| Author | Affiliation |
|---|---|
| Eric R Schmitt, MD, MPH | Harbor-UCLA Medical Center, Department of Emergency Medicine, Torrance, California |
| Michael D Burg, MD | Kaweah Delta Medical Center, Department of Emergency Medicine, Visalia, California |
A 25-year-old male presented to the emergency department with 1 week of progressive right-sided chest pain. The pain was sharp, radiated to the back, and worse with deep inspiration. He denied dyspnea and leg pain or swelling. The patient’s medical history was remarkable for a lower extremity deep vein thrombosis diagnosed 6 months prior. He’d self-discontinued anticoagulant therapy 2 months prior. Blood pressure was 131/66 mmHg, heart rate 76 beats per minute, respiratory rate 20 breaths per minute, temperature 36.4°C, and oxygen saturation 99% on room air. Physical examination was essentially unremarkable. Chest radiograph, urinalysis, and blood count were normal; basic chemistry was normal, except for glucose of 111 mg/dL; D-dimer was elevated at 1,485 μg/L.
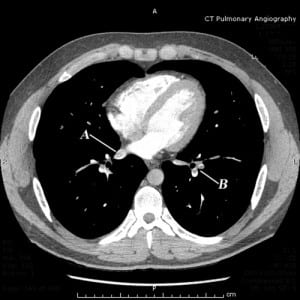
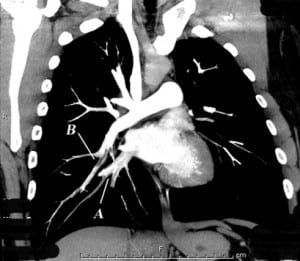
A computed tomographic pulmonary angiogram (CTPA) was performed using a 64-slice machine and read by a staff radiologist as showing a pulmonary vein thrombosis (PVT) and a pulmonary artery embolism (Figures 1 and and2).2). A clot was also identified in the azygos vein (Figure 3). Anticoagulation was begun, and the patient was admitted. The inpatient workup for an underlying prothrombotic state was negative, including negative screen for anticardiolipin antibodies, lupus anticoagulant, and activated protein C resistance, which is found in patients with factor V Leiden; normal levels of protein S and antithrombin III. Protein C was slightly elevated at 182% (70–130%). It is unclear if the patient was tested for a prothrombin gene mutation. The patient was discharged on hospital day 3. A CTPA 7 days after hospital discharge showed no remaining arterial or venous thrombus.

PVT is an uncommon complication of lung transplantation, lobectomy, and primary and secondary tumors of the lung.1 Case reports describe PVT following radiofrequency ablation for atrial fibrillation and repair of type B aortic dissection.2,3 Our patient had none of these conditions, nor had he recently undergone any medical or surgical procedures. Rare idiopathic cases are described as well.4,5 Thrombosis of the azygos vein has been described and in 1 case was associated with pulmonary embolism, but in all these cases, an underlying aneurysm of the vein was present. This was not the case in our patient.6–8
Presenting findings associated with PVT are nonspecific and include: fever, chest pain, dyspnea, cough, hemoptysis, hypoxia, and isovolemic opacification (an infiltrate without volume loss, ie, not atelectasis) on chest radiograph.1,4 Evidence of embolization to the peripheral circulation—splenic infarction and bilateral femoral artery occlusion—has also been reported.5,9
According to published reports, PVT has been diagnosed by angiography or echocardiography.1,4,9PVT may also be diagnosed with a contrast-enhanced chest computed tomography and magnetic resonance imaging.5 However, often the diagnosis is established at autopsy or during pathological evaluation of resected necrotic lung tissue.3,4
Conservative management hinges on anticoagulation. Earlier case reports reference the use of antibiotics, but they lack a proven role in the case of pure PVT, absent infection.1,5 Worsening clinical status may indicate lung infarction and embolectomy, or lobe resection may be indicated.1,4
To our knowledge, there is only 1 prior report in the emergency medicine literature of PVT, and our case is the first reported of a PVT presenting concurrently with pulmonary artery embolism and azygos vein thrombosis.10
Footnotes
Supervising Section Editor: Rick A. McPheeters, DO
Submission history: Submitted April 4, 2011; Revision received May 18, 2011; Accepted May 19, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.5.6762
Address for Correspondence: Eric R. Schmitt, MD, MPH
Harbor-UCLA Medical Center, Department of Emergency Medicine, 1000 W Carson St, Box 21, Torrance, CA 90509
E-mail: ericrschmitt@yahoo.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Burri E, Duwe J, Kull C, et al. Pulmonary vein thrombosis after lower lobectomy of the left lung. J Cardiovasc Surg. 2006;47:609–612. [PubMed]
2. Yataco J, Stoller JK. Pulmonary venous thrombosis and infarction complicating pulmonary venous stenosis following radiofrequency ablation. Respir Care. 2004;49:1525–1527. [PubMed]
3. Thelin S, Karacagil S, Grewal P, et al. Surgical repair of type B aortic dissection complicated by early postoperative lung vein and artery thrombosis. Scand Cardiovasc J. 1999;33:248–249.[PubMed]
4. Alexander GR, Reddi A, Reddy D. Idiopathic pulmonary vein thrombosis: a rare cause of massive hemoptysis. Ann Thorac Surg. 2009;88:281–283. [PubMed]
5. Selvidge SDD, Gavant ML. Idiopathic pulmonary vein thrombosis: detection by CT and MR imaging. AJR. 1999;172:1639–1641. [PubMed]
6. Nakamura Y, Nakano K, Fukada T, et al. Surgical exclusion of a thrombosed azygos vein aneurysm causing pulmonary embolism. J Thorac Cardiovasc Surg. 2007;133:834–835. [PubMed]
7. Ishikura H, Kimura S, Fukumura Y, et al. Resection of an azygos vein aneurysm with thrombosis.Gen Thorac Cardiovasc Surg. 2010;58:209–211. [PubMed]
8. Icard P, Fares E, Regnard JF, et al. Thrombosis of an idiopathic saccular azygos aneurysm. Eur J Cardiothorac Surg. 1999;15:870–872. [PubMed]
9. Garcia MJ, Rodriguez L, Vandervoort P. Pulmonary vein thrombosis and peripheral embolization.Chest. 1996;109:846–847. [PubMed]
10. Mumoli N, Cei M. Idiopathic pulmonary vein thrombosis. J Emerg Med. [published online ahead of print May 1, 2010] doi: 10.1016/j.jemermed.2010.03.019.


