| Author | Affiliation |
|---|---|
| John W. Hafner, MD, MPH | University of Illinois College of Medicine at Peoria, Division of Emergency Medicine, Peoria, Illinois |
| Adam Bryant, BS | University of Illinois College of Medicine at Peoria, Division of Emergency Medicine, Peoria, Illinois |
| Felix Huang, BS | University of Illinois College of Medicine at Peoria, Division of Emergency Medicine, Peoria, Illinois |
| Keir Swisher, DO | University of Illinois College of Medicine at Peoria, Division of Emergency Medicine, Peoria, Illinois |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction:
Our objective was to compare the effectiveness, speed, and complication rate of the traditional manually placed intraosseous (IO) catheter to a mechanical drill-assisted IO catheter by emergency medicine (EM) resident physicians in a training environment.
Methods:
Twenty-one EM residents participated in a randomized prospective crossover experiment placing 2 intraosseous needles (Cook® Intraosseous Needle, Cook Medical, Bloomington, IN; and EZ-IO® Infusion System, Vidacare, San Antonio, TX). IO needles were placed in anesthetized mixed breed swine (mass range: 25 kg to 27.2 kg). The order of IO placement and puncture location (proximal tibia or distal femur) were randomly assigned. IO placement time was recorded from skin puncture until the operator felt they had achieved successful placement. We used 3 verification criteria: aspiration of marrow blood, easy infusion of 10 mL saline mixed with methylene blue, and lack of stained soft tissue extravasation. Successful placement was defined as meeting 2 out of the 3 predetermined criteria. We surveyed participants regarding previous IO experience, device preferences, and comfort levels using multiple choice, Likert scale, and visual analog scale (VAS) questions. IO completion times, VAS, and mean Likert scales were compared using Student’s t-test and success rates were compared using Fisher’s exact test with p<0.05 considered significant.
Results:
Drill-assisted IO needle placement was faster than manually placed IO needle placement (3.66 versus 33.57 seconds; p=0.01). Success rates were 100% with the drill-assisted IO needle and 76.2% with the manual IO needle (p=0.04). The most common complication of the manual IO insertion was a bent needle (33.3% of attempts). Participants surveyed preferred the drill-assisted IO insertion more than the manual IO insertion (p<0.0001) and felt the drill-assisted IO was easier to place (p<0.0001).
Conclusion:
In an experimental swine model, drill-assisted IO needle placement was faster and had less failures than manual IO needle placement by inexperienced resident physicians. EM resident physician participants preferred the drill-assisted IO needle.
INTRODUCTION
Peripheral intravenous (IV) catheter placement is the most commonly used procedure to gain vascular access in the emergency department (ED), with over 25 million placements each year.1 However, when peripheral access is difficult or unsuccessful, intraosseous (IO) infusion is an alternative for life-saving vascular access.2–5 An IO needle can be placed within the medulla of bones, providing a non-collapsible venous sinus able to accommodate rapid fluid administration. Most medications or fluid support given through the IV route can also be given intraosseously.4 Traditionally, IO infusion was mostly used in pediatric cases, but adult IO infusion has become increasingly common.3–9,11
Current instruments used to obtain IO access include the standard Cook® IO needle (Cook Medical Co., Bloomington, IN), the drill-assisted EZ-IO® device (Vidacare Co., San Antonio, TX), the Jamshidi® needle (CareFusion Co., San Diego, CA), and the FAST1® IO infusion system (PYNG Medical Co., Richmond, BC). The Cook®, Jamshidi®, and FAST1® needles have been compared previously.6,12,13 The EZIO® catheter has been shown to be comparatively more effective than the FAST1® system in a prehospital system setting.14,15 The EZ-IO® catheter also demonstrated a high success rate (94–97%) in prospective observational studies with trained EMS personnel.16,17 To our knowledge this is the first study to compare the effectiveness, speed, and complication rate of the traditional manual intraosseous catheter (Cook®) to the mechanical drill-assisted intraosseous catheter (EZ-IO®) by emergency medicine resident physician trainees with limited IO placement experience, in a live swine model.
