| Author | Affiliation |
|---|---|
| Matthew Ahern, DO | University of Utah, Division of Emergency Department, Salt Lake City, UT |
| Michael P. Mallin, MD | University of Utah, Division of Emergency Department, Salt Lake City, UT |
| Scott Weitzel, MD | University of Utah, Division of Emergency Department, Salt Lake City, UT |
| Troy Madsen, MD, MPH | University of Utah, Division of Emergency Department, Salt Lake City, UT |
| Pat Hunt, MD | University of Utah, Division of Emergency Department, Salt Lake City, UT |
ABSTRACT
Introduction:
Education in emergency ultrasound (EUS) has become an essential part of emergency medicine (EM) resident training. In 2009, comprehensive residency training guidelines were published to ensure proficiency in ultrasound education. The American College of Emergency Physicians (ACEP) recommends that 150 ultrasound exams be performed for physician competency. Our goal is to evaluate the current ultrasound practices among EM residency programs and assess the need for further formalization of EUS training.
Methods:
We generated a survey using an online survey tool and administered via the internet. The survey consisted of 25 questions that included multiple choice and free text answers. These online survey links were sent via email to EM ultrasound directors at all 149 American College of Graduate Medical Education EM residency programs in April 2008. We surveyed programs regarding EUS curriculum and residency proficiency requirements and descriptive statistics were used to report the survey findings.
Results:
Sixty-five residency programs responded to the survey. The average number of ultrasound exams required by programs for EUS competency was 137 scans. However, the majority of programs 42/65 (64%) require their residents to obtain 150 scans or greater for competency. Fifty-one out of 64 (79%) programs reported having a structured ultrasound curriculum while 14/64 (21%) of programs reported that EUS training is primarily resident self-directed. In terms of faculty credentialing, 29/62 (47%) of residency programs have greater than 50% of faculty credentialed. Forty-four out of 61 (72%) programs make EUS a required rotation. Thirty-four out of 63 (54%) programs felt that they were meeting all their goals for resident EUS education.
Conclusion:
Currently discrepancies exist between EM residency programs in ultrasound curriculum and perceived needs for achieving proficiency in EUS. Although a majority of residency programs require 150 ultrasound exams or more to achieve resident competency, overall the average number of scans required by all programs is 137 exams. This number is less than that recommended by ACEP for physician competency. These data suggest that guidelines are needed to help standardize ultrasound training for all EM residency programs.
INTRODUCTION
Education in emergency ultrasound (EUS) has become an essential part of emergency medicine (EM) resident training. However, it is unclear what degree of standardization exists among EM residency programs in terms of ultrasound training. In the past, several organizations, including the American College of Emergency Physicians (ACEP), Society for Academic Emergency Medicine (SAEM) and American Academy of Emergency Medicine (AAEM), have issued position statements or guidelines regarding the use of ultrasound by emergency physicians.1–3 These guidelines served as a standard for many residency programs in developing their EUS education and curriculum.
In 2009, ACEP issued a policy statement that outlined guidelines for residency EUS education.4 It follows previously developed guidelines, which were not evidence-based and were developed for practicing emergency physicians with little previous residency ultrasound training.5 The most recent published data surveying the status of ultrasound training was performed in 2001.6 The goal of our study was to evaluate the current ultrasound practices among EM residency programs through a survey of programs.
METHODS
We generated a survey using an online survey tool and administered it via the internet. The survey consisted of 25 questions, which included multiple choice and free text answers regarding residency programs’ EUS requirements, structure of their ultrasound curriculum, number of credentialed faculty, method of quality assurance and overall perceptions of their own curriculum. We sent a link to this online survey via email to EM ultrasound directors, program coordinators and residency program directors at all Accreditation Council for Graduate Medical Education (ACGME) EM residency programs in April 2008. The survey was anonymous; no identifier linked individual surveys to individual programs.
After one month, a second email was sent to all programs directors and, if available, ultrasound directors, requesting survey completion. The survey was closed and the data collected in May 2008. Data were analyzed using descriptive statistics.
RESULTS
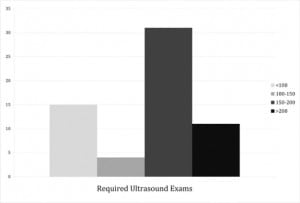
A total of 65 out of 149 (44%) ACGME EM residency programs responded to the survey. The average number of ultrasound scans required for EUS competency across all reporting residencies was 137. The majority of programs, 42/65 (67%) required greater than 150 scans, 9/65 (13.8%) required greater than 200 scans, while four programs had no specified number of scans for competency. For programs reporting a competency requirement the range was 25 to 300 scans (Figure 1).
