| Author | Affiliation |
|---|---|
| Tiffany Jan, MD | University of Chicago, Department of Emergency Medicine, Chicago, Illinois |
| Jorge del Castillo, MD, MBA | University of Chicago, Department of Emergency Medicine, Chicago, Illinois NorthShore University Healthsystem, Department of Emergency Medicine, Evanston, Illinois |
ABSTRACT
The following is a case of Charles Bonnet syndrome in an 86-year-old woman who presented with visual hallucinations. The differential diagnosis of visual hallucinations is broad and emergency physicians should be knowledgeable of the possible etiologies.
INTRODUCTION
Visual hallucinations are not a common presentation in the emergency department (ED). However, emergency physicians should be adept in differentiating between various causes. Patients who present with this neuro-ophthalmologic dysfunction carry a broad differential diagnosis. This usually results in an extensive evaluation, including neuro-imaging, laboratory testing, and consultation with pertinent specialties, such as neurology or psychiatry. While there are many serious causes of visual hallucinations, in this case report we present an unusual yet benign etiology for visual hallucinations.
CASE REPORT
An 86-year-old woman presented to the ED with a chief complaint of visual hallucinations. She had been having these “visions” for a week, occurring mainly in the evening. The hallucinations were episodic, binocular and lasted for hours. She was unable to identify any specific factors that would trigger their arrival or resolution.
The hallucinations were clear and vivid, representing either various objects around the house moving, such as a clock and a planter, or people and faces on the ceiling or corner of her room. She had become so frightened thinking she was “going crazy” that she decided to come to the ED. While experiencing these hallucinations, the patient had no change in mental status and maintained full insight and awareness. She denied any other visual disturbances, such as diplopia, scotomata, tunnel vision or loss of vision. She further denied auditory or other sensory hallucinations as well as headaches, fever, or trauma. There was no history of drug or alcohol abuse.
Her past medical history included open-angle glaucoma, macular degeneration, cataracts, hypothyroidism, hyperlipidemia and gastric reflux. Her surgical history was relevant for bilateral cataract surgeries with her right eye requiring 2 surgeries, as well as a corneal transplant. She denied any psychiatric history.
On physical examination she appeared well and in no acute distress. She was oriented to person, place and time. Her vital signs were: blood pressure 213/98 mmHg, pulse rate 66 beats/minute and regular, respirations 20 breaths/minute, temperature of 36.8°C and oxygen saturation of 97% on room air. There were no complaints of any hallucinations at the time of the exam. She had bilateral iridectomies and her corrected visual acuities were 20/50 OD and 20/100 OS. The visual fields were full, and her fundoscopic exam revealed no gross abnormalities. Neurologic examination showed no focal findings. A mental status examination did not reveal mood disturbance or cognitive deficits, and she scored 30/30 points on her Mini Mental Status Exam (MMSE). The remainder of her physical examination was normal.
Laboratory studies demonstrated a serum sodium level of 128 mEq/L and a serum chloride of 92 mEq/L. Glucose and renal function were normal. White blood cell count was 8.3 × 109/L. A urinalysis was positive for nitrites, 2+ leukocyte esterase and 50–100 white blood cells/HPF. Computed tomography (CT) of the head without contrast showed no acute intracranial hemorrhage, stable moderate to marked chronic microvascular ischemic changes in the supratentorial white matter, and a stable small chronic infarct in the right basal ganglia.
Based on clinical history and exam, a diagnosis of Charles Bonnet syndrome was made by the ED attending physician. She was seen 2 days later by her ophthalmologist who concurred with the ED diagnosis based on similar presentation of many previous patients in his practice. At the time of her follow up, the hallucinations had resolved and her eye exam was unremarkable.
DISCUSSION
There are many etiologies for visual hallucinations, which include retinal disease, migraines, acute stroke, drug-related side effects, neurodegenerative disease, alcohol and/or drug use, toxic-metabolic encephalopathy and psychiatric illness. Visual hallucinations can be categorized as simple or complex. Simple hallucinations involve basic imagery, such as lights, colors, lines and shapes, whereas complex hallucinations include images of people, objects or specific scenes. Classifying the type of visual hallucinations can help narrow the differential diagnosis, thereby aiding in accurately diagnosing the patient’s underlying condition. Other features that should be delineated are the presence versus absence of insight, monocular versus binocular involvement, amount of visual field involvement, triggers, frequency and duration.
