| Author | Affiliation |
|---|---|
| Thomas Edward Carter, DO | Southern Ohio Medical Center and Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio |
| Curtis Dee Mortensen, DO | Southern Ohio Medical Center and Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio |
| Salita Kaistha, DO | Southern Ohio Medical Center and Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio |
| Christopher Conrad, DO | Southern Ohio Medical Center and Ohio University Heritage College of Osteopathic Medicine, Athens, Ohio |
| Godwin Dogbey, PhD | Ohio University Heritage College of Osteopathic Medicine, Research Office of the Centers for Osteopathic Research and Education, Athens, Ohio |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction:
Needle decompression of a tension pneumothorax can be a lifesaving procedure. It requires an adequate needle length to reach the chest wall to rapidly remove air. With adult obesity exceeding one third of the United States population in 2010, we sought to evaluate the proper catheter length that may result in a successful needle decompression procedure. Advance Trauma Life Support (ATLS) currently recommends a 51 millimeter (mm) needle, while the needles stocked in our emergency department are 46 mm. Given the obesity rates of our patient population, we hypothesize these needles would not have a tolerable success rate of 90%.
Methods:
We retrospectively reviewed 91 patient records that had computed tomography of the chest and measured the chest wall depth at the second intercostal space bilaterally.
Results:
We found that 46 mm needles would only be successful in 52.7% of our patient population, yet the ATLS recommended length of 51 mm has a success rate of 64.8%. Therefore, using a 64 mm needle would be successful in 79% percent of our patient population.
Conclusion:
Use of longer length needles for needle thoracostomy is essential given the extent of the nation’s adult obesity population.
INTRODUCTION
Tension pneumothorax is a devastating and fatal injury pattern that requires the rapid removal of air via needle decompression of the thoracic cavity as an essential lifesaving technique.1 The current American College of Surgeons Advanced Trauma Life Support (ATLS) guidelines advocate the use of a 51 mm (2 inch) needle for needle decompression for tension pneumothoraces.1 The United States is experiencing an increasing problem with obesity, Inaba et al2 discussed alternate sites for decompression based on computed tomography (CT) and postulated a change in site of needle decompression. Air collects anteriorly in the supine patient in addition to scar tissue, breast tissue, hemothorax. Placement of the needle in the abdominal cavity, a solid organ, or the heart, would limit the use of a change of site for this blind technique. Two other studies were published with similar hypotheses and design in Canada and Japan, both of which have a smaller percentage of adult populations suffering from obesity.3,4 All 3 of these studies focused on trauma populations that are predominately young males with primarily penetrating injuries. As a result of sampling bias away from the general population, these studies’ assertions relating to medical causes of pneumothorax are limited.2–4 Our rural patient population has a preponderance of obese patients exceeding Ohio’s average of 29%.5 If an insufficient needle length were used to access the thoracic cavity the patient wound could not be temporized for definitive treatment of a tension pneumothorax, which could result in increased fatalities. Based on a review of the literature and clinical experience, our hypothesis was that the ATLS recommended needle length of 51 mm would not be sufficient in 90% of our patients.6–9
METHODS
With local institutional review board approval as an exempt study, we queried a retrospective database of 100 sequential patients from November 1, 2010 to November 19, 2010 who had chest CTs in a 180-bed community hospital in Appalachia. Statistical power analysis suggested a sample size of at least 70 complete records to detect moderate differences between the chest wall depth and the needle lengths as significant with 80% power. We reviewed the 100 records to ensure that the study was not statistically powered in case there were incomplete records. Inclusion criteria were adult patients (18 years or older) requiring a chest CT. Only the first CT in the date range selected was used (if the patient received more than 1 CT during the time period). Exclusion criteria involved those under the age of 18, subsequent chest CTs of the same patient, marked subcutaneous emphysema, and those with a chest wall tumor. We measured the average chest wall depth at the anterior second intercostal space at the mid clavicular line bilaterally. Three abstractors, comprised of 2 resident physicians and 1 college student, obtained the measurements. Questions of exclusion were handled by quorum of the 2 resident physicians and the attending research advisor. The variables were well defined and the abstractor group was very small; hence, no measure of inter-rater reliability was tested. We recorded chest wall depth measurements of 91 subjects who met inclusion criteria in Microsoft Excel and then analyzed the data using PASW 18 software (SPSS Inc., Chicago, IL) to the various needle lengths (46, 51, and 64 mm) using a combination of statistical methods, including the one-sample t-test, simple linear egression, and ANOVA. Statistical significance was set at p≤0.05.
