| Author | Affiliation |
|---|---|
| Lynn E.J Gower, DO | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis (Tacoma), Washington |
| Medley O’Keefe Gatewood, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis (Tacoma), Washington |
| Christopher S. Kang, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis (Tacoma), Washington |
ABSTRACT
An increasing number of elderly patients are presenting to the emergency department. Numerous studies have observed that emergency physicians often fail to identify and diagnose delirium in the elderly. These studies also suggest that even when emergency physicians recognized delirium, they still may not have fully appreciated the import of the diagnosis. Delirium is not a normal manifestation of aging and, often, is the only sign of a serious underlying medical condition. This article will review the significance, definition, and principal features of delirium so that emergency physicians may better appreciate, recognize, evaluate, and manage delirium in the elderly.
BACKGROUND
The elderly, defined as 65 years of age and older, are rapidly representing a larger portion of the population in the United States. In 2000, they numbered 34.6 million, or 12% of the population. By the mid-21st century, this number will increase to 82 million, or 20% of the population,1,2 It is estimated that 10% to 30% of the elderly evaluated in the emergency department (ED) will present with delirium.3–5 The prevalence might be even higher, as patients who are unable to communicate due to critical illness or are unable to cooperate are excluded from many studies.6 Several other studies have suggested that emergency physicians are “suboptimal” at recognizing mental status impairment in the elderly as well as eliciting signs and symptoms necessary to diagnose delirium.6–8 Physicians correctly diagnose delirium in only 24% to 35% of elderly patients,3,4,8 with one study revealing that nearly half of the patients with delirium were discharged with little consideration that delirium could be the harbinger of a serious underlying medical condition.7 Failure to detect delirium in the elderly in the ED and subsequent discharge has the potential for increased mortality within 6 months of discharge.9Several authors also noted that even when delirium was diagnosed, some patients were still inappropriately discharged. The high prevalence of impaired mental status combined with the number of elderly patients with delirium discharged has led some experts to suggest that age alone should be a criterion for screening the elderly for delirium through the use of a formal mental status evaluation.10Elderly patients diagnosed with delirium in the ED had a 12-month mortality rate of 10% to 26%.6,11,12Similar mortality rates have been observed with acute myocardial infarction and sepsis.5 In addition, delirious elderly patients tend to have poorer outcomes and their short-term risk of mortality increases when compared with their nondelirious counterparts.4,7,13 A recent meta-analysis found that delirium in the elderly is independently associated with poorer outcomes, regardless of factors such as other illnesses and baseline dementia.14 Even when admitted, older patients ultimately diagnosed with delirium have increased mortality during the 12 months following hospital admission. Delirium was identified to be an independent risk factor of increased mortality, and especially significant if underlying dementia was absent.12 Cognitive impairment is not considered a normal part of the aging process. As a result, emergency physicians should recognize delirium, even if subtle, as a medical emergency. Early diagnosis, treatment, and the appropriate disposition of the delirious elderly patient may facilitate a faster recovery and more desirable longer-term outcomes.11
DEFINING DELIRIUM
Delirium is a syndrome defined by the American Psychiatric Association as “a disturbance of consciousness and a change in cognition that develops over a short period of time.”15 Delirium is derived from the Latin word “delirare,” which literally means, “to go out of the furrow” or figuratively, “crazy or deranged.”16 Thus, delirium is a transient cerebral dysfunction resulting in an acute reversible decline in attention and cognition. Delirium may manifest itself clinically in the hyperactive, the hypoactive, or the mixed form.11 The hyperactive form is identified by agitation, increased vigilance, and hallucinations. The hypoactive form is associated with lethargy and reduced psychomotor functioning. Often, this leads the caregiver or practitioner to believe that the patient is doing fine due to the lack of any sign of discomfort or distress. Unfortunately, the hypoactive form is more common and generally portends a poorer prognosis. In the mixed form of delirium, characteristics from both the hyperactive and hypoactive forms are manifested. Special care must be given to patients with the mixed form of delirium, as they may vacillate unpredictably and can be especially difficult to manage.5,8,16
