| Author | Affiliation |
|---|---|
| Matthew L. Harrison, DO | Huguley Memorial Medical Center, Department of Emergency Medicine, Burleson, Texas |
| Paul E. Lizotte, DO | University of Michigan, Department of Radiology, Ann Arbor, Michigan |
| Talmage M. Holmes, PhD | University of Arkansas for Medical Sciences, Department of Emergency Medicine, Little Rock, Arkansas |
| Phillip J. Kenney, MD | University of Arkansas for Medical Sciences, Department of Radiology, Little Rock, Arkansas |
| Charles B. Buckner, MD | University of Arkansas for Medical Sciences, Department of Radiology, Little Rock, Arkansas |
| Hemendra R. Shah, MBBS | University of Arkansas for Medical Sciences, Department of Radiology, Little Rock, Arkansas |
Introduction
Methods
Results
Conclusion
ABSTRACT
Introduction:
High body mass index (BMI) values generally correlate with a large proportion of intra-peritoneal adipose tissue. Because intra-peritoneal infectious and inflammatory conditions manifest with abnormalities of the adipose tissue adjacent to the inflamed organ, it is presumed that with a larger percentage of adipose surrounding a given organ, visualization of the inflammatory changes would be more readily apparent. Do higher BMI values sufficiently enhance the ability of a radiologist to read a computed tomography (CT) of the abdomen and pelvis, so that the need for oral contrast to be given is precluded?
Methods:
Forty six patients were included in the study: 27 females, and 19 males. They underwent abdominal/pelvic CTs without oral or intravenous contrast in the emergency department. Two board certified radiologists reviewed their CTs, and assessed them for radiographic evidence of intra-abdominal pathology. The patients were then placed into one of four groups based on their body mass index. Kappa analysis was performed on the CT reads for each group to determine whether there was significant inter-rater agreement regarding contrast use for the patient in question.
Results:
There was increasingly significant agreement between radiologists, regarding contrast use, as the study subject’s BMI increased. In addition, there was an advancing tendency of the radiologists to state that there was no need for oral or intravenous contrast in patients with higher BMIs, as the larger quantity of intra-peritoneal adipose allowed greater visualization and inspection of intra-abdominal organs.
Conclusion:
Based on the results of this study, it appears that there is a decreasing need for oral contrast in emergency department patients undergoing abdominal/pelvic CT, as a patient’s BMI increases. Specifically, there was statistically significant agreement, between radiologists, regarding contrast use in patients who had a BMI greater than 25.
INTRODUCTION
Background
An estimated 62 million computed tomographies (CT) are performed annually in the United States (U.S.).1 A substantial number of these are performed in emergency departments (ED). Many scans targeting the abdomen and pelvis require oral and intravenous contrast, which is currently believed to enhance the accuracy of the radiologist’s read of the scan. However, in a study in the American Journal of Surgery in 2005, no difference in sensitivity was found when radiologically diagnosing acute appendicitis whether or not the patient received oral contrast.2
Intra-abdominal infectious and inflammatory conditions often manifest with abnormalities of the adjacent fat of the peritoneal cavity and omentum, which are detectable without oral contrast. Because intra-peritoneal infectious and inflammatory conditions manifest with abnormalities of the adipose tissue adjacent to the inflamed organ, it is presumed that with a larger percentage of adipose surrounding a given organ, visualization of the inflammatory changes would be more readily apparent. In addition, abdominal abscesses can be detected without oral contrast. Bowel wall pathology may be better delineated with bowel distension secondary to contrast, but given the time constraints in the ED, oral contrast doesn’t usually reach the colon in time for the scan. Also, the detection of pneumatosis intestinalis is not improved by oral contrast. Lee and colleagues did a prospective study of 100 ED patients with abdominal pain. These patients were initially scanned without oral contrast and then again 90 minutes after oral contrast was given, with identical scanning parameters. Experienced radiologists were given no information about medical history before they interpreted the noncontrast CTs; the interpretation of the noncontrast scans matched scans in which the patients were given oral contrast.3
Because the yearly patient census at most U.S. EDs is increasing, rapidly examining, treating, and dispositioning patients is crucial for effective ED operation, maintaining patient safety, and sustaining hospital revenue.4 Eliminating the need to give oral contrast for abdominal/pelvic CTs performed on patients would greatly reduce the time some patients spend in the ED, allowing more to be seen, and improving ED throughput.
