| Author | Affiliation |
|---|---|
| Casey A. Grover, MD | Stanford/Kaiser Emergency Medicine Residency, Department of Emergency Medicine, Stanford, California |
| Joshua W. Elder, MD, MPH | David Geffen School of Medicine, University of California Los Angeles, Los Angeles, California |
| Reb JH. Close, MD | Community Hospital of the Monterey Peninsula, Department of Emergency Medicine, Monterey, California |
| Sean M. Curry, MD | Kaiser Permanente Santa Clara Medical Center, Department of Emergency Medicine, Santa Clara, California |
ABSTRACT
Introduction:
Drug-seeking behavior (DSB) in the emergency department (ED) is a very common problem, yet there has been little quantitative study to date of such behavior. The goal of this study was to assess the frequency with which drug seeking patients in the ED use classic drug seeking behaviors to obtain prescription medication.
Methods:
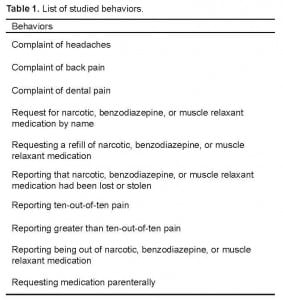
We performed a retrospective chart review on patients in an ED case management program for DSB. We reviewed all visits by patients in the program that occurred during a 1-year period, and recorded the frequency of the following behaviors: complaining of headache, complaining of back pain, complaining of dental pain, requesting medication by name, requesting a refill of medication, reporting medications as having been lost or stolen, reporting 10/10 pain, reporting greater than 10/10 pain, reporting being out of medication, and requesting medication parenterally. These behaviors were chosen because they are described as “classic” for DSB in the existing literature.
Results:
We studied 178 patients from the case management program, who made 2,486 visits in 1 year. The frequency of each behavior was: headache 21.7%, back pain 20.8%, dental pain 1.8%, medication by name 15.2%, requesting refill 7.0%, lost or stolen medication 0.6%, pain 10/10 29.1%, pain greater than 10/10 1.8%, out of medication 9.5%, and requesting parenteral medication 4.3%. Patients averaged 1.1 behaviors per visit.
Conclusion:
Drug-seeking patients appear to exhibit “classically” described drug-seeking behaviors with only low to moderate frequency. Reliance on historical features may be inadequate when trying to assess whether or not a patient is drug-seeking.
INTRODUCTION
Pain is cited as the most common reason for visits to the emergency department (ED).1–3In 1997, 94.9 million ED visits, accounting for 22% of all ED visits, resulted in the administration of pharmacotherapy for pain.4 Despite the frequent use of pharmacotherapy, many studies have suggested that emergency physicians (EP) undertreat patients’ pain in what is termed oligoanalgesia.5 While there are numerous reasons for which EP are hesitant to provide opiate analgesia, concern for patients seeking medication for non-therapeutic purposes is among the most common.3,6–9 Such patients are estimated to account for as many as 20% of all ED visits, and are often labeled as “drug-seeking.” Furthermore, they often present with conditions that are difficult to evaluate and easily feigned, such as headache, back pain, and dental pain.8–11
Despite their prevalence, there is no uniform method established to identify these drug-seeking patients. Some ED have developed habitual patient files and case management programs to track patients with frequent use of emergency care, while others have increased physician education as a means to improving identification of these patients.8,10,12–16 Additionally, several screening methods (Screener and Opioid Assessment for Patients with Pain – Revised, Opioid Risk Tool, Current Opioid Misuse Measure, Diagnosis, Intractability, Risk, and Efficacy inventory, and Addiction Behaviors Checklis) have been developed to assist in identifying problematic narcotic use in chronic pain patients. However, these screening methods were developed in pain clinics and may be lengthy, making them difficult to use in the ED.17–24 Uniform among all of these approaches is the reliance on the identification of drug-seeking behavior as a means of identifying problem patients. Such behaviors frequently cited as being present in ED patients include complaining of headache, back pain, dental pain, requesting medication by name, requesting a refill of narcotics, benzodiazepines, or muscle relaxants (high risk medications for abuse[HRM]), reporting HRM as having been lost or stolen, reporting being out of HRM, reporting greater than 10/10 pain, and requesting HRM parenterally. While there is a preponderance of publications on the subject of drug-seeking patients, there is very little literature that quantifies the prevalence of these behaviors.10,25–29 By identifying the frequency of these drug-seeking behaviors we can begin to understand whether our current approach in identifying these patients is both effective and substantiated.