ETIOLOGY
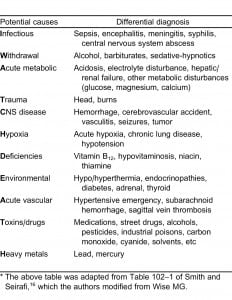
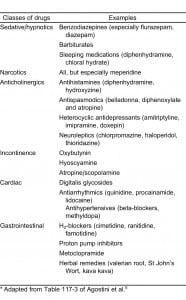
The etiology of delirium in the elderly is multifactorial as any one or more predisposing and precipitating factors may be involved (Table 1). As compared to a younger, healthier patient, an elderly patient can enter a delirious state when exposed to a simple noxious insult or precipitating event. Predisposing factors include advanced age, preexisting cognitive impairment/dementia, severe underlying illness (eg, chronic renal insufficiency), functional impairment, male gender, depression, dehydration/malnutrition, alcohol abuse, and sensory impairment (vision or hearing). In addition to a noxious insult such as acute pain, other precipitating factors include medication use, acute medical illness or infection, immobilization or the use of physical restraints, urinary retention or Foley catheterization,17dehydration, environmental factors, alcohol/drug use, and psychosocial factors.18–21 One of the most common causes of delirium in the elderly is the use of medications (Table 2), especially routinely prescribed medications (psychoactive agents such as benzodiazepines, narcotic analgesics, and drugs with anticholinergic effects),18–26 with an overall incidence of 22% to 39%.16 Living in a nursing home has also been identified as an independent risk factor for delirium, as up to 40% of nursing home residents will experience delirium, usually from an infection.18
Commonly noted signs and symptoms for certain ailments are not always evident in the elderly. For example, an elderly patient may be experiencing respiratory difficulty, but not have dyspnea or tachypnea, or an acute myocardial infarction without the expected classic complaint of chest pain. Pneumonia, urinary tract infection, endocarditis, abdominal abscess, and infected joints have all been diagnosed in elderly patients who were afebrile and did not have an elevated white blood cell count.5 In short, a “common herald” of a physical illness in the elderly may be the onset of an acute confusional state, rather than the signs and symptoms classically associated with a particular illness.16
Studies involving electroencephalograms, evoked-potential studies, neuroimaging, and other modalities suggest that neurotransmitter abnormalities are associated with delirium.5 At the cellular level, widespread alterations in cerebral metabolic activity with secondary deregulation of neurotransmitter synthesis and metabolism are present. The elderly appear especially vulnerable to cerebral biochemical alteration. Although multiple neurotransmitters have been implicated, the most prominent agent in the development of delirium is acetylcholine. Delirium is frequently caused by anticholinergic drugs, and increased serum anticholinergic activity has been demonstrated in delirious elderly patients.5,22,23Elevated serotonin levels have been identified in patients with sepsis, hepatic encephalopathy, serotonin syndrome, and psychedelic drug ingestion. Other disturbances associated with delirium are cytokine increases and oxidative metabolism substrate disturbances (eg, glucose, oxygen, gamma-aminobutyric acid, cortisol, dopamine, beta endorphins).5
DIAGNOSING DELIRIUM
Diagnosing delirium in the elderly requires recognition of the syndrome and a systematic approach (Figure).27 Some patients are obviously delirious. Patients who present without overt delirium pose a more difficult diagnostic challenge, especially when information or patient corroboration is limited. Most etiologies of delirium may be uncovered by a guided history and physical examination, with special emphasis on medication history, combined with focused ancillary testing and a search for occult infection.5 An important caveat to remember is that a delirious person may be oriented to person, place, and time, but that apparent alertness and orientation do not preclude delirium. Eliciting a more subtle presentation may require more substantial questioning.11 Unfortunately, early or evolving baseline dementia may complicate initial evaluation.

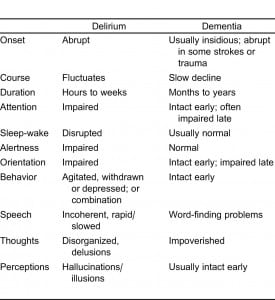
Dementia may be distinguished from delirium (Table 3)28 by the tempo of onset, clinical course, level of attention and consciousness, orientation, and changes in speech patterns. For dementia, onset is insidious and progressive, occurring over months to years. The course usually does not fluctuate throughout the day, and inattention and disorientation are not usually observed until the latter stages of dementia. A demented individual’s speech may be marked by parsimony, anomia, or even aphasia, while a delirious person will talk incoherently, illogically, and have dysnomia. Dysnomia (the inability to name objects correctly) and dysgraphia (impaired writing ability) are 2 of the most sensitive indicators of delirium.16 In summary, the hallmark of delirium is the acute onset (hours to days) of changes in attention and cognition.