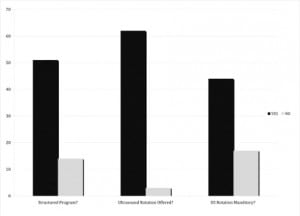
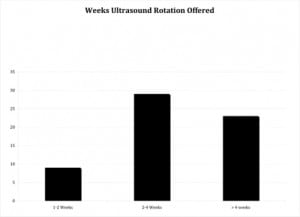
A majority of reporting programs, 51/64 (79%) had a structured ultrasound curriculum, while the remainder of programs report that EUS training is primarily resident self-directed. A formal ultrasound rotation is offered at 62/65 (95%) of residencies but is required at only 44/65 (72%) of these programs (Figure 2). Residencies reported variability in the length of formal ultrasound rotations offered. Of 62 programs that responded, nine (15%) reported that they offer 1–2 weeks of ultrasound rotation, while 29 (47%) offered a 2–4 week ultrasound rotation. Finally, 23 (37%) of the residencies offered an ultrasound rotation longer than four weeks (Figure 3).
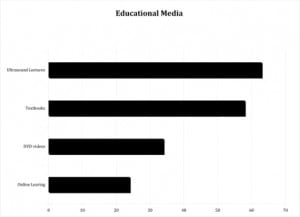
Multiple forms of instructional media educated residents about EUS. The majority (80%) use lecture-based education to train their residents in ultrasound. In addition to lectures, 36% of reporting residencies use some form of online education to train their residents (Figure 4). Fifteen programs responded when asked the number of hours they commit to ultrasound-related lectures during the course of resident training. On average residents received 34 hours of ultrasound-specific lectures during their training. Of the programs that reported faculty involvement in training, the average number of dedicated faculty hands-on instruction was 46 hours during the course of residency training; however, only 15 programs responded to this question (Figure 6).
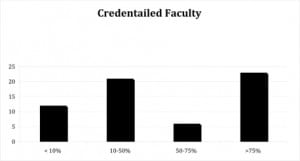

In terms of faculty credentialing, 29/62 (47%) of residency programs have greater than 50% of faculty credentialed. A large majority, 62/64 (96%) of credentialed faculty reported using ultrasound in patient care decisions (Figure 5).
A majority of programs, 47/64 (73%) felt no adversity within their hospital to emergency department use of ultrasound and EM resident ultrasound education.
Approximately half, 34/63 (54%) of programs reported meeting all of their goals for resident EUS. Only 5/63 (7.9%) reported not meeting their ultrasound program goals.
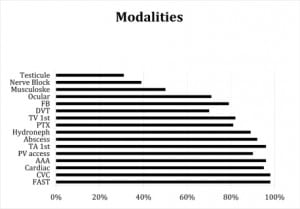
Figure 7 reports the different types of ultrasound modalities that EM residents are currently being trained in.
DISCUSSION
Ultrasound education is becoming an increasingly important part of EM residency training. EM organizations such as ACEP have developed guidelines for residency training in different ultrasound modalities.4 There are no recent surveys that report the current state of emergency ultrasound training or how residency programs have implemented these guidelines.
Although our data show discrepancies in ultrasound training among all residency programs, we found that progress has been made in EUS training when we compared our data to past surveys. Review of the 2001 study by Counselman et al. suggests there have been significant increases in the number of hours of dedicated ultrasound didactic training. In 2001, 76%, of programs offered between 1–20 hours of formal didactic training while our survey respondents in 2008 reported a total average of 34 hours dedicated to ultrasound didactics and lectures.6 Also, in terms of hands-on resident ultrasound training, there has been an even greater increase. In the 2001 survey, 83% of programs offered less than 20 hours of direct, hands-on resident ultrasound training. In contrast, we found that residents received an average of 46 hours of direct, hands-on training for all reporting programs.
Interestingly, programs are now reporting ultrasound training in more advanced applications. Most of the earlier literature surveying residency training reported training in only six or seven core EUS applications.6 Our data set indicates that more than 50% of the responding programs offer training in 13 applications.
Faculty credentialing appears to be another area of advancement with 61% of programs reporting half of their faculty credentialed in ultrasound. Furthermore, 94% of programs reported credentialed faculty using ultrasound in patient care decisions. These numbers suggest a growing percentage of faculties in residency programs using ultrasound for patient care and passing that practice on to future emergency physicians.