METHODS
Protocol approval was obtained from the local Institutional Review Board and Institutional Animal Care and Use Committee prior to experimentation. Twenty-one emergency medicine (EM) resident physicians participated in the study during an EM technical and procedural skills laboratory session. The procedural skills laboratory provides them opportunities to practice lifesaving procedures on a live swine model. The EM residency program consists of 10 residents per class (PGY1–PGY3). The program is based in a Midwestern University and associated academic ED, with an annual patient volume of 74,000. No extramural or industry funding was received for this study or the procedural skills laboratory.
Laboratory sessions began with a short lecture on the use of the drill-assisted and manual IO catheters. The lecture followed the manufacturer’s standard instructions on insertion of the Cook® and EZ IO® needles, as well as the clinical indications, contraindications, and possible adverse effects associated with the devices. For the Cook® IO, participants were instructed to use a smooth, controlled, to twisting motion with moderate pressure until there was a loss of resistance and the needle stood on its own, while for the EZ IO®, participants were instructed to squeeze the driver trigger and apply gentle, steady pressure until a “give” or “pop” was felt, indicating entry into medullary space. Faculty demonstrated the insertion of each device prior to the experiment initiation.
A randomization scheme assigned each resident to the needle insertion order, as well as the location of each needle (proximal tibia/distal femur). Mixed breed swine in good health were anesthetized using a combination of intramuscular injections ketamine (10 mg/kg) along with an inhalation aesthetic (isoflurane 4%). Each resident physician placed both a manual (Cook® 16 gauge × 30 mm intraosseus needle with a standard trochar tip design) and a drill-assisted needle (EZ IO® 15 gauge × 25 mm training intraosseus needle with 4 asymmetrical bevels on the stylet and 2 cutting tips on the catheter, and the 9050 Power Driver®) in a clean, but non-sterile technique. The time required for insertion was recorded beginning with puncture of the skin until the verbal end-mark given by the resident upon insertion. We evaluated successful placement using 3 criteria: aspiration of marrow blood, successful infusion of 10 mL methylene blue saline solution, and absence of extravasation of the stained saline solution. Successful IO insertion was defined as meeting two out of three criteria. Complications were defined as any event that would prevent successful placement in subsequent attempts with the same needle.
Participating residents were asked to complete a short survey after completion of the experiment. The administered questionnaire gauged prior experience using a modified Likert scale (1=strongly disagree, 5=strongly agree) and 10 cm Visual Analog Scale (VAS); 0 cm=most easy, 10 cm=most difficult). Participants were also asked to provide comments concerning the catheters and the study. IO completion times, VAS, and mean Likert scales were compared using Student’s t-test, and success rates were compared using Fisher’s exact test with p<0.05 considered significant.
RESULTS
Of the 21 resident participants, 14 were male (66.7%) and 7 were female (33.3%). Nine were first-year residents (42.9%), 7 were second-year residents (33.3%), and 5 were third-year residents (23.8%). Six residents (28.6%) had prior experience using the drill-assisted IO needle, and 12 residents (57.1%) had prior experience with the manual needle.
The average time to insertion for the drill-assisted IO needle was 3.66 seconds, compared to 33.57 seconds for the manual IO needle. The placement of the drill-assisted IO needles were successfully accomplished in 100% (21/21) compared to only 76.2% (16/21) of the manual IO needles (Table). There were no significant statistical relationships between anatomic sites (proximal or distal tibia) or among residents’ gender, experience, or post-graduate year level for number of attempts or placement time.
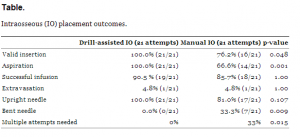
Intraosseous (IO) placement outcomes.