HISTORY TAKING
Detailed history-taking may also require interviewing multiple people, including the prehospital providers who evaluated and transported the patient to the ED, family members, and other caregivers. It is critical to ascertain the patient’s cognitive baseline, the recent sequence of events, any history of similar problems or prior episodes, new medications (including prescribed medications, dietary supplements, and over-the-counter agents), and any history of alcohol use or substance abuse. Past medical history and comorbid conditions, such as diabetes, hypertension, and any immunosuppressive disease should be confirmed.5,16 A comprehensive review of systems should then be conducted since, as noted above, the elderly may often report vague or nonspecific complaints, such as weakness.29 The patient’s baseline activities of daily living (ADL) should also be verified. The normal progression of functional decline or inability to perform these activities typically occurs in the following manner: bathing, dressing, toileting/continence, transferring (bed/chair), and, lastly, feeding. If difficulty with a specific ADL occurs acutely or out of order (eg, an elderly patient has decreased ability to feed but can still dress), an underlying medical condition should be suspected.29
PHYSICAL EXAMINIATION
A thorough physical examination is essential, especially if the cause of delirium is not obvious. As with any patient, observation of the patient’s general behavior should be conducted as subtle or obvious abnormalities in breathing, walking, and reactions to activity or conversations in the room may be noted. Delirious patients are easily distracted and have difficulty maintaining focus and performing simple repetitive tasks, such as counting backwards from 100 by 7s or reciting the days of the week or months backwards. They will often perseverate, not be able to follow a conversation, and answer a question with the response given to a previous question.16 Delirious patients are usually oriented to person, but not to time and/or place. They may also manifest memory impairment, especially short-term, and the inability to assimilate new information. Disorganized thought processes and speech (disjointed or incoherent speech, an unclear or illogical progression of ideas), sleep-wake cycle disturbances, and perceptual disturbances may also be reported or observed. There may be a misperception of the environment with poorly formed delusions and hallucinations. Emotions may also be affected and can become quite labile. The delirious person can have a decreased capacity to modulate fine emotional expression. Also, a significant portion of confused patients will have impairments with spelling, writing, and spatial organization.5,16
Standard questions should assess orientation to person, time, place, and self, as well as 3-item recall. These should then be followed by more in-depth questioning if cognitive impairment is noted.16,29 The assessment methods most cited in research are the Mini-Mental State Examination (MMSE) and the Confusion Assessment Method (CAM).8,30 The MMSE involves a series of questions that elicit a maximum score of 30 points and can be performed in less than 5 minutes. The areas tested are: orientation, registration, attention and calculation, recall, and language and praxis. A score of 23 or below indicates organic brain syndrome.16 The CAM scale (Table 4)31 assesses 4 criteria: acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness. Diagnosis of delirium requires the presence of the first 2 criteria and either the third or the fourth criteria.29 The CAM scale has a sensitivity of 93% to 100% and a specificity of 90% to 95%.30

Bedside cognitive tests have some limitations. The MMSE lacks questions evaluating executive function. Patients with mild impairment can pass the test. To offset this limitation, the patient’s category fluency (eg, name as many animals as possible in 1 minute) and phonemic fluency (eg, name as many words beginning with the letter “F” in 1 minute) should be tested. Furthermore, cognitive tests may also be affected by the patient’s general intelligence or level of education.16
The physical examination should continue in a head-to-toe systematic fashion with a keen eye toward findings that may mark an underlying precipitant condition. Common examination findings causing delirium in the elderly include, but are not limited to, urinary retention, constipation/fecal impaction, and sources of occult infection.16 The simple procedure of relieving urinary retention (in men) can sometimes resolve an episode of delirium. The most common reversible cause of geriatric urinary retention is constipation/fecal impaction.17 The elderly person has increased susceptibility to infection and may have an atypical disease presentation, such as lack of focal signs and symptoms of an infection, isolated fever, or hypothermia, instead of hyperthermia. Common infection sites are the lungs, abdomen, urinary tract, and skin.23
DIAGNOSTIC TESTING
Ancillary testing should be ordered as indicated by clinical examination, and usually include blood oxygen saturation, complete blood count, chemistry panel, urinalysis, and a chest radiograph. An electrocardiogram should also be obtained because there is a higher risk of silent myocardial infarction in the elderly population.16 Elderly patients with cognitive dysfunction warrant special consideration as to whether or not they should undergo a lumbar puncture. The classic meningeal findings of fever, headache, and stiff neck are often absent.16,32 A retrospective chart review studied the utility of lumbar puncture (LP) to detect meningitis in elderly patients with altered mental status, including those afebrile on presentation. The results indicated that 18% (15/84) of the afebrile patients had meningitis versus 24% of the febrile patients, prompting the authors to suggest consideration of an LP in all elderly patients with altered mental status, even if afebrile. They also acknowledged that a limitation of the chart review design is the inability to ascertain whether information in the patient’s history or examination would provoke the physician to perform an LP, even in the absence of a fever.32
Finally, additional studies worth considering are: arterial blood gas (hypercarbia, hypoxia), thyroid function tests (hypothyroid and hyperthyroid), liver function tests (liver failure, encephalopathy), blood alcohol level, drug levels (intoxication), toxin screens (overdose), rapid plasma reagin test (syphilis), vitamin B12 and folic acid (metabolic deficiencies) levels, and carbon monoxide level (hypoxia, poisoning)4,15 (Figure).
