| Author | Affiliation |
|---|---|
| Tomohiro Sonoo, MD | The University of Tokyo Hospital, Emergency Medicine and Critical Care Medicine Department, Bunkyo-ku, Tokyo, Japan; Hitachi General Hospital, Emergency Medicine Department, Hitachi-shi, Ibaraki, Japan |
| Ryota Inokuchi, MD | The University of Tokyo Hospital, Emergency Medicine and Critical Care Medicine Department, Bunkyo-ku, Tokyo, Japan; Hitachi General Hospital, Emergency Medicine Department, Hitachi-shi, Ibaraki, Japan |
| Miyuki Yamamoto, MD | The University of Tokyo Hospital, Emergency Medicine and Critical Care Medicine Department, Bunkyo-ku, Tokyo, Japan; Hitachi General Hospital, Emergency Medicine Department, Hitachi-shi, Ibaraki, Japan |
| Kensuke Nakamura, PhD | Hitachi General Hospital, Emergency Medicine Department, Hitachi-shi, Ibaraki, Japan |
| Susumu Nakajima, PhD | The University of Tokyo Hospital, Emergency Medicine and Critical Care Medicine Department, Bunkyo-ku, Tokyo, Japan |
| Naoki Yahagi, PhD | The University of Tokyo Hospital, Emergency Medicine and Critical Care Medicine Department, Bunkyo-ku, Tokyo, Japan |
CASE
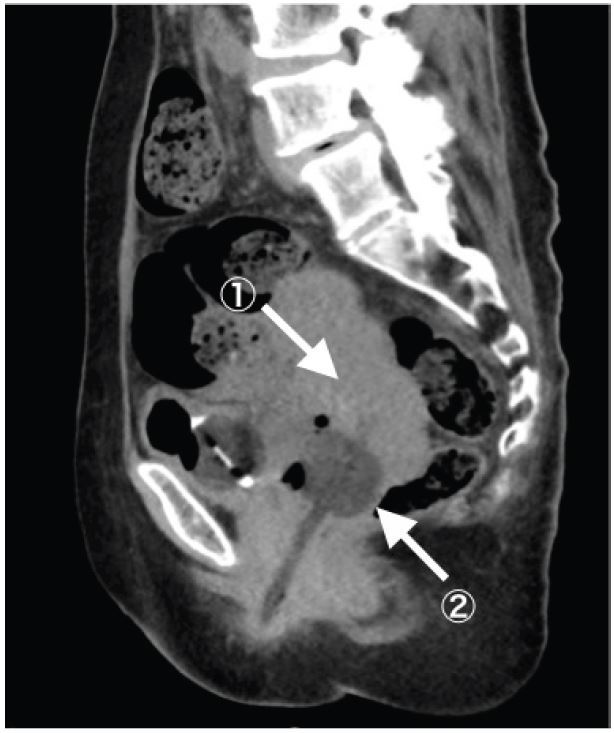
A 67-year-old woman complaining of continuous fresh vaginal hemorrhage came to our emergency department in a pre-shock state. Examinations revealed an irregularly shaped mass in the uterus and active arterial bleeding. Emergent hysterectomy and interventional radiology were not immediately available. Foley catheter with 20mL water was inserted into the uterine cavity, then the balloon was pulled to obstruct the uterus output (Figure). Her vital signs became stabilized, and she was transferred to another hospital two days later.
DIAGNOSIS AND DISCUSSION
A 67-year-old patient was diagnosed as Stage IIb cervical carcinoma. In this case, we controlled active bleeding from cervical cancer by balloon tamponade technique, which is frequently used in obstetric postpartum hemorrhage as a noninvasive and fertility-sparing procedure.1 Although devices specially made for obstetric hemorrhages are frequently used, less expensive and more easily accessible devices such as Foley catheters and condom catheters are also used.2,3 Only one case has ever been reported with this procedure used for hemorrhage from gynecologic malignancies.4 In this case, we were able to achieve sufficient tamponade effect using a single quite-small volume balloon, probably because the tumor itself and coagulated blood almost filled the uterine cavity.
Similar tamponade techniques are commonly used by emergency physicians for several emergency hemorrhages, such as vaginal, nasal, esophageal, or urethral hemorrhage, which usually require procedures performed by each specialty physician afterwards. Such balloon tamponade techniques are valuable as a bridge to specialty treatment because they can be conducted easily by emergency physicians using easily accessible devices.
Footnotes
Section Editor: Sean O. Henderson, MD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Tomohiro Sonoo, MD, The University of Tokyo Hospital, 7-3-1, Hongo, Bunkyo-ku, Tokyo, Japan 1138655. Email: sonot-icu@h.u-tokyo.ac.jp. 9 / 2015; 16:793 – 794
Submission history: Revision received July 11, 2015; Accepted July 17, 2015
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Georgiou C. Balloon tamponade in the management of postpartum haemorrhage: a review. BJOG. 2009;116(6):748-57.
2. De Loor JA, van Dam PA. Foley catheters for uncontrollable obstetric or gynecologic hemorrhage. Obstet Gynecol. 1996;88(4 Pt 2):737.
3. Bagga R, Jain V, Sharma S, et al. Postpartum hemorrhage in two women with impaired coagulation successfully managed with condom catheter tamponade. Indian J Med Sci. 2007;61(3):157-60.
4. Kyrgiou M, Martin-Hirsch P, Singh M. The use of a Rusch intrauterine balloon to cause tamponade on a severe hemorrhage in a case of endometrial cancer. Int J Gynecol Cancer. 2014;24(5):946-9.