Previously, we reported what we believe to be an innovative study that provided quantitative data as to the relative frequency of drug-seeking behaviors in patients suspected of non-therapeutic use.29 This case- control study proved instructive in identifying the most common classic drug-seeking behaviors, which included requesting parenteral medication and reporting greater than 10/10 pain. The study did not, however, assess the prevalence of these classic drug-seeking behaviors among drug-seeking patients. Our goal for this investigation was to assess the frequency with which drug seeking patients in the ED use classic drug-seeking behaviors to obtain prescription medication.
METHODS
This study consisted of a retrospective chart review performed at a 205-bed community hospital that receives approximately 55,000 ED visits each year. The hospital is located in a suburban area, in a city of approximately 30,000 people. The hospital also serves several neighboring cities, serving a total of approximately 100,000 people in the area. This study was given Institutional Review Board (IRB) exemption by the hospital committee on research
The hospital ED has a case management program that functions to assist in the care and management of difficult patients in the ED, particularly those patients frequently seeking emergency care for problems related to prescription medication addiction. Patients may be considered for enrollment in this program if they are identified as having 5 or more visits in a 1-month period or if any member of the ED staff is concerned about repetitive use of the ED for drug-seeking behavior. Furthermore, any patient identified by the California Bureau of Narcotic Enforcement as having committed prescription forgery or fraud is automatically enrolled in the program. As the criteria for enrollment in the program are not strictly defined, the reason for enrollment is not kept in the patients’ case management files. While not all patients in the case management program are enrolled for problems related to substance abuse, nearly 95% of the patients have a case management care plan that limits the prescription of controlled substances or referral to chemical dependency.15 The goal of the case management program is not to capture all drug-seeking patients in the ED; rather, it is to address the patients with excessive ED use secondary to drug-seeking behavior and other issues.
Inclusion criteria for patients in our study were the following: any patient enrolled in the case management program that was given a referral to chemical dependency and any patient enrolled in the case management program that had a care plan involving limitation of narcotics, benzodiazepines, or muscle relaxants.
Exclusion criteria for patients in our study were the following: all patients enrolled in the case management program whose care plans did not involve either a chemical dependency evaluation or limitation of narcotics, benzodiazepines, or muscle relaxants. We did not exclude patients with known painful chronic medical conditions.
For each of the patients that met our inclusion criteria, we reviewed all visits to the ED for a 1-year period prior to enrollment in the case management program. Patient medical records were accessed using the hospital’s medical record system, Horizon Patient Folder (McKesson, 2002), and all physician and nurse documentation for each visit was carefully reviewed. For each patient, we recorded the number of times that patients exhibited any of the 10 behaviors listed in Table 1. As this study was a retrospective chart review, physicians and nurses treating these patients were not expected to look for or document the presence or absence of these behaviors; rather, we recorded the number of times these behaviors were documented in the medical record. If 2 (or more) behaviors occurred at a single visit, then both (or more, if present) behaviors were recorded as individual events. Furthermore, we only looked at each drug-seeking behavior in isolation. We did not record the number of visits at which a patient demonstrated multiple behaviors.
These 10 behaviors were chosen for assessment as they represent drug-seeking behaviors frequently reported in the literature, and are often described as being “classic” for such behavior.10–12,25,30–32 While certain behaviors commonly associated with drug-seeking behavior, such as headache and reporting a non-narcotic allergy, are easy to assess in a chart review, behaviors such as exaggeration of symptoms are not. We thus chose to look for complaining of 10/10 pain and complaining of greater than 10/10 pain as measurable equivalents to assess for exaggeration of symptoms.
Due to limitations on access to the hospital’s medical record system, each chart was reviewed by a single physician reviewer. To standardize the chart review and data collection process, we collected and entered data into a pre-formatted Excel spreadsheet (Microsoft, 2007) consisting of 1 column for patient medical record number followed by 10 columns (one for each studied behavior).
