| Author | Affiliation |
|---|---|
| Kashyap Tadisina, BS | University of Illinois at Chicago, School of Medicine, Chicago, Illinois |
| Ariane Abcarian, MD | University of Illinois at Chicago, Department of Surgery, Chicago, Illinois |
| Ellen Omi, MD | Advocate Christ Medical Center, Department of Trauma Surgery, Oak Lawn, Illinois |
Introduction
Case report
Discussion
Conclusion
ABSTRACT
Fireworks are used to celebrate a variety of religious, patriotic, and cultural holidays and events around the world. Fireworks are common in the United States, with the most popular holiday for their use being national Independence Day, also known as July Fourth. The use of fireworks within the context of celebrations and holidays presents the ideal environment for accidents that lead to severe and dangerous injuries. Injuries to the face from explosions present a challenging problem in terms of restoring ideal ocular, oral, and facial function. Despite the well documented prevalence of firework use and injury, there is a relatively large deficit in the literature in terms of firework injury that involves the face. We present a unique case series that includes 4 adult male patients all with severe firework injuries to the face that presented at an urban level 1 trauma center. These four patients had an average age of 26.7 years old and presented within 5 hours of each other starting on July Fourth. Two patients died from their injuries and two patients underwent reconstructive surgical management, one of which had two follow up surgeries. We explore in detail their presentation, management, and subsequent outcomes as an attempt to add to the very limited data in the field of facial firework blast injury. In addition, the coincidence of their presentation within the same 5 hours brings into question the availability of the fireworks involved, and the possibility of similar injuries related to this type of firework in the future.
INTRODUCTION
Fireworks are used worldwide to celebrate a variety of religious, patriotic, and cultural holidays and events. Fireworks are extremely common in the United States (U.S.), with the most popular holiday for fireworks being national Independence Day, also known as July Fourth. We present a unique case series that includes 4 adult male patients, all with firework injuries to the face, who presented within 5 hours of each other during the July Fourth holiday at an urban level 1 trauma center. We explore in detail their presentation, management, and subsequent outcomes as an attempt to add to the very limited data in the field of facial firework blast injury.
CASE REPORT
Case 1
Patient 1 is a 26-year-old male that was transferred from an outside hospital secondary to a firework blast to the face. He was described as alert but “restless” upon presentation. The outside hospital physician was not able to intubate the patient after 2 attempts and a cricothyroidotomy was performed at the outside hospital for airway protection. He was hypoxic and tachycardic the majority of the time at the outside hospital. During transport the patient became asystolic and his blood pressure dropped. En route, the patient was started on dopamine drip, and percutaneous pacing was initiated. Upon arrival at the emergency department (ED), his cricothyroidotomy was in place and he was in pulseless electrical activity. His Glasgow Coma Scale (GCS) score was a 3T. Advanced cardiovascular life support was initiated and 3 rounds of epinephrine were given without return of spontaneous circulation. The patient was pronounced dead shortly after his rhythm deteriorated to asystole.
Case 2
Patient 2 is a 23-year-old male transferred from an outside hospital after being hit in the face from a firework blast. Upon presentation to our institution, the patient had a GCS score of 9T and he was intubated using direct laryngoscopy on the second attempt. Etomidate and succinylcholine were given as the sedative and paralytic. He had extensive injury to his forehead, frontal head, orbits, with exposed facial bones. His face was covered with abrasions and lacerations, his right cornea was burned, and the left eye was ruptured. The patient’s vital signs were stable.
