| Author | Affiliation |
|---|---|
| Bharath Chakravarthy, MD, MPH | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
| Shyam Shah, MD | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
| Shahram Lotfipour, MD, MPH | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
ABSTRACT
The Center for Disease Control and Prevention (CDC) has published significant data and trends related to opioid prescription pain relievers (OPR). In 2008, 20,044 deaths were attributed to prescription drug overdose of which 14,800 (73.8%) were due to OPR, an amount greater than the number of overdose deaths from heroin and cocaine combined. The majority of these deaths were unintentional. Between 1999–2008, overdose deaths from OPR increased almost four-fold. Correspondingly, sales of OPR were four times greater in 2010 than in 1999. Most significant to emergency physicians is the estimate that 39% of all opioids prescribed, administered or continued come from the emergency department (ED). We present findings from the CDC’s Morbidity and Mortality Weekly Report (MMWR) with commentary on current recommendations and policies for curtailing the OPR epidemic.1
CDC MMWR FINDINGS
In the November 4, 2011, issue of the Morbidity and Mortality Weekly Report (MMWR), the CDC published data and trends related to opioid prescription pain relievers (OPR). The MMWR article mainly examined figures related to overdose deaths from prescription OPR, while also discussing usage among different demographics and U.S. states. The report clearly demonstrated that deaths from opioid painkillers have continued to increase along with several other concerning trends.
To gather data related to overdose deaths, the CDC used the “multiple cause-of-death mortality files,” a subset of data from the National Vital Statistics System database (maintained by the National Center for Health Statistics). The “multiple cause-of-death mortality files” provides mortality data by cause of death for all deaths occurring in the United States (U.S.) from 1959 – 2009. Data are obtained from death certificates filed in the National Vital Statistics System offices in each state and the District of Columbia. CDC researchers accessed these data between 1999 and 2008 and were able to sort causes of death due to drug overdose, prescription drug overdose and overdose related to OPRs by using ICD-10 (International Classification of Disease – 10th edition)codes.
In 2008, 36,450 deaths were attributed to drug overdose, of which 27,153 were due to identifiable drugs. Of the 27,153 deaths attributed to identifiable drugs, 20,044 (75%) involved one or more prescription drugs. OPR were involved in 14,800 (73.8%) of the 20,044 deaths related to prescription drug overdose. The majority of these deaths were listed as unintentional, versus suspected suicide or undetermined. Between 1999–2008, overdose deaths from OPR increased exponentially; overdose deaths attributed to OPR were almost four times greater in 2008 than in 1999. Correspondingly, sales of OPR were four times greater in 2010 than in 1999.1
Data from the MMWR showed that deaths due to OPRs were not uniform across demographic groups. OPR overdose deaths in 2008 seemed to be significantly greater among men (5.9/100,000 population) than women (3.7/100,000). OPR overdose death rates in 2008 among Non-Hispanic whites (6.3/100,000 population) and American Indians/Alaska Natives (6.2/100,000) were approximately 3 times higher than Hispanics (2.1/100,000) and blacks (1.9/100,000) and approximately 12 times greater than Asians/Native Hawaiians/Pacific Islanders (0.5/100,000). This is in contrast to overdose death rates for illicit substances, where the rates among blacks (4.0/100,000) were significantly greater than Non-Hispanic whites (2.9/100,000), Hispanics (2.5/100,000) American Indians/Alaska Natives (2.7/100,000) and Asians/Native Hawaiians/Pacific Islanders (0.6/100,000). Differences in OPR overdose mortality by race/ethnicity match the pattern for medical and nonmedical use of OPRs, with the lowest rates for medical and nonmedical use among Asians and blacks and the highest rates among American Indians/Alaska Natives and non-Hispanic whites. By age, the overdose death rate due to OPR was substantially higher for those ages 25–54 then other groups.1