Do higher body mass index values sufficiently enhance the ability of a radiologist to read a CT of the abdomen and pelvis, so that the need for oral contrast to be given is precluded?
METHODS
Study Design, Setting, and Selection of Participants
This was a comparative study. An institutional review board exemption was granted for this study as no direct intervention was performed on the patients involved. Heights and weights were recorded on ED patients who underwent an abdominal/pelvic CT without oral contrast during the dates 12/4/10–1/4/11, and 4/22/11–5/20/11. This data was either obtained by weighing and measuring patients in triage by ED nurses (58 patients), or in the patient’s room, by the principle investigator (12 patients). It was collected at various times of the day and night, including weekdays, and weekends. We obtained data using a single scale/tape measure that recorded weight in kilograms and height in centimeters, and could be rolled from triage to the patient’s room. We excluded patients from the study if they presented to the ED secondary to any type of trauma. Individuals younger than 18 were excluded, as were any individuals who received oral contrast. In addition, we used only the data from a patient’s initial CT if the patient presented to the ED, and was scanned multiple times within the patient data collection period.
Methods of Measurement
We calculated body mass indices (BMI) on these patients using the collected data, and the formula: weight (in kilograms) divided by height (in meters) squared. The remaining patients were divided into 4 groups using the National Institute of Health’s BMI categories: <24.9, 25–29.9, 30–39.9, and >40. Two board-certified radiology attendings, including the department chair, and an expert in body CT reviewed the cases. The radiologists were blinded as to the purpose of the study; their objective was to read the scans as they normally would.
The radiologists filled out a form as they reviewed the CT for each patient. Both radiologists were assigned a number, which they would place atop each form to identify it as theirs. They also identified each form with the patient’s medical record number. The radiologists were to then specifically examine 4 organs on every CT: the gallbladder, appendix, pancreas, and colon. For each organ, they were to answer the question, “how well can you visualize the following anatomic structure for pathology?” by making a mark on a modified Likert scale located below the name of each organ. The scale was 12 cm long with the phrases, “Not at all” on the extreme left, and “Excellent” on the extreme right, without any marks or numbers in between. The radiologist was to place a mark on the line corresponding to how well each organ was visualized. If the radiologist could visualize a specific organ and completely identify all pathology related to that organ, he/she was to place a mark on “Excellent” for that organ. If the organ could not be visualized at all, a mark was to be placed on “Not at all.” If the organ could be identified with average difficulty, a mark was to be placed midway between the two ends of the scale, etc. The radiologists, while assessing each organ for pathology, were not instructed to delineate the pathology they identified on the grade sheet, but only to assess the difficulty with which they identified it and their ability to identify it. At the lower portion of the form was an additional question for the radiologists to answer, based on how accurately each preceding organ was identified. That question asked, “was there a need for contrast in this patient?” The radiologist was to circle, “yes,” or “no.”