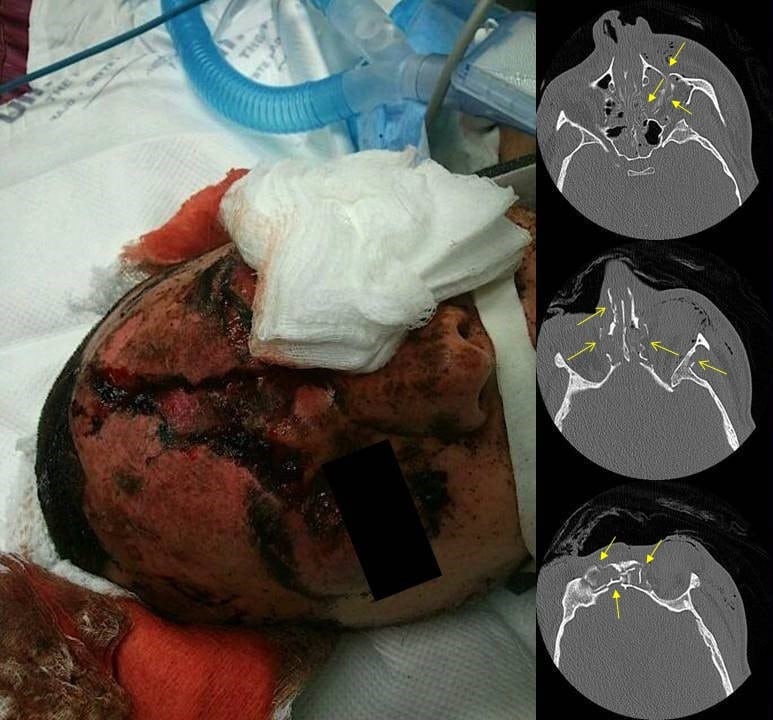
Figure 1
Patient 2 upon presentation with computed tomography of the head (axial view). Multiple facial fractures (arrows).
A computed tomography (CT) of the head and face revealed a 5 mm left frontal epidural with a complex frontal sinus fracture involving the posterior wall of the sinus. Extensive facial fractures were noted involving the paranasal sinuses, the nasal orbital ethmoidal complex, the planum sphenoidale, and the left greater wing of the sphenoid. The left eye was ruptured.
Ophthalmology, neurosurgery, and plastic surgery services were consulted. Ophthalmology took the patient immediately to the operating room (OR) for enucleation of the left eye. Neurosurgery found that there was no surgical intervention appropriate at the time, and plastic surgery deferred any reconstruction until the patient stabilized.
The patient was then admitted to the intensive care unit (ICU), started on dilantin for seizure prophylaxis, and continued on antibiotics for the open wound to the forehead. He was extubated on the third day in the hospital. The patient also sustained a large soft tissue defect to forehead, requiring debridement in OR on the sixth hospital day.
While an inpatient, the patient required pain control, intravenous antibiotic therapy, and physical and occupational therapy. He was discharged and his wounds healed, but he declined further surgery. This patient was lost to follow up after his initial outpatient follow up.
Case 3
Patient 3 is a 30-year-old male who presented to the ED from the field with extensive facial trauma secondary to a firework blast to the face. His airway was secured immediately upon arrival due to an altered mental status with a GCS of 3 and poor oxygenation. A glidescope intubation with a size 7 tube was performed, with almost immediate replacement of a size 8 tube when an air leak was found. Exchange of the endotracheal tube was guided with the help of a bougie. He was hypotensive initially and had episodes of bradycardia. The hypotension responded to fluids. He had extensive facial blast injury with a large amount of tissue loss of the eyes, forehead and nose. Both of the eyes were clinically ruptured. The maxilla was unstable upon examination. Focused assessment with sonography for trauma was performed and no free fluid was found. Ophthalmology, neurosurgery, and plastic surgery services were consulted.
Figure 2
Preoperative view of patient 3 with computed tomography of the head (axial view). Multiple facial fractures (arrows).
CT head revealed diffuse cerebral edema with effacement of the 3rd and 4th ventricles, subarachnoid hemorrhage and bilateral frontal and temporal contusions. CT maxillofacial revealed multiple complex fractures as follows: frontal bone with a comminuted fracture involving the inner and outer table and displacement of both; large defect noted in the anterior and central skull base with destruction of the ethmoid complex and the sphenoid bone; left temporal bone fracture with involvement of the inner ear and mastoid sinus; bilateral orbital, pterygoid, zygomatic and maxillary sinus fractures; fracture of the hard palate with obvious diastases of the bone fragments; and a mandibular body fracture. In addition the CT of the face revealed bilateral globe ruptures with extensive edema of the ophthalmic nerves and extraocular muscles.
