Jewelry is mainly body-site specific and made from metal. Metals used include stainless steel, gold, titanium, and various alloys. When these alloys contain nickel, there are associated allergic skin reactions and contact dermatitis. Specific complications relevant to the EP are summarized in Table 5. Rarer complications of piercings include bacterial endocarditis, tetanus, piercing migration with embedding, and even a case reported of appendicitis from a swallowed piercing that occluded the appendiceal aperture.15–18
Psychologic Associations of Body Modifications
The EP should be more concerned about illnesses and suicidal behavior in those with body modifications. Tattooing correlates with the perception of decreased mental health, and tattooing and body piercing together correlate highly with increased “sensation-seeking” behavior.19 A study of young tattooed Korean males conducted in Korea, where body modification is considered part of counterculture, used the Minnesota Multiphasic Personality Inventory personality test and found high scores in items of psychopathic deviance and schizophrenia, suggesting that those with tattoos were impulsive, hostile, and prone to delinquent behavior.20 A data analysis of 4,700 individuals who responded to a Web site (www.bmezine.com) for body modification found a high frequency of abuse in the background of those who participated. This survey also found that 36.6% of the males had suicidal ideation and 19.5% had attempted suicide. For the females, a statistically significant higher suicidality rate was found, with percentage values of 40.8% and 33.3% respectively.21 Skegg22noted that piercing was more common among women rated as having low constraint or high negative emotionality and was less common among those with high positive emotionality. Therefore, one can conclude that body piercing and tattoos, especially in females, could be a sign of suicidal behavior. However, no association has been found with eating disorders.7
Some authors have attempted to show positive association for these body modifications. In a study of women with eating disorders, the authors suggested that body piercing could be seen as reflecting a positive attitude towards the body, an expression of care.23 In addition people with piercings are more likely to give attention to their physical appearance and are less likely to be overweight than people without piercings.22

REMOVAL OF TATTOOS AND PIERCINGS
Burris and Kim24 found that 50% of persons with tattoos express regret and wish for tattoo removal. The quest for tattoo removal reflects earlier poor decision making and an embarrassing stigma often perceived by the age of 40 years. Tattoos may cause immediate and delayed hazard to health and are not easy to remove. Delayed complications include development of allergic, hypersensitivity, or granulomatous reactions that require tattoo removal.25 On average, tattoo regret occurs 14 years after tattooing and has spawned a whole new industry. Nonprofit organizations also provide tattoo removal to gang members wishing to remove their tattoos (www.homeboy-industries.org). Tattoos can be removed by mechanical, chemical, or thermal methods.
Alternatives to permanent tattoos include the Indian technique of staining the skin with henna. This will fade over a period of 7 to 10 days. In the past year there has been the development of nonpermanent tattoo ink. This technique uses ink-containing beads that are deployed in the same method as used previously. However, the ink can be fully removed by single-pass laser treatment (www.freedom2ink.com) that dissolves the bead, allowing the dye to be exposed to enzymes, laser, and UV rays.
CONCLUSION
Tattoos and piercings have become widespread practices that enjoy greater social acceptance than ever before. Body modification is important to the EP because it provides information about the “patient.” The physician can learn a great deal about these patients via their body modification, including information of immediate relevance to their medical evaluation. Secondarily, T&P are directly responsible for an increasing number of emergency department visits due to both immediate and delayed complications. The EP armed with knowledge about T&P/body modifications can forge more functional doctor-patient relationships, obtain critical historical data, and provide better treatment and referral for this patient population.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted March 28, 2011; Revision received April 21, 2011; Accepted April 22, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.4.2268
Address for Correspondence: Michael Urdang, MD
University of Southern California, Department of Emergency Medicine, 1200 N State St, Rm 1011, Los Angeles, CA 90033-1029
E-mail: murdang@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Tattoos By Design. History of tattoos. Tattoos By Design Web site. Available at: www.tattoos-by-design.co.uk/history.html. Accessed April 23, 2008.
2. Gennaro J. A brief tattoo history. Religious Tattoos Web site. Available at:www.religioustattoos.net/tattoos-history/index. Accessed April 23, 2008.
3. Scheinfeld N. Tattoos and religion. Clin Dermatol. 2007;;25:362–365. [PubMed]
4. Vassileva S, Hristakieva E. Medical applications of tattooing. Clin Dermatol. 2007;;25:367–374.[PubMed]
5. Laumann A, Derick A. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol. 2006;55:413–421. [PubMed]
6. Sever J. The Harris Poll No. 58, October 8, 2003. Harris Interactive Web site. Available at:http://harrisinteractive.com/harris_poll/printerfriend/index.asp?PID=407. Accessed April 23, 2008.