Establishing intraosseous access using the manually placed IO needle was associated with technical complications, such as bending or breaking an infusion needle such that subsequent intraosseous infusion was impossible. Thirty-three percent of the manually placed IO needles in our study were bent compared to none of the drill-assisted IO needles (Table). No other technical complications were observed.
Based on survey results using a modified Likert scale, resident physicians would prefer to use the drill-assisted IO needle over the standard manual IO needle (4.52 versus 1.57, respectively; p<0.0001) and feel more confident using the drill-assisted IO than the manual IO needle in a clinical situation (4.48 versus 3.62, respectively; p<0.0001). Using a VAS (1 easiest and 10 most difficult), EM resident physicians also felt the drill-assisted IO needle was easier to place than the manual IO needle (0.98 cm versus 4.59 cm, respectively; p<0.0001).
DISCUSSION
This study compared two methods of intraosseous insertion, the drill-assisted IO needle and the manual IO needle. Our study provided inexperienced resident physicians the opportunity to train with both needles on a live swine model. In acute emergent patient care scenarios, obtaining prompt intravenous or intraosseous access is often required. Clinicians in these situations require devices that are rapidly and can be readily placed. The results of our prospective randomized experimental trial indicate that the drill-assisted IO needle outperformed the manual IO needle with a higher success rate, faster insertion time, and fewer complications. The drill-assisted IO needle was the preferred device for emergency medicine resident physicians based upon survey data.
The reliability of intraosseous placement is imperative in emergency scenarios where medication, fluid, or blood administration is required and intravenous catheter placement is difficult to obtain or has been unsuccessful. Successful placement in our study was defined by meeting 2 of 3 criteria: aspiration of marrow blood, successful infusion of 10 mL methylene blue saline solution, and absence of extravasation of the stained saline solution. The rate of successful insertion of the drill-assisted IO needle compared to the manual IO needle demonstrates that the drill-assisted IO is the more reliable device in novice users. In comparison to a similar study published by Brenner et al12, the placement of the drill-assisted IO needle in adult human cadavers had a success rate of 97.8% (44/45), while the manual IO needle had a success rate of 79.5% (31/39). These other studies help support our findings that the drill-assisted IO needle is a more reliable device than the manual IO needle.11,14,17,18
Much of the reason for the decreased success of the manual IO needle can be attributed to the higher rate of complications. Both needles are 15G and are similar in size. It is possible that participants in our study may have placed increased force when trying to place the manual IO needle, causing them to bend. This could be due to their lack of experience with the device or the overall nature of the manual insertion.
The drill-assisted needle can also be placed in less time, allowing faster fluid and medication administration to the patient. In a recent study of pediatric ED patients, the time for placement of a drill-assisted IO in 73/95 (77%) patients was less than 10 seconds.18 This is consistent with our findings for drill-assisted IO insertion times. Other studies have shown comparable time lengths of 30 seconds for placement of both needles.3,12 Regardless of the device used, intraosseous puncture can be performed quickly with the novice user and should not be delayed when IV access cannot be obtained. In clinical practice, parameters such as the cost of device, local practice patterns, and provider training and comfort levels may also have an impact on clinicians’ decisions concerning the IO type utilized.
Resident responses in our survey show that the drill-assisted IO device is preferred over manual insertion in novice users. Residents also feel more confident with the drill-assisted IO needle and find it less difficult to use than the manual IO needle. These responses help solidify the drill-assisted IO needle as the better choice in inexperienced users.
LIMITATIONS
Our results must be interpreted in light of certain limitations. Participants were given the same in-service demonstration on the proper use of the devices. However, a certain degree of observational learning may have occurred with bystanders. Results may also be different in prehospital and clinical settings. The use of the swine model may serve as an explanation for the complications seen with the manual IO insertions, as swine are generally considered to have a thicker bone cortex than humans and in particular children. With more experienced users, different intraosseous devices may provide higher reliability and faster infusion. Further studies are needed to compare the rate of complications in novice users to that of experienced users in the prehospital or clinical setting.