Once data collection was complete, we analyzed the data using Excel (Microsoft, 2007). For each of the 10 behaviors studied, we tallied the total number of times each behavior was exhibited. We then calculated the percentage of total visits at which patients in our study demonstrated each behavior, as well as a 95% confidence interval for each calculated percentage.
RESULTS
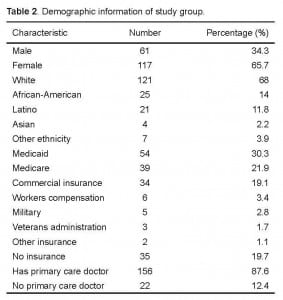
Review of patients in the case management program identified 178 patients meeting inclusion criteria. The average age of studied patients was 42.7 years, with complete demographic information listed in Table 2. These 178 patients contributed to 2,488 visits to the ED in the 1-year prior to enrollment in the case management program, which represented an average of 13.9 visits per patient per year. We recorded that our studied behaviors occurred 2,775 times in total, which corresponds with a calculated average of 1.1 behaviors per visit.
The frequency of each of the classic drug-seeking behaviors is outlined in Table 3. The most prevalent classic drug-seeking behavior was complaint of 10/10 pain, followed by complaint of headache, and then complaint of back pain. The least prevalent behavior was complaint of lost medication.
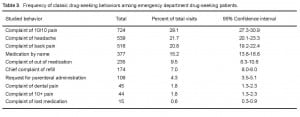
Frequency of classic drug-seeking behaviors among emergency department drug-seeking patients.
DISCUSSION
In this study, which represents one of the largest groups of drug-seeking ED patients studied to date, we found that drug-seeking patients appear to exhibit “classically” described drug-seeking behaviors relatively infrequently. In reviewing this data, it appears that relying on the presence of any single one of our studied behaviors would be of low sensitivity to identify drug-seeking patients in the ED. As such, EP may attempt to use the presence of multiple drug-seeking behaviors to identify patients presenting to the ED to obtain prescription medications. However, our patients demonstrated approximately 1.1 drug-seeking behaviors per ED visit, which suggests that multiple behaviors at a single visit is a relatively uncommon event. Additionally, the behaviors most frequently used (headache, back pain, and 10/10 pain) are extremely common complaints in the ED, and are likely not very specific for the diagnosis of drug-seeking behavior. These results are concerning, as they suggest that utility of using historical features to identify drug-seeking patients in the ED is limited. Reliance on any single historical feature to identify drug-seeking patients is likely inadequate as a result of the low frequency of each behavior. Furthermore, reliance on the presence of multiple historical features is inadequate as a result of the low frequency with which multiple behaviors are used at a single visit.
Our results are particularly important in the context of nonmedical use of prescription medication reaching near-epidemic proportions in the United States, especially that of narcotics and benzodiazepines. Approximately 7 million Americans over the age of 12 use prescription medications for non-therapeutic reasons each year, and non-medical use of prescription medications leads to upward of 700,000 ED visits yearly.33,34. Furthermore, death from narcotic overdose has more than tripled between 1999 to 2006, with nearly 14,000 opiate-related deaths in 2006. Research on opiate-related deaths has shown that patient non-adherence and underlying substance use disorders are 2 of the major factors contributing to prescription-misuse related mortality.35 Prescription misuse is particularly common in the ED, with up to 20% of all ED visits being made by drug-seeking patients.4 This unfortunate situation places an impetus on EP to be vigilant and skilled in detecting patients trying to obtain medications for non-therapeutic reasons. With the data from this study demonstrating the inadequacy of history alone in detecting drug-seeking patients, EP are in dire need of a better way to identify patients who are trying to obtain narcotics for non-therapeutic reasons. The vast majority of states in the U.S. now have state-run prescription monitoring programs, which allow physicians and pharmacists to access a patient’s prescription record for controlled substances. Previous research by Baehren et al has demonstrated that access to such prescription monitoring programs in the ED affects EP prescribing behaviors, but research on the use of such programs in the ED is extremely limited.36 As it pertains to the results of this endeavor, none of the physicians at our study site had access to such a database during the time of study.