Charles Bonnet syndrome is an uncommon condition causing visual hallucinations in patients without mental illness. Charles Bonnet, a Swiss philosopher, first described the syndrome in 1760 in a publication describing visual hallucinations experienced by his grandfather who was blind secondary to cataracts.1 However, it was not until 1967 that a Swiss scientist, George de Morsier, labeled the condition as Charles Bonnet syndrome.2Since then, a number of case reports have been described in the ophthalmology and psychiatry literature.3
The neurophysiology explaining the visual hallucinations in Charles Bonnet syndrome is not clearly elucidated. The currently accepted theory suggests that vision loss leads to visual sensory de-afferentation, causing disinhibition, and later spontaneous firing, of the visual cortical regions.7 Visual deprivation experiments have resulted in similar hallucinations, and functional magnetic resonance imaging (MRI) in patients with Charles Bonnet syndrome has found an association with visual hallucinations and spontaneous activity of the ventral occipital lobe.8
The majority of patients with Charles Bonnet syndrome are elderly with a mean age of 70–85 years. However, cases have been reported in all age groups. Identifying the exact prevalence of Charles Bonnet syndrome is difficult, and the number differs widely among various studies.3,4 This uncertainty and inconsistency is likely due to two main causes: underreporting of symptoms and misdiagnosis. Up to 60% of patients with Charles Bonnet syndrome are hesitant to tell their physician about their visual hallucinations for fear of being labeled with a mental illness or dementia.6 Misdiagnosis is also common as the syndrome is not recognized by clinicians and often labeled as psychosis, delirium or early dementia.
Patients with Charles Bonnet syndrome are also likely to have a history of diminished visual acuity or visual field loss. Both this and elderly age were found to be the primary factors correlated with Charles Bonnet syndrome.5 Visual deficits are generally the result of macular degeneration, cataracts, glaucoma or diabetic retinopathy. Patients possess insight into the unreality of their visual experiences, which are commonly pleasant but may cause significant anxiety.
The visual hallucinations of Charles Bonnet syndrome may be simple or complex. The characteristic features of these images are not associated with the specific anatomical location of the ocular injury. However, they will typically correspond to the area of visual loss, whether that localizes to a certain visual field or are monocular versus binocular.9These images are typically well-defined, clear, and lack personal meaning or impact to the patient. Hallucinations will occur more frequently with eyes open and will disappear when the eyes close or visual gaze changes.3 One study also showed that hallucinations appeared more often during periods of sensory deprivation, such as inactivity or evening and nighttime.9 The duration of hallucinations will vary from continuous to less than one minute, but most patients report duration of several minutes occurring multiple times a day or week.7
Symptoms caused by Charles Bonnet syndrome cannot be explained by the presence of a psychiatric disorder, and patients do not have any significant metabolic derangements or impaired sensorium that would otherwise explain the symptoms. Although Charles Bonnet syndrome has no official diagnostic criteria, the features described are generally accepted and can be used as guidelines to make the diagnosis when appropriate (Table 1). A patient presenting to the ED with symptoms suggestive of Charles Bonnet syndrome should receive basic laboratory tests, such as a metabolic panel and complete blood count along with neuro-imaging, typically with CT without contrast. MRI could be considered, although it would likely be most appropriate in the outpatient setting.
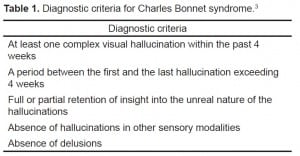
Diagnostic criteria for Charles Bonnet syndrome
Our patient had the characteristic features with her age and history of vision loss. She also had full insight into the fictional nature of her hallucinations and met the diagnostic criteria of Charles Bonnet syndrome discussed previously. However, our patient also presented with hyponatremia and a urinary tract infection, although these findings were unlikely to be the cause of her symptoms. At a level of 128 mEq/L, her hyponatremia would typically be considered mild. Most neurological manifestations of hyponatremia occur at levels of < 115 mEq/L, and it would be unlikely for a patient with a serum sodium of 128 mEq/L to exhibit visual hallucinations without other changes in mental status as the only symptom of her hyponatremia. The urinary tract infection was a subclinical diagnosis as our patient had no symptoms. She also had no risk factors of a complicated infection, such as a recent catheterization, residence in a nursing home, or an immuno-compromised status. In contrast, she was a high functioning and independent octogenarian. In these circumstances, it would be unlikely that the infection was the primary cause of the patient’s visual hallucinations with no other neurologic changes or confusion. However, it is possible that these abnormalities could have contributed in exacerbating her symptoms, although this would be difficult to fully assess.
Currently, there is no universally accepted treatment for Charles Bonnet syndrome. Visual hallucinations often resolve once the underlying cause of vision loss is rectified. Unfortunately, in some cases, they can be persistent for several years.10 In these scenarios, patients can learn how to suppress hallucinations and improve quality of life. Clinicians can encourage patients to heighten visual stimulation, either with increased arousal through social interaction or activity or rapid eye movements, both of which can reduce hallucinations.2,11
Anecdotally, typical and atypical antipsychotics have shown benefit in individual patients, although there is little evidence to support this and may not outweigh the risks of side effects or interactions with other medications.4 Atypical antipychotic medications such as Risperidone (Risperdal), Quetiapine (Seroquel) and Olanzapine (Zyprexa) have been used with varying success.