One area we have identified for improvement is in requirements for resident competency. The average number of scans required among all programs was 137, which is slightly less than that suggested as a guideline for physician competency by ACEP. Furthermore, we noticed a large discrepancy in the number of required scans between residency programs. The majority of programs (64%) required more than 150 ultrasound exams for competency. This is a considerable improvement in comparison to a survey study by Witting in 1998, in which only one program reported meeting SAEM guidelines.7 It is also worth noting that 14% of respondents required greater than 200 ultrasound exams for residency competency. Only a small percentage of programs reported requiring significantly less than the benchmark of 150 ultrasound exams.
While ACEP has established this number, it is uncertain whether 150 ultrasound exams is an important benchmark to achieve in obtaining EUS competency. ACEP points out that these guidelines are not evidence based.8 In fact, we are unaware of any study that demonstrates a particular number of ultrasound exams to correlate with competency. However, these results do demonstrate that the majority of programs in the United States are requiring greater than 150 ultrasound exams for resident competency.
Our survey found that a majority (80%) of programs considered their ultrasound program highly structured with 72% of programs requiring mandatory ultrasound rotation and training. There is considerable advancement in EUS training when one considers that in a survey by Cook and Roepke 10 years ago only 50% of programs reported offering any training in emergency ultrasound.9
Finally, it appears that despite the relative infancy of EUS, 73% of the reporting programs in our study stated there is low institutional opposition to training residents in emergency ultrasound.
LIMITATIONS
The study has several limitations. Only 65 of the 149 EM residency programs responded to our survey. The fact that there was only a 44% response rate is a significant limitation of this data set. However, the data suggest that residencies with well-developed ultrasound programs may have been more likely to respond. This is witnessed by the fact that a disproportionate percentage, 26/65 (40%) of programs responding offer a fellowship, a number higher than the expected number of fellowships available. Therefore, although we are unable to characterize the use of ultrasound in the 84 programs that did not respond to our survey, the data set can be assessed as a best-case scenario since those programs that failed to respond are likely to have less developed ultrasound curricula.
CONCLUSION
Currently there exist discrepancies among EM residency programs in ultrasound curricula and perceived needs for achieving proficiency in EUS. Although a majority of residency programs responding to the survey require 150 ultrasound exams or more to achieve resident competency, overall the average number of scans required by all programs is 137 exams. This number is slightly less than that recommended by ACEP for physician competency. There currently exists a feeling among emergency ultrasound educators that formal competency assessment and testing will be needed in the near future for the credentialing of physicians in the use of emergency bedside ultrasound. With this there also exists the possibility that competency testing in EUS will be a separate certification from the EM board-testing process. Our data suggest that discrepancies currently exist among residency programs in the level and quality of ultrasound training. These findings suggest that further guidelines help standardize ultrasound training for all EM residency programs may be warranted.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted June 15, 2009; Revision Received October 29, 2009; Accepted March 15, 2010
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Michael P. Mallin, MD, Division of Emergency Medicine, 30 South 1500 East Rm1C026, University of Utah, Salt Lake City, UT 84132
Email: michael.mallin@hsc.utah.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. American College of Emergency Physicians Use of ultrasound imaging by emergency by emergency physicians [policy statement] Ann Emerg Med. 2001;38:469–70. [PubMed]
2. Society for Academic Emergency Medicine Ultrasound policy statement. SAEM Newsletter. 1991 Summer;:2.
3. American Academy of Emergency Medicine Performance of emergency screening ultrasound examinations. Common Sense. 1999;6(2):8.
4. American College of Emergency Physicians Use of ultrasound by Emergency Physicians.http://acep.org/practres.aspx?id=32882.
5. Mateer J, Plummer D, Heller M, et al. Model curriculum for physician training in emergency training in emergency ultrasonography. Ann Emerg Med. 1994;23(1):95–102. [PubMed]
6. Counselman F, et al. The Status of Bedside Ultrasound Training in Emergency Medicine Resideny Programs. Acad Emerg Med. 2003;10:37–42. [PubMed]
7. Witting MD, Euerle BD, Butler KH. A comparison of emergency medicine ultrasound training with guidelines of the Society of Academic Emergency Medicine. Ann Emerg Med. 1998;16:655–7.
8. Mateer J, Plummer D, Heller M, et al. Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med. 1994;23:95–102. [PubMed]
9. Cook T, Roepke T. Prevalence and structure of ultrasound curricula in emergency medicine residencies. J Emerg Med. 1998;16:65–7.


