| Author | Affiliation |
|---|---|
| Steve C Christos, DO, MS | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, Illinois |
| Bridgette Svancarek, MD | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, Illinois |
| Adam Glassman, MD | Resurrection Medical Center, Emergency Medicine Residency Program, Chicago, Illinois |
A 38-year-old female presented with acute onset epigastric abdominal pain and vomiting. Surgical history included gastric bypass surgery 8 years prior and cesarean delivery. The patient was in severe distress, afebrile, had significant epigastric tenderness with guarding, normal bowel sounds, and no distention or masses.
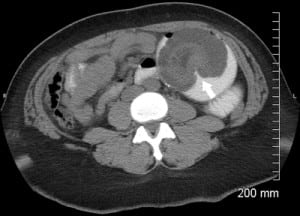
Results for white blood cell count, serum chemistry panel, anion gap, urinalysis, liver function tests, lipase test, and plain radiographs were all normal; computed tomography (CT) of the abdomen/pelvis showed intussusception at the jejunojejunal anastomosis (Figure). The patient underwent resection of the affected bowel segment and had an uneventful recovery.
Roux-en-Y gastric bypass (RYGB) is the most common surgical treatment of morbid obesity in the United States.1–5 The frequency of small-bowel obstruction after laparoscopic RYGB is between 0.2% to 4.5% and can occur months to years after the procedure.1,5 Small-bowel obstruction in these patients is usually caused by adhesions, internal hernias, and rarely, intussusception.1–5Intussusception must be considered because ischemia and necrosis of the affected bowel segment can occur.5
Clinical presentation can be acute or subacute (recurrent vague abdominal pain) and is variable (most patients do not appear ill). The most common presentation is vague abdominal pain, nausea, and vomiting.4 Severity of pain is usually out of proportion to physical examination. Lack of obstruction symptoms does not rule out intussusception.
Findings on plain radiographs are often negative.1,5 CT of the abdomen and pelvis (oral and intravenous contrast) is the diagnostic test of choice, with an accuracy of 80%. Pathognomonic findings include a “target sign” (Figure).5 Patients with a history of gastric bypass surgery, persistent abdominal pain, and a negative CT finding still require surgical evaluation and possibly surgical exploration.1,5 Blind nasogastric tube placement can lead to perforation at the gastrojejunostomy.1Treatment is surgical intervention, usually with resection of the affected bowel segment and reconstruction of a new jejunojejunostomy distally.1 Recurrences can occur after surgical repair.1
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted April 19, 2011; Revision received April 23, 2011; Accepted April 25, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.4.6775
Address for Correspondence: Steve C. Christos, DO, MS
Resurrection Medical Center, Emergency Medicine Residency Program, 7435 W Talcott, Chicago, IL 60631
E-mail: stevesfmc@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Efthimiou E, Court O, Christou N. Small bowel obstruction due to retrograde intussusception after laparoscopic roux-en-y gastric bypass. Obes Surg. 2009;19:378–380. [PubMed]
2. Al-Sabah S, Christou N. Intussusception after laparoscopic roux-en-y gastric bypass. Surg Obes Relat Dis. 2008;4:205–209. [PubMed]
3. Coster DD, Sundberg SM, Kermode DS, et al. Small bowel obstruction due to antegrade and retrograde intussusception after gastric bypass: three case reports in two patients, literature review, and recommendations for diagnosis and treatment. Surg Obes Relat Dis. 2008;4:69–72. [PubMed]
4. Lessmann J, Soto E, Merola S. Intussusception after roux-en-y gastric bypass for morbid obesity.Surg Obes Relat Dis. 2008;4:664–667. [PubMed]
5. Zainabadi K, Ramanathan R. Intussusception after laparoscopic roux-en-y gastric bypass. Obes Surg. 2007;17:1619–1623. [PubMed]