Further research on the use of prescription monitoring programs in treating drug-seeking patients in the ED is imperative, as it may allow EP to better detect addiction in the ED. Potentially useful research on the topic includes how to interpret the information obtained in a prescription monitoring record when assessing a patient presenting to the ED, whether or not the routine use of prescription monitoring programs increases detection of drug-seeking patients in the ED, and an assessment of the accuracy of EP in diagnosing drug-seeking behavior by comparing EP clinical assessment of drug-seeking to the prescription record.
One major difficulty in studying patients suspected of drug-seeking behavior is that there is no way to definitively determine the motive of the patient s trying to obtain prescription medication. Pseudoaddiction is a condition resulting from inadequate pain management, in which patients may exhibit “classic” drug-seeking behaviors to obtain medication so as to relieve their pain. Once a patient’s pain is adequately treated, the patient’s drug-seeking behaviors cease. Unfortunately, the behaviors used by patients seeking prescription medication who are suffering from pseudoaddiction are extremely difficult to differentiate from those of patients with prescription medication addiction, particularly in the acute care setting.30 As a result, we made no attempt in our study to determine the cause of a patient’s behaviors, and simply focused on the different behaviors associated with drug-seeking regardless of the cause.
Lastly, it is important to consider whether or not the data presented here may be comparable to patient populations at other sites. Previous research by McNabb et al on a group of 37 drug-seeking patients at an urban tertiary care center consisted of approximately 50% males, with an average age of 39.5 years.27 Furthermore, previous research by Zechnich et al on a group of 30 drug-seeking patients at an urban academic medical center consisted of 50% males, with an average age of 34.3 years.10 Our study population consisted of more women and was slightly older than these 2 populations, but does not seem to vary markedly from these 2 previous study groups. The institution from which our data comes is a community hospital in a moderate-sized suburban city, which likely makes it most applicable to other community hospitals in such a setting.
LIMITATIONS
Our study had several limitations, which should be taken into consideration when reviewing the data presented. First, in performing a chart review, the quality of the data is dependent on the quality of physician and nursing documentation, which may lack completeness or uniformity. It also may be biased in that a care provider who suspects a patient is drug-seeking may be more likely to document particular behaviors or actions. Possible variations in the quality of the documentation by physicians and nurses could also be attributed to experience level, burnout, familiarity with the patient, overall patient load, and time needed to document drug-seeking behaviors appropriately.
Second, it is nearly impossible to assess whether or not our patients were suffering from addiction or pseudoaddiction, as both groups may exhibit drug-seeking behavior. As such, we do not know the prevalence of pseudoaddiction in our study group, which may limit how applicable our data is to the consideration of addiction in the ED. As mentioned above, the prevalence of drug-seeking behaviors in our study might not be generalizable to other drug-seeking patient populations, such as those seeking to sell medication for profit. Additionally, frequent users may decide not to come into the ED based on a particular physician or nurse working at the time, which could impact the prevalence of documented behaviors.
Third, the patients in our study consisted of patients exhibiting drug-seeking behavior who were also predominantly frequent users of a single ED. Our results may be poorly applicable to drug-seeking patients making a single visit to an ED or patients who frequent multiple ED. Additionally, we used patients in an existing case management program as our study population. Enrollment criteria for this program were not clearly defined and included physician or nursing concern as enrollment criteria, which may have been a source of bias in selecting our study group. As it pertains to the methodology of our research, we used a single physician reviewer to perform data abstraction from all charts, which may have been a source of bias. Finally, we only looked at each drug-seeking behavior in isolation. We did not record the number of times a patient exhibited more than 1 behavior at a single visit.
The authors recognize that there are several limitations to the study, which provides the possibility for bias and error in a number of places. However, when trying to study a condition (drug-seeking behavior) for which there is no confirmatory test or diagnostic criteria, conducting research is difficult. While our study design and methodology has a number of limitations unrelated to the behaviors we are trying to study, our hope is that we can provide some preliminary data on a subject of increasing public health concern and a subject that will require much research in the future. We hope that our study can be hypothesis-generating for other researchers.