The patient was admitted to the ICU. Consultation of neurosurgery, ophthalmology and plastic surgery were obtained. Post injury the patient developed persistent high fevers and was treated with antibiotics, he developed central diabetes insipidus, and was minimally responsive with only a cough and a gag. Eventually he was able to intermittently move his upper and lower extremities with stimulus. No surgical intervention was planned for his injuries.
On hospital day six, the patient underwent tracheostomy, percutaneous endoscopic gastrostomy tube placement, and facial wound debridement, all of which were uneventful. On hospital day seven, the patient had an increasing pressor requirement and fevers. His responsiveness also diminished after the operating room and it was thought that he progressed to brain death. He was in the middle of a brain death workup when he went into cardiac arrest. After 3 cycles of cardiopulmonary resuscitation, the patient was pronounced dead.
Case 4
Patient 4 is a 28-year-old male that was hit in the face by a firework described as a mortar. The patient was described as being combative during transport by emergency medical services. The patient was not speaking upon arrival, but saturating well on a non-rebreather mask. He was intubated in the ED due to the extensive facial trauma and the risk for loss of airway. Although the patient had lacerations on the mouth, oral intubation with an 8.0 tube was achieved using direct laryngoscopy while maintaining inline stabilization of the cervical spine. The patient was sedated and paralyzed with etomidate and succinylcholine. Glasgow coma scale was 10 (eyes 3, verbal 1, motor 6). Grossly, the patient had a laceration to the scalp, a frontal skull fracture, and avulsion of the left eye. Vital signs remained stable throughout his ED stay and he was admitted to the ICU after his workup was completed.
Figure 3
Patient 4 upon presentation with computed tomography of the head (axial view). Multiple facial fractures (arrows).
CT of the head revealed 3 mm left frontal contusion and bilateral frontal and right parietal subarachnoid hemorrhage. CT maxillofacial revealed multiple facial fractures as follows: bilateral frontal and frontal sinus fractures with involvement of the inner and outer tables; floor roof and lateral wall fractures of the left orbit with absence of the left globe; comminuted ethmoidal, nasal bone and left maxillary sinus fractures; and left sphenoid sinus fracture.
Ophthalmology, Neurosurgery, and Plastic Surgery services were consulted. Ophthalmology removed the remainder of the left globe and orbital debris. Neurosurgery did not offer any surgical intervention and plastic surgery determined that the patient would need reconstruction once stable
On hospital day five the patient underwent tracheostomy and percutaneous endoscopic gastrostomy. The facial wounds were debrided and the midline frontal scalp laceration was repaired. Swallow evaluation done and a soft mechanical diet was started. No progression of his intracranial hemorrhages noted.
On hospital day thirteen, the patient was taken to the OR by ophthalmology and plastic surgery services to begin reconstruction. Left eye enucleation was performed first. The reconstruction of the face included open reduction internal fixation of the left orbital roof and lateral wall, the left maxillary sinus, frontal sinus, left maxilla, upper and lower eyelid reconstruction and repair of complex laceration. On hospital day #21, the patient was discharged home decannulated. This patient had two subsequent operations, the first of which occurred 12 days after discharge. He developed a 1.5 cm dehiscence present at the level of the left orbital rim with exposed plate. A pedicle flap was made based on the previous scar and the area was closed without further difficulty. The second operation was performed 68 days after discharge due to severe contracture development in the left upper and lower eyelid.
DISCUSSION
The American Pyrotechnics Association (APA) estimates that the total firework consumption in 2011 was 234.1 million pounds and total firework revenue for 2011 to be over $950 million dollars.1 The U.S. Consumer Product Safety Commission (CPSC) estimated that 9600 (95% confidence interval of 7600–11600) fireworks related injuries were treated in U.S. ED in 2011 with 65% of the injuries occurring between June 17, 2011 and July 17, 20112. Only four firework related deaths were reported in 2011 by the CPSC, but the Commission states that this is likely an underestimation. All deaths reported were due to either illegal or homemade fireworks.