Data Collection and Processing
Seventy patients identified during the data collection period met criteria for inclusion in the study. Five were excluded initially: 1 for receiving intravenous contrast, 3 because they had undergone recent surgery secondary to metastatic carcinoma, and 1 because his CT was of poor technical quality and unreadable. One additional patient was overlooked during the CT reading period and was excluded because there was no read for his scan. It was determined that an additional 18 patients had missing data on their grade forms, after the radiologists finished reading their CTs, and were excluded from the study as well due to missing data. Any attempt to have the radiologists re-read these scans was futile, as they maintain a robust clinical and academic schedule and did not afford the time necessary to re-read 18 CTs. Forty-six patients were included in the study: 27 females, and 19 males. The average age was 37 years, and average BMI was 29. The average age for patients in the “normal BMI” category was 36, and percent female was 46. The average age for patients in the “overweight” category was 37, and percent female was 56. The average age for patients in the “obese” category was 38, and percent female was 72. The average age for patients in the “morbidly obese” category was 35, and percent female was 66.
Primary Data Analysis
We performed Kappa analysis on the data to ascertain whether there was a statistical measure of inter-rater agreement between radiologists in determining whether or not oral contrast was needed in the study subjects.
RESULTS
In the “normal BMI” group (<24.9), the radiologists agreed that no contrast was needed in 9 of 16 cases. In the “overweight” group (25–29.9), they agreed no contrast was needed in 16 of 19 cases. In the “obese” group (30–39.9), they agreed no contrast was needed in 11 of 13 cases. And in the “morbidly obese” group (>40), they agreed no contrast was needed in all 6 cases.
In the “normal BMI” group, a Kappa value of 0.259 was calculated, with a p-value of 0.247. In the “overweight” group, a Kappa value of 0.457 was calculated, with a p-value of 0.018. In the “obese” group, a Kappa value of 0.629 was calculated with a p-value of 0.015. And in the “morbidly obese” group, a Kappa value of 1.0 was calculated with a p-value of 0.00.
CONCLUSION
There was increasingly significant agreement between radiologists regarding contrast use, as the study subject’s BMI increased. In addition, there was an advancing tendency of the radiologists to state that there was no need for contrast to be administered in patients with higher BMIs. Eliminating the need to give oral contrast to patients undergoing abdominal and pelvic CTs in the ED (even if only eliminating the need to give contrast to patients with higher BMIs), would greatly reduce the length of stay for some ED patients, decrease wait times, increase ED throughput, increase hospital revenue, and theoretically decrease the percentage of complications from patients receiving contrast material. In addition, this and future studies regarding this topic could be helpful medico-legally as they provide a degree of evidence (albeit small) to defend a practice that is becoming increasingly popular among ED providers: that of scanning patients who present to the ED with abdominal pain without oral contrast. Perhaps there is a subset of these patients – those with a high BMI – who deserve to be scanned without oral contrast. A larger study is needed to verify the results of this pilot study and to determine at what BMI radiologists feel comfortable scanning patients without contrast.
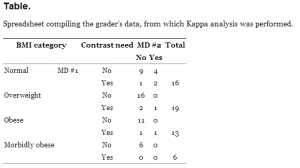
Spreadsheet compiling the grader’s data, from which Kappa analysis was performed.
Footnotes
Address for Correspondence: Matthew L. Harrison, DO. 3228 Rogers Ave., Fort Worth, TX 76109. Email: matthewlharrison@gmail.com. 11 / 2013; 14:595 – 597
Submission history: Revision received July 17, 2012; Submitted March 8, 2013; Accepted May 20, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Brenner DJ, Hall EJ Computed Tomography. An Increasing Source of Radiation Exposure. N Engl J Med. 2007; 357:2277-2284
2. Anderson BA, Salem L, Flum DR A systematic review of whether oral contrast is necessary for the computed tomography diagnosis of appendicitis in adults. Am J Surg. 2005; 190:474-478
3. Lee SY, Coughlin B, Wolfe JM Prospective comparison of helical CT of the abdomen and pelvis without and with oral contrast in assessing acute abdominal pain in adult emergency department patients. Emerg Radiol. 2006; 12:150-157
4. Hong R, Baumann BM, Boudreaux ED The Emergency Department for Routine Healthcare: Race/Ethnicity, Socioeconomic Status, and Perceptual Factors. J Emerg Med. 2007; 32:149-158