Additional data from the MMWR showed that trends in OPR sales, OPR use for non-medical purposes and total drug overdose deaths varied widely across states. In 2010, the 5 states with the highest levels of OPR sales were: Florida (12.6 kg OPR sold/100,000 population), Nevada (11.8/100,000), Tennessee (11.8/100,000), Oregon (11.6/100,000) and Delaware (10.2/100,000). From 2008 to 2009, the 6 states with highest rate of persons age 12 and older using OPR non-medically were: Oklahoma (8.1 persons age 12 or older/100,000 population), Oregon (6.8/100,000), Washington (6.1/100,000), Rhode Island (6.1/100,000), Arizona (6.0/100,000) and Kentucky (6.0/100,000). In 2008, the 5 states with the highest rate of drug overdose deaths were New Mexico (27.0 deaths /100,000 population), West Virginia (25.8/100,000), Nevada (19.6/100,000), Utah (18.4/100,000) and Alaska (18.1/100,000).1
It is instructive to compare the rates of overall drug overdose deaths with rates of non-medical use and sales. One would expect those states with high non-medical use rates and high OPR sales to be more likely to have above average overdose death rates. Indeed, that appears to be the case. Among the 27 states with drug overdose death rates above the national rate, 21 (77.8%) had rates of nonmedical use of OPR above the national rate. Among the 24 states with drug overdose death rates at or below the national rate, only 6 (25.0%) had rates of nonmedical use of OPR above the national rate. Among these same 27 states with drug overdose death rates above the national rate, 21 (77.8%) had rates of OPR sales above the national rate. Among these same 24 states with drug overdose death rates at or below the national rate, only 5 (20.8%) had rates of OPR sales above the national rate.1
The CDC stated that there are limitations to the findings in the MMWR. Vital Statistics information underestimates the rates of prescription and illicit drugs because the type of drug is not specified on many death certificates. Additionally, respondents might underreport nonmedical use of OPR in surveys.
COMMENTARY
A clinical scenario frequently encountered by many emergency physicians (EP) follows: A 27-year-old woman is brought in by ambulance to the ED with a Glasgow Coma Scale score of 5. EMS found the patient unresponsive at her home with shallow respirations at 5 per minute. The patient has pinpoint pupils, suggesting opioid overdose. The patient is given multiple rounds of intravenous naloxone that succeed in reversing the overdose and resuscitating her. This clinical scenario is not unfamiliar to most EDs, but a fact that may not be known is that there is over a 50% likelihood that the opiates causing the overdose were legally manufactured prescription painkillers.1 The CDC estimates that 14,800 deaths in 2008 were due to OPRs, a figure which is greater than the number of deaths attributed to heroin and cocaine combined.1 Perhaps most significant to EPs is the estimate that 39% of all opioids prescribed, administered or continued come from the ED.2
Although our patient was successfully resuscitated, many patients are not as fortunate. It is believed that the number of overdoses due to OPRs have nearly quadrupled over a 10-year period from 1999 – 2008.1 This increase in overdose deaths seems directly correlated with the large increase in sales of prescription opioids, which also quadrupled between 1999 – 2010.1 The CDC estimates that in 2010 enough OPRs were sold to medicate every American with a typical 5 mg dose of hydrocodone every 4 hours for 1 month.1 It is clear that prescription opioid abuse, dependence and overdose are growing epidemics that will continue to claim lives unless interventions are made.
There are a number of potential reasons for the increase in incidence of opiate abuse and dependence in the U.S. A possible major driving factor of the epidemic is that OPRs are a legally available alternative to illicit substances, such as heroin, and also have the potential to create euphoria and addiction. It is likely that many patients with chronic pain misrepresent their need for OPRs and then either abuse their obtained medications or sell them to others.3 Ultimately, it is prescriptions written by physicians that enable such patients to have access to drugs with a high potential for abuse. Physicians face the difficult challenge of balancing the treatment of legitimate chronic pain patients with combating the OPR epidemic that is claiming so many lives.
