| Author | Affiliation |
|---|---|
| Peter J. Mariani, MD | State University of New York Upstate Medical University, Syracuse, NY |
ABSTRACT
The U.S. Department of Health and Human Services Office of the Inspector General has issued a report concerning “high use” and “questionable use” ultrasound. Findings include those geographic areas where occurrences are most frequent, as well as the most common elements that characterize questionable use. While not its primary focus, emergency physician performed bedside ultrasound is within the scope of the report. Implications for emergency ultrasound are discussed and practice recommendations made for minimizing regulatory exposure for emergency physicians and departments.
BACKGROUND
In July 2009, the U.S. Department of Health and Human Services Office of the Inspector General (OIG) reported results of an investigation concerning “high use” and “questionable use” of ultrasound.1 OIG identified counties exhibiting high ultrasound use and determined whether reimbursement claims had certain “questionable characteristics.” The office examined Ultrasound Part B technical component claims for 2007. Of 41 million identified, a technical component was billed in 18.8 million. Further exclusions resulted in a final data set of 17 million claims involving beneficiaries in 3,239 counties.
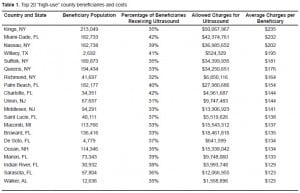
They assessed two variables of use: 1) average annual ultrasound charges per beneficiary and 2) percentage of beneficiaries who received ultrasound services. Twenty counties were found to occupy the top one percent of both of these measures (Figure 1). They accounted for 16% of Medicare’s ultrasound costs despite being populated by only 6% of its beneficiaries. Part B spent an average of $171 per beneficiary in the high-use counties compared to $55 in the rest of the country. Use for the top 20 counties appears in Table 1.

The OIG then examined the claims for presence of certain attributes it deemed “questionable.” Five assessed characteristics were:
-
Absence of a preceding service claim from the ordering physician.
-
Use of suspect combinations of billing codes, “such as billing for both a complete abdominal scan and a scan of an individual organ within the abdominal cavity.”
-
Occurrence of more than five ultrasounds provided to the beneficiary on the same day by the same provider.
-
Beneficiaries who had ultrasounds billed by more than five providers.
-
Missing or invalid ordering physician identifiers.
The OIG discovered that the first was by far the most frequent, occurring in 17% of claims. The remaining four occurred each with frequencies < 2%.
Final OIG recommendations to the Centers for Medicare and Medicaid Services (CMS) call for CMS to monitor for and act on questionable claims. Potential action includes individual review prior to payment. CMS concurred, reporting they would, “take appropriate action to forward the listing of questionable claims to the recovery audit contractors [RACs] and Medicare administrative contractors [MACs].”
IMPLICATIONS FOR EMERGENCY ULTRASOUND
To what extent does the OIG report impact current emergency department (ED) practice? Does standard clinician-performed bedside ultrasound in the ED risk raising red flags to the government or its bounty hunters?
As the technical component of hospital-based ED ultrasound is billed (if at all) to Part-A, OIG’s specific audit of Part-B technical component claims indicates focus elsewhere; it’s unlikely that OIG had explicit interest in EDs. Emergency physician (EP) groups generally do not bill for the technical component and instead, via the −26 modifier, explicitly limit claims to the professional component. Maintaining distance from OIG/CMS’ newfound interest is an additional reason to continue this practice.
We should not, however, conclude that ED ultrasound remains uninteresting to regulators. OIG’s conclusions appear to extend to all of Part B ultrasound, notwithstanding the study’s audit of only technical component claims. Per the report’s overview: “Compared to other types of diagnostic imaging machines, which can cost millions of dollars to acquire and install, ultrasound machines are relatively inexpensive. Providers can buy used machines for under $5,000 and roll them into examining rooms on carts.” The OIG appears to presume that inexpensive fraud/abuse is more frequently committed than fraud/abuse requiring greater investment. While perhaps displaying greatest concern for fraudulent low budget “diagnostic mills,” OIG’s portrayal of “rolling in the machine” does accurately describe this physical element of ED practice.
The most common “questionable” ultrasound claim characteristic identified by OIG was the “[absence] of a prior service claim from the doctor who ordered the ultrasound.” This refers to an ultrasound ordered and performed without a preceding Evaluation & Management encounter to generate an ultrasound-addressable question. It is almost inconceivable that an ED ultrasound would be billed without an associated EP’s evaluation and management (E&M) code billed concurrently. Therefore, the most common questionable claim would likely never occur in legitimate emergency medicine practice.