Often times, the cause of the hallucinations is more distressing to the patient than the actual hallucinations, and therefore reassurance from the provider can make patients more comfortable without pharmacologic treatment.13
Once the diagnosis of Charles Bonnet syndrome is made in the ED, the provider can reassure the patient and provide suggestions to suppress hallucinations as mentioned previously. Any metabolic abnormalities should be corrected to prevent potential exacerbations of symptoms. Referral to an ophthalmologist for follow up would be appropriate, especially if visual acuity correction is needed. Patients can typically be discharged safely without any prescriptions and follow up with their primary care provider to assess whether further diagnostic work up, such as MRI or a trial of an antipsychotic medication, would be necessary.
Another closely related diagnosis that should be considered in patients that present with acute onset of visual hallucinations is Lhermitte’s hallucinosis, otherwise known as peduncular hallucinosis. Similar to Charles Bonnet syndrome, Lhermitte’s hallucinosis is more commonly attributed to the elderly. The visual hallucinations in Lhermitte’s hallucinosis are vivid, well-formed, and usually are recognized to be unreal. In contrast though, Lhermitte’s hallucinosis is associated with dementia, with correlated lesions or infarcts in the midbrain or brainstem on neuro-imaging.13 Also, many patients will demonstrate other neurological findings, reflecting deficits from prior cerebrovascular injuries. In a case series of 5 patients with Lhermitte’s hallucinosis, all patients were found to have decreased MMSE scores, and patients had intermittently displayed periods of confusion and disorientation. Furthermore, visual hallucinations were accompanied by various deficits in higher cortical functioning, including memory deficits, agnosia and dysarthria.13,14 Although our patient did not undergo a MRI, the absence of any cognitive deficits or episodes of confusion made this diagnosis unlikely. Lhermitte’s hallucinosis should be included in the differential when evaluating patients similar to the one described in this case report.
CONCLUSION
Charles Bonnet syndrome should be considered in all elderly patients who present with visual hallucinations. However, more serious causes of hallucinations should be considered and ruled out, as Charles Bonnet syndrome is a clinical diagnosis of exclusion. As our society ages, EPs are likely to encounter this diagnosis with greater frequency as vision problems such as cataracts and macular degeneration become more common. Although Charles Bonnet syndrome is benign, the visual hallucinations can cause great anxiety for patients. Therefore, increased awareness of this condition can assist clinicians in proper diagnosis, counseling and reassurance of their patients.
Footnotes
Supervising Section Editor: Rick A McPheeters, DO
Submission history: Submitted April 23, 2012; Revisions received June 27, 2012; Accepted July 09, 2012
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.7.12891
Address for Correspondence: Tiffany Jan, MD, University of Chicago, Department of Emergency Medicine, 5841 S. Maryland Ave, MC 5068, Chicago, IL 60637
Email: Tiffany.Jan@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Damas-Mora J, Skelton-Robinson M, Jenner FA. The Charles Bonnet syndrome in perspective. Psychological Medicine. 1982;12:251–261. [PubMed]
2. Kester EM. Charles Bonnet syndrome: case presentation and literature review.Optometry. 2009;80:360–366. [PubMed]
3. Teunisse RJ, Zitman FG, Cruysberg JR, et al. Visual hallucinations in psychologically normal people: Charles Bonnet syndrome. Lancet. 1996;347:794–797. [PubMed]
4. Hartney KE, Catalano G, Catalano MC. Charles Bonnet syndrome: are medications necessary? Journal of Psychiatric Practice. 2011;17:137–141. [PubMed]
5. Teunisse RJ, Cruysberg JR, Verbeek ALM, et al. The Charles Bonnet syndrome: a large prospective study in The Netherlands. A study of the prevalence of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijmegan. British Journal of Psychiatry. 1995;166:254–257.[PubMed]
6. Yacoub R, Ferrucci S. Charles Bonnet syndrome. Optometry. 2011;82:421–427.[PubMed]
7. Fiabins PV. The genesis of phantom (deenervation) hallucinations: a hypothesis.International Journal of Geriatric Psychiatry. 2004;9:775–777.
8. Ffytche DH, Howard RJ, Brammer MJ, et al. The anatomy of conscious vision: an fMRI study of visual hallucinations. Nature Neuroscience. 1998;1:738–742.
9. Menon GJ, Rahman I, Menon SJ, et al. Complex visual hallucinations in the visually impaired: the Charles Bonnet syndrome. Survey of Ophthalmology. 2003;48:58–72.[PubMed]
10. Schultz G, Meizack R. The Charles Bonnet syndrome: ‘phantom visual images.’Perception. 1991;20:809–825. [PubMed]
11. Schadlu A, Schadlu R, Shepherd JB. Charles Bonnet syndrome: a review. Current Opinion in Ophthalmology. 2009;20:219–222. [PubMed]
12. Menon GJ. Complex visual hallucinations in the visually impaired: a structured history-taking approach. Archives of Ophthalmology. 2005;123:349–355. [PubMed]
13. Leo RJ, Ahrens KS. Visual hallucinations in mild dementia. A rare occurrence of Lhermitte’s hallucinosis. Psychosomatics. 1999;40:360–363. [PubMed]
14. Benke T. Peduncular hallucinosis: A syndrome of impaired reality monitoring.Journal of Neurology. 2006;253:1561–1571. [PubMed]