To manage this issue, health policy analysts at the CDC have listed several recommendations. Of these recommendations, the one that has significant potential for assisting EPs in curtailing the epidemic is the use of Prescription Drug Monitoring Programs (PDMPs). PDMPs are state-run electronic databases that track the prescribing and dispensing of controlled prescription drugs to patients. The PDMPs enable physicians to assess whether patients have received unusually high or excessive amounts of controlled substances in the past and adjust their prescribing decisions accordingly. The CDC also believes PDMPs will enable physicians to control “Doctor Shopping,” the practice where pain-medication seeking patients visit many different physicians (oftentimes in multiple states) to obtain prescriptions.1 The CDC recommends that PDMPs link to electronic health-records systems, so that PDMP information is better integrated into healthcare providers’ day-to-day practices. These recommendations have already been adopted by many hospitals, and professional organizations such as the American College of Emergency Physicians (ACEP) have actively encouraged members to integrate PDMP usage into their general practice.4
One study has monitored how PDMPs influence EP prescribing practices; Baehren et. al in 2008 examined the effect of the Ohio state PDMP, the Ohio Automated Rx Reporting System, on ED prescribing practices. This study of 179 patients was conducted at one ED in Ohio and found that EPs changed their prescription decision after accessing the state PDMP in 41% of the cases. In 61% of the cases where the EP’s original decision was altered, fewer or no opioid medications were prescribed than originally planned. In 39% of the cases where EPs altered their original decision, more opioid medications were prescribed than previously planned.5 The results of this study indicate that PDMPs have the potential to assist physicians in making more judicious decisions when prescribing opioid pain medications. More clinical research and data is needed to measure the impact of these statewide PDMPs, as another study found that states with PDMPs already in place had no significant decrease in the number of overdose deaths from opioids.6 This suggests that physician education in an attempt to change practice patterns can be an effective way to maximize the clinical utility of PDMPs. If PDMPs are shown to be an effective means of appropriately managing prescribing of OPRs, national and statewide efforts to incentivize physicians to use PDMPs are viable future strategies for controlling OPR abuse.
The CDC also believes that physician education regarding use of OPR is another important strategy to control the prevalence of OPR abuse and overdose. On a national level, the CDC has suggested mandatory prescriber education, including requiring prescribers to be trained in appropriate prescribing of opioids before obtaining their controlled substance registration from the Drug Enforcement Administration (DEA).3 This recommendation has already been listed as a planned action item in the Presidential 2011 report on the prescription opioid epidemic. Another planned intervention listed in the report is collaborating with appropriate medical boards to institute required educational curricula in health professional schools and using continuing medial education programs to teach the safe and appropriate use of OPR. The report also included working with the American College of Emergency Physicians to develop evidence-based clinical guidelines that establish best practices for opioid prescribing in the ED.7
Other recommendations made by the CDC (which are outside the typical day-to-day practice of physicians) also show significant promise in combating the OPR abuse epidemic. These recommendations include instituting regulations against rogue pain clinics, or “pill mills,” and practitioners who unethically dispense prescription pain medications. There have already been efforts at both the federal and statewide level to take actions against these unscrupulous distributors of prescription medication. The Drug Enforcement Administration has worked alongside state and municipal law enforcement agencies to shut down rogue pain clinics and prosecute the physicians that work for them. In the state of Florida alone, 477 illegal pain clinics have been shut down by authorities over the last 2 years.8 A 2011 report by the American College of Surgeons details how a number of states have instituted regulations against pill mills and penalties against healthcare workers that deviate from state specific guidelines for prescribing controlled substances. Louisiana has instituted its own guidelines for pain clinics under a Pain Management Clinic Law; violation of the law can result in a fine up to $50,000 or a 5-year prison sentence. Texas rogue pain clinic laws make it illegal to own or operate a pain clinic without certification from the Texas Medical Board and owners and employees must go through a background check. The state of Florida has passed legislation that establishes standards for physicians who prescribe narcotic-grade pills. This same legislation increased penalties against physicians who overprescribed narcotics to a minimum of $10,000 and a 6-month license suspension. The law also bans physicians from on-site dispensing of the most abused pills, including oxycodone and hydrocodone.9 Some states have sought more severe charges against unethical physicians; a Southern California physician, who wrote 27,000 prescriptions for opiates and benzodiazepines over a 3-year period, is being prosecuted for second-degree murder in relation to overdose deaths. If convicted, this physician faces a 45-year prison sentence.10
In addition to increased regulation and use of PDMPs, the CDC also recommends states increase access to substance abuse treatment programs. Although the CDC has not given specific recommendations, several initiatives are being reported nationwide to improve access. The newly passed Affordable Care Act requires coverage for substance abuse services by health insurance plans.11 The 2011 Presidential report on the prescription opiate epidemic set a goal of expanding funding for substance abuse treatment by 10% over the next 36 months.7 Eleven states have taken measures to allow Vivitrol (Naltrexone) to be more easily available to physicians by allowing pharmacies to bill Medicaid directly for reimbursement (versus having physicians who administer the medicine pay for it out of pocket and then seek reimbursement from Medicaid).12 In 2006 Congress passed legislation that made Suboxone (buprenorphine) another drug used in detox from opiates, more accessible to patients needing substance abuse treatment. The new legislation increased the limit of patients per physician that may receive Suboxone from 30 to 100.13 Since 2010 the state of Maryland expanded access to substance abuse treatment services by increasing service reimbursement rates to Medicaid providers and expanding benefits of state substance abuse program to include outpatient substance abuse treatment.14 These are all examples of federal and statewide efforts to increase access to substance abuse treatment programs. However, due to the alarming rate of growth of the OPR epidemic, it is clear that more will need to be done across the nation to treat those already struggling with opiate addiction.