Directions for future research
Despite the limitations of this study, our data suggests that the reliance on the use of classic drug-seeking behaviors may only help identify a minority of drug-seeking patients. Although prospective research is needed to confirm these results, the data begin to illuminate a much larger question of whether our reliance on the use of drug-seeking behaviors as a means of identifying drug-seeking patients is an efficient and reliable method to decrease irresponsible administration of narcotics. Moreover, there are unintended consequences of our system’s current reliance on the use of drug-seeking behaviors as a primary means of identifying these patients. Research suggests that our current ED culture is resulting in the undertreatment of those patients who actually require narcotics to achieve effective and responsible pain control, such as patients with pseudoaddiction.9
As more research continues to highlight the issues associated with responsible pain control in the ED and throughout the healthcare system, there are foreseeable steps in achieving this reality. The ED culture should begin to create a more systematic approach to addressing pain. If a patient presents to the ED with a pain severity requiring narcotics administration, the EP should consider checking his or her habitual patient files/case management program or prescription monitoring record. This can empower the physician to help identify true drug-seeking patients instead of relying simply on the seemingly unreliable classic drug-seeking behaviors. We plan to research whether the use of a habitual patient files/case management program/or alternative data system is a more reliable method of identifying these patients.
CONCLUSION
Drug-seeking patients appear to exhibit “classically” described drug-seeking behaviors with only low to moderate frequency, with each of the studied behaviors in this study being recorded as present in less than one third of all ED visits. This data suggests that reliance on historical features of a patient encounter may be inadequate when trying to assess whether or not a patient is drug-seeking.
Footnotes
Supervising Section Editor: Christopher Kang, MD
Submission history: Submitted December 15, 2011; Revision recieved March 8, 2012; Accepted April 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.11600
Address for Correspondence: Casey A. Grover, MD, Standford Kaiser Emergency Medicine Residency, Department of Emergency Medicine, 300 Pasteur Dr., Alway Building Room M121, Stanford, CA 94305
Email: caseygrover@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Todd KH, Ducharme J, Choiniere M, et al. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain.2007;8:460–6. [PubMed]
2. Pletcher MJ, Kertesz SG, Kohn MA, et al. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;29:70–8. [PubMed]
3. O’Connor AB, Zwemer FL, Hays DP, et al. Outcomes after intravenous opioids in emergency patients: a prospective cohort analysis. Acad Emerg Med. 2009;16:477–87.[PubMed]
4. Nourjah P. National hospital ambulatory medical care survey: 1997 emergency department summary. Adv Data. 1999;304:1–24. [PubMed]
5. Wilson JE, Pendleton JM. Oligoanalgesia in the emergencydepartment. Am J Emerg Med. 1989;7:620–3. [PubMed]
6. Rupp T, Delaney KA. Inadequate analgesia in emergency medicine. Ann Emerg Med.2004;43:494–503. [PubMed]
7. Tamayo-Sarver JH, Dawson NV, Cydulka RK, et al. Variability in emergency physician decision making about prescribing opioid analgesics. Ann Emerg Med.2004;43:483–93. [PubMed]
8. Hawkins SC, Smeeks F, Hamel J. Emergency management of chronic pain and drug-seeking behavior: an alternative perspective. J Emerg Med. 2008;34:125–9. [PubMed]
9. Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: Are we ever going to get better? J Pain Res. 2009;2:5–11. [PMC free article][PubMed]
10. Zechnich AD, Hedges JR. Community-wide emergency department visits by patients suspected of drug-seeking behavior. Acad Emerg Med. 1996;3:312–7. [PubMed]
11. McCaffery M, Grimm MA, Pasero C, et al. On the meaning of “drug seeking” Pain Manag Nurs. 2005;6:122–36. [PubMed]
12. Carlson MJ, Baker LH. Difficult, dangerous, and drug-seeking: the 3D way to better patient care. Am J Public Health. 1998;88:1250–2. [PubMed]