Also determined to be questionable were “[instances] of more than five ultrasound services provided to the same beneficiary on the same day by the same provider.” Can reasonable ED practice inadvertently trigger scrutiny via this criterion? In its White Paper 2 and Update 3 on coding and billing, the American College of Emergency Physicians enumerates multiple ultrasound CPT codes that can be appropriately billed for a single acute patient. The initial evaluation of undifferentiated shock can require numerous diverse insonations,4 all generating CPTs. Serial focused assessments with sonography for trauma (FASTs) are an established ultrasound use for the trauma patient with changing clinical condition. To the above examples, the reader is invited to additionally assume that patients are female and possibly pregnant. It’s easily conceivable that these and other patients receiving legitimate ultrasound imaging could transgress this OIG “Rule of 5” on a single ED encounter with a single ED provider. If justification for such “questionable characteristic” ultrasounds is clearly reflected in the patient record, it’s unlikely that the studies would fail scrutiny. They might, however, still generate initial scrutiny, possibly resulting in individual reimbursement delay and/or consequent wider audit of claims.
The OIG also assigned “questionable” status to the characteristic: “Beneficiaries who had ultrasound services billed for them [in a single year] by more than five providers.” Are there ED patients at risk of triggering this criterion? Anyone who presents frequently to the ED with chest pain might frequently receive bedside echocardiography for assessment of pericardiditic effusion. A critically ill ED patient could undergo several diagnostic scans (e.g. serial eFASTs) and ultrasound-guided procedures. Following intensive care unit admission, intensivists or radiologists performing more of the same could add to the total. Even in the course of a single hospitalization, such a patient could transgress this OIG “Other Rule of 5.” Once again, appropriate documentation demonstrating medical justification/necessity is the best cure for later scrutiny.
Do any of the OIG’s geographic findings implicate ED ultrasonography? Metropolitan and suburban downstate New York counties figure prominently among the top half-dozen identified as “high-use.” This region is also distinguished by a higher prevalence of emergency ultrasound (EUS) fellowships. This is almost certainly a correlation without causation. The OIG does note that such high-use counties have generally higher ultrasound provider-to-beneficiary ratios than remaining counties. In fact, the ratio is approximately tripled. The contribution of EUS fellowships to overall provider numbers is likely negligible. Additionally, the prominence of South Florida counties characterized as “high-use” is without similar correlation and likely reflects an older and sicker population, as well as a higher provider/beneficiary ratio. Consistent with other interpretations in this commentary, the above does not prominently place emergency medicine on the OIG ultrasound radar screen, but neither does it explicitly remove it. An ED’s geographic location could be future cause for increased CMS scrutiny.
CONCLUSION
EPs in general, and those performing bedside ultrasound in particular, are experienced with life in the fish bowl. With its recent report, the OIG joins the ranks of on looking ichthyologists. EUS practitioners and their coding and billing agents should keep abreast of regulatory developments and their implications as discussed above. Evidence-based, medically indicated and competently performed imaging should be practiced by appropriately credentialed physicians and be accurately reflected in the medical record. Physician group practices and hospitals should stand ready to appeal the adverse audit.5 Emergency medicine specialty societies should monitor for problems encountered by members, and lobby to correct any abusive enforcement practices by the government or its contractors.
Footnotes
Supervising Section Editor: Seric S Cusick, MD
Submission history: Submitted August 4, 2009; Revision Received October 8, 2009; Accepted October 25, 2009.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Peter J. Mariani MD FAAEM, Professor, Department of Emergency Medicine, SUNY Upstate Medical University, Syracuse, NY 13210
Email: marianip@upstate.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Department of Health and Human Services Office of Inspector General Part-B Billing for Ultrasound. Publication # OEI-01-08-00100, July 2009. DHHS website. Available athttp://oig.hhs.gov/oei/reports/oei-01-08-00100.pdf.downloaded July 22, 2009.
2. Ultrasound Section of the American College of Emergency Physicians Emergency Ultrasound Coding and Reimbursement. ACEP website. Available at:http://www.acep.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=33016.downloaded July 22, 2009.
3. Hoffenberg S, Goldstein J. Emergency Ultrasound Coding and Reimbursement Update 2007. ACEP website. Available at: http://www.acep.org/WorkArea/DownloadAsset.aspx?id=33280.downloadedJuly 22, 2009.
4. Jones AE, Tayal VS, Sullivan DM, et al. Randomized controlled trial of immediate versus delayed goal-directed ultrasound to identify the cause of nontraumatic hypotension in emergency department patients. Crit Care Med. 2004;32(8):1703–8. [PubMed]
5. Braccili R. Medicare RACs: how should hospitals prepare? Healthcare Financial Mgt. 2009;63:60–7.