In summary, abuse of prescription opiates and corresponding overdose deaths are rapidly growing issues for our society. Many of the CDC’s recommendations to combat the epidemic have been adopted at both the federal and state level. Because a large number of prescriptions for these medications come from EDs, emergency physicians will be at the forefront of efforts to control inappropriate prescription of opiate painkillers. PDMPs are promising tools that can be used by physicians to better control their prescribing practices.
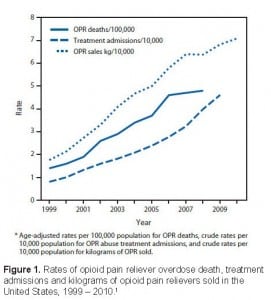
Rates of opioid pain reliever overdose death, treatment admissions and kilograms of opioid pain relievers sold in the United States, 1999 – 2010.
Footnotes
Supervising Section Editor: Mark I Langdorf, MD, MHPE
Submission history: Submitted July 11, 2012; Revision received July 18, 2012; Accepted July 20, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.7.12936
Address for Correspondence: Bharath Chakravarthy, MD, MPH University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California
Email: bchakrav@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Centers for Disease Control and Prevention (CDC) Vital Signs: Overdose of prescription opioid pain relievers – United States, 1999 – 2008. MMWR Morbidity Mortality Weekly Report. 2011;60(43):1487–92.
2. Emergency Department Opioid Abuse Work Group – Sponsored by the Washington State Department of Health Washington Emergency Department Opioid Prescribing Guidelines. Washington ACEP Web site. Available at:http://washingtonacep.org/Postings/edopioidabuseguidelinesfinal.pdf. Accessed July 3, 2012.
3. Baehren DF, Marco CA, Droz DE, Sinha S, Callan EM, Akpunonu P. A statewide prescription monitoring program affects emergency department prescribing behaviors.Annals of Emergency Medicine. 2010;56(1):19–23. [PubMed]
4. Center for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses – a U.S. epidemic. MMWR Morbidity Mortality Weekly Report. 2012;61(1):10–3.
5. Fenton A. Despite early flaws CURES proves invaluable in preventing prescription drug abuse. Lifeline. 2012;1:10–11.
6. Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Medicine. 2011;12:747–754. [PubMed]
7. The White House Epidemic: responding to America’s prescription drug abuse crisis.thewhitehouse.gov Web site. Available at:http://www.whitehouse.gov/sites/default/files/ondcp/policy-and-research/rx_abuse_plan.pdf. Accessed July 4, 2012.
8. CBS 12 News Local officials caution there could be fallout from closing pill mills. CBS 12 News Web site. Available at: http://www.cbs12.com/news/top-stories/stories/vid_1053.shtml. Accessed July 3, 2012.
9. Macias A. State legislatures attempt to shut down pill mills. Bulletin of the American College of Surgeons. 2011;96(11):38–9. [PubMed]
10. Lipsky J. “Dirty doctor to stand trial in connection with death of San Ramon student. San Ramon express Web site. Available at:http://www.sanramonexpress.com/news/show_story.php?id=5934. Accessed July 17, 2012.
11. The White House Substance abuse and the Affordable Care Act. thewhitehouse.govWeb site. Available at: http://www.whitehouse.gov/ondcp/healthcare. Accessed July 4, 2012.
12. Welsh-Huggins A. Ohio expands use of anti-narcotic treatment. SFGate Web site. Available at: http://www.sfgate.com/news/article/Ohio-expands-use-of-anti-narcotic-treatment-3681973.php. Accessed July 4, 2012.
13. Levin A. Congress lets M.D.s treat more buprenorphine patients. Psychiatry News.2007;42:4.
14. Bienek M. More marylanders getting substance abuse treatment: state expanding programs as need continues to grow. Cumberland Times-News Web site. Available at:http://times-news.com/latest_news/x1254881669/More-Marylanders-getting-substance-abuse-treatment. Accessed July 4, 2012.