As defined by the federal explosives laws, fireworks are separated into two broad categories: display and consumer fireworks. Consumer fireworks are those available to the general public and defined by as any small firework device designed to produce visible effects by combustion and which must comply with the construction, chemical composition, and labeling regulations of the U.S. Consumer Product Safety Commission.3 These include rockets, firecrackers, smoke balls, roman candles, sparklers, artillery shells, and air bombs. All consumer fireworks include a trade name and manufacturing information displayed clearly on them. In the state that these patients were treated, firework laws are quite strict, whereas the patients transferred from bordering states are more relaxed. Regardless, the force necessary to cause such damage was likely illegal in either state. Unfortunately, due to the retrospective nature of this study, information regarding the specific firework and method of injury was unavailable for each patient. Previous reports have been sparse in regards to the types of fireworks associated with injuries, making the mechanism and object of injury an important piece of history that can influence the management of these often complicated patients and vital to initial assessment of these patients.
The use of fireworks in the context of celebrations and holidays presents the ideal environment for accidents that lead to severe and dangerous injury. Studies conducted in China and Iran in conjunction with the Chinese annual spring festival and Iranian Last Wednesday Eve Festival respectively have found that private use of fireworks increases the incidence of injury.4,5 Further, the two most common causes of injury with firework were found to be due to illegal firework use and improper handling 4, with no reduction in incidence of firework injury in those with increased socioeconomic or education level. Another survey conducted in Iran found that during festival times, civilians that have a lower perceived injury risk and a higher perceived ability of managing injury were more likely to participate in the use of fireworks and had a higher incidence of injury.6 It can be concluded that firework use and associated injury is an individual choice, making education and awareness of safety and risk reduction methods all the more necessary.
Explosive injuries to the face present a challenging problem in terms of restoring ideal ocular, oral, and facial function.7–9 Firework injury is often associated with extensive soft tissue trauma complicated by fractures, burns, accompanying traumas, and the presence of foreign bodies8. Reconstruction, if deemed necessary, is recommended to be completed as soon as possible after the injury, with the most useful techniques including microsurgical reconstruction, nerve, vessel, and soft tissue grafting, fracture fixation, and the use of free flaps to address large defects9–10.
Despite the well documented prevalence of firework use and injury, there is a relatively large deficit of published work regarding firework injury involving the face. While extensive literature exists characterizing isolated ocular firework trauma11, there are only a few isolated case reports and retrospective studies characterizing other facial firework trauma and subsequent management and reconstruction.8–10 Previous literature describes the most common victims to be male, children, and innocent bystanders.10,11 The most common locations for injury have been found to be the hand and face, with burns being the most common associated injury.10,11
Of the 4 patients that suffered firework blasts to the face, two expired, one immediately upon arrival to the ED and one after spending six days in the ICU, confirming the potentially fatal consequences of firework injuries. One of the 2 surviving patients was handled with debridement and ophthalmologic surgical management, and was discharged after seven days without complication. The other surviving patient had more extensive facial reconstruction, requiring five operations, including enucleation, open reduction and internal fixation, extensive soft tissue repair, along with two follow up surgeries due to dehiscence and contracture formation around the orbit. Despite the survival of two patients, both lost vision in one eye and required multiple follow ups.
Our case report confirms that males are highly likely to be victims of firework injury, although all of them were directly involved with the fireworks and were not innocent bystanders. The average age of victims was 26.7 years old, which is of young adult age, while literature states that children are the most frequent victims of these injuries. Reconstructive techniques documented for our patients match those cited as the most commonly used in the literature, with debridement, open reduction and internal fixation, eye enucleation, Z-plasty, and complex soft tissue repair being used in our patients.
According to Advance Trauma Life Support (ATLS) guidelines (ACS COT)12, one of the most important principles in taking care of patients with such severe facial injuries is management of their airway and a potential avoidance of early preventable death. As demonstrated with these 4 cases, airway management was immediately addressed in each of the patients with one patient receiving a cricothyroidotomy. Given the location and the extent of some of the blast injuries that can occur from fireworks or penetrating injuries to the face, swelling, anatomical distortion, obstruction and aspiration can be a consequence of the injury and an airway can be quickly compromised. When the lower part of the face is involved (i.e. mandible, neck), airway protection often becomes more challenging. In addition, the need for establishment of an airway and mechanical ventilation for airway protection in the event of a concomitant severe head injury is important to avoid exposure of the patient to secondary brain injury as a result of an unstable airway.