MANAGEMENT OF CAUSES OF DELIRIUM REQUIRING EMERGENT ATTENTION
Initial management of the delirious patient should start with the standard assessment of airway, breathing, circulation, and, if indicated, cervical spine precautions. Intravenous access, cardiac monitoring, and simultaneous screening for readily reversible causes, such as hypoglycemia, hypoxia, and excessive opioid use should be initiated. Elderly patients with multisystem trauma may present with initially normal vital signs prior to a precipitous clinical deterioration.24 An acute ischemic stroke and other neurologic conditions, such as Wernicke encephalopathy, should not be overlooked.16
For elderly patients with hyperactive delirium, chemical restraints may be required to complete the examination, perform vital tests or procedures, or for personal safety. Haloperidol, a starting dose of 0.5 to 1.0 mg, may be effective. However, haloperidol should be used with caution in elderly patients with acute coronary ischemia, decompensated congestive heart failure, or those taking medications associated with QTc prolongation.16 A QTc of less than 440 msec, however, is believed to have a decreased risk of dysrhythmia.33 A prospective study that evaluated the effectiveness of haloperidol versus lorazepam, and the combination of both agents, in the treatment of psychotic agitation demonstrated that the use of both medications appeared to be more effective during the first hours of treatiment.34 In contrast, a 2004 treatment algorithm for ED patients who presented with acute psychotic agitation requiring chemical restraint suggested that the use of lorazepam in the elderly or cognitively impaired should be avoided, unless the cause of their agitation was due to sedative or alcohol withdrawal.35 The newer atypical antipsychotics, such as risperidone or olanzapine, may also be effective and tend to have fewer extrapyramidal side effects. Risperidone is predominantly used in the elderly, with a recommended starting dose of 0.25 to 0.50 mg.16,36 The use of physical restraints should be avoided. If necessary, the use of physical restraints for elderly patients should be temporary, as it may contribute to delirium.16
When providing analgesia, morphine should be used judiciously since any associated dysphoria, respiratory depression, and hepatic encephalopathy may be more pronounced in elderly patients. Similarly, diazepam should be avoided, except in alcohol or sedative hypnotic withdrawal, due to its long half-life and the increased potential for respiratory depression.16 Other simple, but often overlooked, measures to facilitate the evaluation and management of delirious elderly patients include adequate lighting, close monitoring with one-to-one support (ideally a family member or caregiver, or someone else the person knows), a quiet environment to decrease sensory overload, the use of hearing aids/glasses, and addressing the patient by name (Figure).
DISPOSITION
Younger patients with delirium are more likely to be diagnosed as well as to recover fully, although mild cognitive dysfunction may linger for some time. As already noted, elderly patients with delirium generally do not fare as well and usually experience a persistent decline in their baseline level of functioning. They also tend to have longer hospital stays, higher rates of institutionalized care, increased long-term mortality risk, and lose one or more ADLs.16,37 One article asserts that any elderly patient with delirium should be admitted for definitive diagnosis and treatment, unless the cause is easily reversible or the delirium abates while in the ED.38
CONCLUSION
Delirium in elderly patients can manifest subtly and often may be the only sign of an underlying serious and potentially life-threatening illness. Numerous studies have revealed that emergency physicians are not proficient at recognizing and diagnosing delirium in elderly patients or that they believe the condition is a normal process of aging. Most causes of delirium are usually readily reversible. However, if not diagnosed and treated promptly, delirium in elderly patients is associated with strikingly elevated morbidity and mortality rates.
Emergency physicians should also be cognizant that many delirious elderly patients warrant and benefit from admission. As the number of elderly patients presenting to EDs continues to increase, emergency physicians must strive to better appreciate, identify, and manage delirium in the elderly.