RESULTS
A 46 mm needle reached the pleural space in 52.7% of our patient sample. This was not statistically different from the patient average chest wall depth of 45.98 mm. (p=0.996, 95% confidence interval [CI]: −4.31 to 4.29). Current ATLS guidelines recommend a 51 mm (2 in) needle, which would reach the pleural space in only 64.8% of our population.1 This was significantly different from the combined average chest wall depth of 45.98 mm (p=0.023, 95% CI: −9.32 to −0.71). Furthermore, it was found that using a 64 mm needle would reach the pleural space in 79% of our patients. Indeed, the 64 mm is statistically significantly higher than the combined average chest wall depth 45.98 mm in our patient sample (p=0.000, 95% CI: −22.31 to −13.70). A comparison of success rates based on needle length is shown in the figure. The table provides summary measures such as the mean and standard deviation of the patient population for height in feet, weight in kilograms, body mass index and chest wall depths in millimeters.
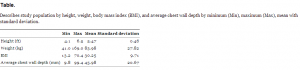
Describes study population by height, weight, body mass index (BMI), and average chest wall depth by minimum (Min), maximum (Max), mean with standard deviation.
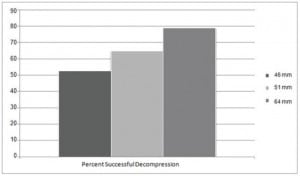
Depicts the success rates with different lengths of needles used for decompression of tension pneumothroax.
DISCUSSION
We failed to reject our study hypothesis based on the statistical significance between the ATLS- recommended needle length of 51 mm and our patient average chest wall depth of 45.98 mm. However, the non-significance between the currently-stocked 46 mm needle and the chest depth wall of 45.98 mm indicated that the stocked needles are not comparatively adequate in reaching the pleural space in our patient population. These results suggest that our current equipment is not sufficient for success in 90% of our patient population.2,7,9,10 The results indicate that a 64 mm needle will offer success in the majority of our patient population however a success rate of 79% is unlikely to be acceptable for the majority of emergency physicians as well as emergency medicine technicians. Given the current obesity epidemic consideration, modifications of many procedural approaches should be considered.
LIMITATIONS
This study is limited by its small sample size and the fact that the geographical region of study is noted for its high obesity rates.5 Elasticity and compressibility of the anterior chest wall with this procedure may lead to higher success rates than static measurements may imply. This error may be negated by movement of the patient, most notably when related to chest compressions for cardiopulmonary resuscitation. The study sample itself could have been changed to review CTs of patients with pneumothorax; however, this is against accepted management of pneumothorax and may be fatal in tension pneumothorax.1 Routine variation in equipment and technique are not addressed. Specifically, the use of a vascular access catheter-based aspiration further shortens the reach of the needle due to the coupling for attaching tubing found on simple catheters and the catheter may collapse or deform more easily when the needle is removed to allow evacuation of air.
CONCLUSION
Using a longer needle will lead to a higher rate of successful needle thoracostomy in our population. Further studies will be needed to validate these findings in a more diverse patient population using a multicenter approach or derivation of a clinical decision rule. Interim changes in technique are needed. Techniques based on aspiration of pleural-based air or ultrasound guidance for reduction of tension pneumothorax to assure successful decompression and reduce potential lung injury will be essential while using longer needles. The current static recommendation of 51 mm needle by the American College of Surgeons ATLS guidelines must increase or be based on the individual patient.1 Advocacy for longer needle lengths for needle thoracostomy is essential until significant reductions in obesity rates are obtained.
Footnotes
Address for Correspondence: Thomas Edward Carter, DO, Southern Ohio Medical Center, Email: carterte@somc.org. 11 / 2013; 14:650 – 652
Submission history: Revision received January 9, 2013; Submitted July 26, 2013; Accepted July 31, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. . Advanced Trauma Life Support Course Manual. 2008;
2. Inaba K, Ives C, McClure K Radiologic Evaluation of Alternative Sites for Needle Decompression of Tension Pneumothorax. Arch Surg. 2012; 147:813-818
3. Zengerink I, Brink P, Laupland K Needle Thoracostomy in the Treatment of a Tension Pneumothorax in Trauma Patients: What Size Needle?. J Trauma. 2008; 64:111-114
4. Yamagiwa T, Morita S, Yamamoto R Determination of the Appropriate Catheter Length for Needle Thoracostomy by Using Computed Tomography Scans of Trauma Patients in Japan. Injury. 2012; 43:42-45
5. Ogden C, Carroll M, Kit B Prevalence of obesity in the United States, 2009–2010. . ;
6. Britten S, Palmer SH Needle thoracocentesis in tension pneumothorax: insufficient cannula length and potential failure. Injury. 1996; 27:321-322
7. Givens M, Ayotte K Needle thoracostomy: implications of computed tomography chest wall thickness. Acad Emerg Med. 2004; 11:211-213
8. Jones R, Hollingsworth J Tension pneumothoraces not responding to needle thoracocentesis. Emerg Med. 2002; 19:176-177
9. Britten S, Palmer SH Chest wall thickness may limit adequate drainage of tension pneumothorax by needle thoracocentesis. J Accid Emerg Med. 1996; 13:426-427
10. Mines D, Abbuhl S Needle thoracostomy fails to detect a fatal pneumothorax. Ann Emerg Med. 1993; 22:863-836