13. Geiderman JM. Keeping lists and naming names: habitual patient files for suspected nontherapeutic drug-seeking patients. Ann Emerg Med. 2003;41:873–81. [PubMed]
14. Pope D, Fernandes CM, Bouthillette F, et al. Frequent users of the emergency department: a program to improve care and reduce visits. CMAJ. 2000;162:1017–20.[PMC free article] [PubMed]
15. Grover CA, Close RJ, Villarreal K, et al. Emergency department frequent user: pilot study of intensive case management to reduce visits and computed tomography. West J Emerg Med. 2010;11:336–343. [PMC free article] [PubMed]
16. Taverner D, Dodding CJ, White JM. Comparison of methods for teaching clinical skills in assessing and managing drug-seeking patients. Med Educ. 2000;34:285–91. [PubMed]
17. Gianutsos LP, Safranek S, Huber T. Clinical inquiries: is there a well-tested tool to detect drug-seeking behaviors in chronic pain patients? J Fam Pract. 2008;57:609–10.[PubMed]
18. Chou R, Fanciullo GJ, Fine PG, et al. Opiods for chronic noncancer pain: prediction and identification of aberrant drug-related behaviors: a review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guideline. J Pain. 2009;10:131–46. [PubMed]
19. Moore TM, Jones T, Browder JH, et al. A comparison of common screening methods for predicting aberrant drug-related behavior among patients receiving opiods for chronic pain management. Pain Med. 2009;10:1426–33. [PubMed]
20. Wu SM, Compton P, Bolus R, et al. The addiction behaviors checklist: validation of a new clinician-based meaure of inappropriate opioid use in chronic pain. J Pain Symptom Manage. 2006;32:342–51. [PubMed]
21. Butler SF, Budman SH, Fernandez KC, et al. Development and validation of the Current Opioid Misuse Measure. Pain. 2007;130:144–156. [PMC free article] [PubMed]
22. Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med. 2005;6:432–42. [PubMed]
23. Butler SF, Fernandez K, Benoit C, et al. Validation of the revised Screener and Opioid Assessment for Patients with Pain (SOAPPR) J Pain. 2008;9:360–72. [PMC free article][PubMed]
24. Belgrade MJ, Schamber CS, Lindgren BR. The DIRE score: predicting outcomes of opiod prescribing for chronic pain. J Pain. 2006;7:671–81. [PubMed]
25. McNabb C, Foot C, Ting J, et al. Diagnosing drug-seeking behavior in an adult emergency department. Emerg Med Australas. 2006;18:138–42. [PubMed]
26. Chan L, Winegard B. Attributes and behaviors associated with opioid seeking in the emergency department. J Opioid Manag. 2007;3:244–8. [PubMed]
27. McNabb C, Foot C, Ting J, et al. Profiling patients suspected of drug seeking in an adult emergency department. Emerg Med Australas. 2006;18:131–7. [PubMed]
28. Ossipov MH, Lai J, Vanderah TW, et al. Induction of pain facilitation by sustained opioid exposure: relationship to opioid antinociceptive tolerance. Life Sci. 2003;73:783–800. [PubMed]
29. Grover CA, Close RJ, Wiele ED, et al. Quantifying drug seeking behavior: a case control study. J Emerg Med. 2012;42:15–21. [PubMed]
30. Sim MG, Hulse GK, Khong E. Acute pain and opioid seeking behavior. Aust Fam Physician. 2004;33:1009–12. [PubMed]
31. Hansen GR. The drug-seeking patient in the emergency room. Emerg Med Clin North Am. 2005;23:349–65. [PubMed]
32. Longo LP, Parran T, Jr, Johnson B, et al. Addiction: part II. Identification and management of the drug-seeking patient. Am Fam Physician. 2000;61:2401–8.[PubMed]
33. Substance Abuse and Mental Health Services Administration Results from the 2009 National Survey on Drug Use and Health: Volume I Summary of National Findings (Office of Applied Studies, NSDUH Series H-38A, HHS Publication No SMA 10-4586Findings)Rockville, MD: 2010.
34. Substance Abuse and Mental Health Services Administration, Office of Applied Studies Drug Abuse Warning Network, 2006: National Estimates of Drug-Related Emergency Department Visits. DAWN SeriesD-30, DHHS Publication No. (SMA) 08-4339.Rockville, MD: 2008.
35. Webster LR, Cochella S, Dasgupta N, et al. An analysis of the root causes for opioid-related overdose deaths in the United States. Pain Med. 2011;12(Suppl 2):S26–S35.[PubMed]
36. Baehren DF, Marco CA, Droz DE, et al. A statewide prescription monitoring program affects emergency department prescribing behaviors. Ann Emerg Med. 2010;56:19–23.[PubMed]