CONCLUSION
The faster and more reliable placement of the drill-assisted IO needle in our anesthetized swine model makes it superior to the traditional manually placed IO needle in newly trained resident physician users. Future studies are needed to follow up and further evaluate our findings, particularly among children and in the prehospital setting.
Acknowledgments
We would like to thank James T. Brown, MD, Matthew N. Jackson, MD, Lauren E. Thompson, and Kyle Brown for their contributions to this study.
Footnotes
Address for Correspondence: John William Hafner, MD, MPH. University of Illinois College of Medicine at Peoria, 530 NE Glen Oak Ave, Peoria, IL 61637. Email: jhafner@uic.edu. 11 / 2013; 14:629 – 632
Submission history: Revision received August 8, 2012; Submitted March 26, 2013; Accepted April 15, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Soifer NE, Borzak S, Edlin BR Prevention of peripheral venous catheter complications with an intravenous therapy team: a randomized controlled trial. Arch Intern Med. 1998; 158:473-477
2. Calkins MD, Fitzgerald G, Bentley TB Intraosseous infusion devices: a comparison for potential use in special operations. J Trauma. 2000; 48:1068-1074
3. Jun H, Haruyama AZ, Chang KS Comparison of a new screw-tipped intraosseous needle versus a standard bone marrow aspiration needle for infusion. Am J Emerg Med. 2000; 18:135-139
4. Orlowski JP, Porembka DT, Gallagher JM Comparison study of intraosseous, central intravenous, and peripheral intravenous infusions of emergency drugs. Am J Dis Child. 1990; 144:112-117
5. Rosetti VA, Thompson BM, Miller J Intraosseous infusion: an alternative route of pediatric intravascular access. Ann Emerg Med. 1985; 14:885-888
6. Abe KK, Blum GT, Yamamoto LG Intraosseous is faster and easier than umbilical venous catheterization in newborn emergency vascular access models. Am J Emerg Med. 2000; 18:126-129
7. Dubick MA, Holcomb JB A review of intraosseous vascular access: current status and military application. Mil Med. 2000; 165:552-559
8. Findlay J, Johnson DL, Macnab AJ Paramedic evaluation of adult Intraosseous Infusion System. Prehosp Disaster Med. 2006; 21:329-334
9. Glaeser PW, Hellmich TR, Szewczuga D Five-year experience in prehospital intraosseous infusions in children and adults. Ann Emerg Med. 1993; 22:1119-1124
10. Glaeser PW, Losek JD, Nelson DB Pediatric intraosseous infusions: impact on vascular access time. Am J Emerg Med. 1988; 6:330-332
11. Miner WF, Corneli HM, Bolte RG Prehospital use of intraosseous infusion by paramedics. Pediatr Emerg Care. 1989; 5:5-7
12. Brenner T, Bernhard M, Helm M Comparison of two intraosseous infusion systems for adult emergency medical use. Resuscitation. 2008; 78:314-319
13. Hartholt KA, van Lieshout EM, Thies WC Intraosseous devices: a randomized controlled trial comparing three intraosseous devices. Prehosp Emerg Care. 2010; 14:6-13
14. Ong ME, Ngo AS, Wijaya R An observational, prospective study to determine the ease of vascular access in adults using a novel intraosseous access device. Ann Acad Med Singapore. 2009; 38:121-124
15. Frascone RJ, Jensen JP, Kaye K Consecutive field trials using two different intraosseous devices. Prehosp Emerg Care. 2007; 11:164-71
16. Davidoff J, Fowler R, Gordon D Clinical evaluation of a novel intraosseous device for adults: prospective, 250-patient, multi-center trial. JEMS. 2005; 30:20-23
17. Gillum L, Kovar J Powered intraosseous access in the prehospital setting: MCHD EMS puts the EZ-IO to the test. JEMS. 2005; 30:24-25
18. Horton MA, Beamer C Powered intraosseous insertion provides safe and effective vascular access for pediatric emergency patients. Pediatr Emerg Care. 2008; 24:347-350