One of the most highly characterized areas of facial trauma is that of ocular injury. A recent meta-analysis of ocular blast injuries found that as much as 28% of blast survivors suffer from ocular injury.13 The most common injuries suffered by victims are corneal abrasions, deposition of foreign bodies on the conjunctiva, cornea and fornix, hyphema. Open globe injuries and the presence of intraocular foreign bodies are less prevalent, but are associated with loss of vision, occurring in a majority of patients. Other risk factors for poor visual outcome included poor initial visual acuity, retinal detachment and development of endophthalmitis.13,14 Ocular injuries were found to be most prevalent from secondary blast injuries, resulting not from direct injury to the eye, but from shrapnel and projectile debris, with periorbital location of injury having the highest associated morbidity.13,15
The use of antibiotics perioperatively has been shown to reduce the incidence of surgical site infection and is the current standard of care in elective clean-contaminated head and neck surgery.16,17 The most feared infectious complication in maxillo-facial injuries is meningitis due to the communication of the face with the intracranial space, making surgical site infection prevention an important part of management in these cases. However, there currently exists no guideline for management of surgical traumatic facial injury patients with prophylactic antibiotics. Some literature suggests the use of prophylactic antibiotics in complex traumatic oral and facial wounds.18 However, recent studies have found no difference between infection rates in surgical patients with maxillofacial fractures19 and midface or frontal sinus trauma20 between those who were given prophylactic antibiotics and those who were not. Overall, there is a severe lack of literature to address the use of prophylactic antibiotics for open skull or facial blast injuries. The authors believe that prophylactic antibiotics may have a role in reducing postoperative infection and support their use in complicated and open facial injuries caused by fireworks, but recognize the need for more research into this topic.
The utility of prophylactic antibiotics in basilar skull fractures is also not clear. Ratilal et al21 performed a Cochrane review of antibiotic use in basilar skull fractures with and without cerebrospinal fluid leak and noted there was no difference in the rates of meningitis, all-cause mortality, meningitis-related mortality and need for surgical correction in patient with cerebrospinal fluid leakage. The patients in this case series all had a combination of severe facial injuries and intracranial injury with basilar skull fracture. Even less literature exists regarding the severe combination of injuries that this case series of patients sustained.
Firework injuries to the face are a unique and often times devastating injury scheme in emergency rooms and trauma hospitals. From this case series and review of literature, the authors agree that principles of airway management are of utmost importance for facial firework injury patients’ initial management. Further, the use of prophylactic antibiotics may be useful while patients are undergoing complex surgical reconstruction. However the paucity of information regarding the types of fireworks, mechanism of injury, and individual behavior influenced injury calls for more research and education regarding firework injury to the face in order to prevent future injuries and develop optimal management of these patients.
CONCLUSION
We outline the clinical course and outcomes for four patients that suffered firework blast injuries to the face. As previously described, firework blast injuries can prove to be very dangerous to patients, with fatal outcomes, and patients often prove to be challenging and complicated in their surgical management when surgery is deemed necessary. In describing these patients, we hope to shed light on a severely under published area of the literature and guide future research, investigative work, and clinical/surgical management of these patients. In the United States, fireworks have various regulations of sale depending on the state. These patients came from both a state which has laws against fireworks and one which has very little restriction. In addition, with the presence of individuals in combat areas and the age where explosives are sadly becoming more frequent, management of facial blast injuries and firework injuries are only going to become more prevalent.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Ellen Omi, MD. Advocate Christ Medical Center, 4440 W 95th St Suite 1835, Oak Lawn, IL 60453. Email: eomil@uic.edu. 7 / 2014; 15:387 – 393
Submission history: Revision received September 28, 2013; Submitted January 5, 2014; Accepted January 10, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.