7. Preti A, Pinna C, Nocco S, et al. Body of evidence: tattoos, body piercing, and eating disorder symptoms among adolescents. J Psychosom Res. 2006;;61:561–566. [PubMed]
8. Armstrong ML, Roberts AE, Koch JR, et al. Investigating the removal of body piercings. Clin Nurs Res. 2007;;16:103–118. [PubMed]
9. Panconesi E. Body piercing: psychosocial and dermatologic aspects. Clin Dermatol.2007;;25:412–416. [PubMed]
10. Samuel MC, Doherty PM, Bulterys M, et al. Association between heroine use, needle sharing and tattoos received in prison with hepatitis B and C positivity among street-recruited injecting drug users in New Mexico, USA. Epidemiol Infect. 2001;;127:475–484. [PMC free article] [PubMed]
11. Zeuzem S, Teuber G, Lee JH, et al. Risk factors for the transmission of hepatitis C. J Hepatol.1996;;24:3–10. [PubMed]
12. Stemper ME, Brady JM, Qutaishat SS, et al. Shift in Staphylococcus aureus clone linked to an infected tattoo. Emerg Infect Dis. 2006;;12:1444–1446. [PMC free article] [PubMed]
13. Long GE, Rickman LS. Infectious complications of tattoos. Clin Infect Dis. 1994;;18:610–619.[PubMed]
14. Meltzer DI. Complications of body piercing. Am Fam Physician. 2005;72:2029–2034. [PubMed]
15. Ochsenfahrt C, Friedl R, Hannekum A, et al. Endocarditis after nipple placement in a patient with bicuspid aortic valve. Ann Thorac Surg. 2001;;71:1365–1366. [PubMed]
16. Lick SD, Edozie SN, Woodside KJ, et al. Streptococcus viridans endocarditis from tongue piercing. J Emerg Med. 2005;;29:57–59. [PubMed]
17. O’Malley CD, Smith N, Braun R, et al. Tetanus associated with body piercing. Clin Infect Dis.1998;;27:1343–1344. [PubMed]
18. Hadi HI, Quah HM, Maw A. A missing tongue stud: an unusual appendicular foreign body. Int Surg. 2006;;91:87–89. [PubMed]
19. Stuppy DJ, Armstrong ML, Casals-Ariet C. Attitudes of health care providers and students toward tattooed people. J Adv Nurs. 1998;;27:1165–1170. [PubMed]
20. Kim JJ. A cultural psychiatric study on tattoos of young Korean males. Yonsei Med J.1991;;32:255–262. [PubMed]
21. Hicinbothem J, Gonsalves S, Lester D. Body modification and suicidal behavior. Death Stud.2006;;30:351–363. [PubMed]
22. Skegg K, Nada-Raja S, Paul C, et al. Body piercing, personality, and sexual behavior. Arch Sex Behav. 2007;;36:47–54. [PubMed]
23. Claes L, Vandereycken W, Vertommen H. Self-care versus self-harm: piercing, tattooing, and self-injuring in eating disorders. Eur Eat Disord Rev. 2004;;13:11–18.
24. Burris K, Kim K. Tattoo removal. Clin Dermatol. 2007;;25:388–392. [PubMed]
25. Stirn A. Trauma and tattoo-piercing, tattooing and related forms of body modification between self-care and self-destruction of traumatized individuals. Psychotraumatologie. 2002;2:45.
26. Van Sciver AE. Hepatitis from ear piercing. JAMA. 1969;207:2285. [PubMed]
27. Perkins CS, Meisner J, Harrison JM. A complication of tongue piercing. Br Dent J. 1992;182:147–148. [PubMed]
28. Fischer T, Fregert S, Gruvberger B, et al. Nickel release from ear piercing kits and earrings.Contact Dermatitis. 1984;10:39–41. [PubMed]
29. McCarthy VP, Peoples WM. Toxic shock syndrome after ear piercing. Pediatr Infect Dis J.1988;7:741–742. [PubMed]
30. Lane JE, Waller JL, Davis LS. Relationship between age of ear piercing and keloid formation.Pediatrics. 2005;115:1312–1314. [PubMed]
31. Turkeltab SH, Habal MB. Acute Pseudomonas chondritis as a sequel to ear piercing. Ann Plast Surg. 1990;24:279–281. [PubMed]
32. Hanif J, Frosh A, Marnane C, et al. Lesson of the week: “High” ear piercing and the rising incidence of perichondritis of the pinna. BMJ. 2001;322:906–907. [PMC free article] [PubMed]
33. Gazzeri R, Mercuri S, Galarza M. Atypical trigeminal neuralgia associated with tongue piercing.JAMA. 2006;296:1840–1842. [PubMed]
34. Hadi HI, Quah HM, Maw A. A missing tongue stud: an unusual appendicular foreign body. Int Surg. 2006;91:87–89. [PubMed]
35. Maheu-Robert LF, Andrian LE, Grenier D. Overview of complications secondary to tongue and lip piercings. J Can Dent Assoc. 2007;73:327–331. [PubMed]
36. Simplot TC, Hoffman HT. Comparison between cartilage and soft tissue ear piercing complications. Am J Otolaryngol. 1998;19:305–310. [PubMed]
37. Gokhale R, Hernon M, Ghosh A. Genital piercing and sexually transmitted infections. Sex Transform Infect. 2001;77:393–394.