Footnotes
Supervising Section Editor: Teresita M. Hogan, MD
Submission history: Submitted October 6, 2010; Revision received March 6, 2011; Accepted October 3, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.10.6654
Address for Correspondence: Lynn E.J. Gower, DO
Madigan Army Medical Center, Department of Emergency Medicine, Bldg 9040, Fitzsimmons Dr, Fort Lewis (Tacoma), WA 98431
E-mail: lynn.gower@us.army.mil
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none. The views expressed are those of the authors and do not reflect the official policy of the Department of the Army, the Department of Defense, or the US Government.
REFERENCES
1. US Census Bureau. Americans are living longer: a trend that is expected to continue. 2010 The American Geriatrics Society Web site. Available at:http://www.americangeriatrics.org/files/documents/stats/slide_3_5.pdf. Accessed August 20.
2. Wilber ST, Gerson LW, Terrell KM, et al. Geriatric emergency medicine and the 2006 Institute of Medicine reports from the Committee on the Future of Emergency Care in the U.S. health system. Acad Emerg Med. 2006;13:1345–1351. [PubMed]
3. Elie M, Rousseau F, Cole M, et al. Prevalence and detection of delirium in elderly emergency department patients. CMAJ. 2000;163:977–981. [PMC free article] [PubMed]
4. Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39:248–253. [PubMed]
5. Agostini JV, Inouye SK. Delirium. Principles of Geriatric Medicine & Gerontology. In: Hazzard WR, Blass JP, Halter JB, et al., editors. New York, NY: McGraw-Hill; 2003. pp. 1503–1515. eds. 5th ed.
6. Hustey FM, Meldon SW, Smith MD, et al. The effect of mental status screening on the care of the elderly emergency department patients. Ann Emerg Med. 2003;41:678–684. [PubMed]
7. Lewis LM, Miller DK, Morley JE, et al. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13:142–145. [PubMed]
8. Han JH, Zimmerman BA, Cutler N, et al. Delirium in older emergency department patients: recognition, risk, factors, and psychomotor subtypes. Acad Emerg Med. 2009;16:193–200. [PubMed]
9. Kakuma R, du Fort GG, Arsenault L, et al. Delirium in older emergency department patients discharged home: effect on survival. J Am Geriatr Soc. 2003;51:443–450. [PubMed]
10. Naughton BJ, Moran MB, Kadah H, et al. Delirium and other cognitive impairment in older adults in an emergency department. Ann Emerg Med. 1995;25:751–755. [PubMed]
11. Alagiakrishnan K, Blanchette P. 2010 Delirium. eMedicine Web site. Available at:http://emedicine.medscape.com/article/288890-overview. Accessed April 15.
12. McCusker J, Cole M, Abrahamowicz M, et al. Delirium predicts 12-month mortality. Arch Intern Med. 2002;162:457–463. [PubMed]
13. Han JH, Shintani A, Eden S, et al. Delirium in the emergency department: an independent predictor of death within 6 months. Ann Emerg Med. 2010;56:244–252. e1. [PubMed]
14. Witlox J, Eurelings LSM, de Jonghe JFM, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304:443–451. [PubMed]
15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Chicago, IL: American Psychiatric Association; 2000. pp. 135–147.
16. Smith J, Seirafi J. Delirium and dementia. Rosen’s Emergency Medicine Concepts and Clinical Practices. 7th ed. In: Marx JA III, Hockberger RS, Walls RM, editors. Philadelphia, PA: Elsevier; 2010. pp. 1367–1373. eds.
17. Thorne MB, Geraci SA. Acute urinary retention in elderly men. Am J Med. 2009;122:815–819.[PubMed]
18. Han JH, Morandi A, Ely EW. Delirium in the nursing home patients seen in the emergency department. J Am Geriatr Soc. 2009;57:889–894. [PubMed]
19. Inouye SK, Viscoli CM, Horwitz RI, et al. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med. 1993;119:474–481. [PubMed]
20. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275:852–857. [PubMed]
21. Inouye SK. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement Geriatr Cogn Disord. 1999;10:393–400. [PubMed]
22. Han L, McCusker J, Cole M, et al. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch Intern Med. 2001;161:1099–1105.[PubMed]
23. Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–1165. [PubMed]
24. Cerullo M. Expect psychiatric side effects from corticosteroid use in the elderly. Geriatrics.2008;63:15–18. [PubMed]
25. Lin RY, Heacock LC, Fogel JF. Drug-induced, dementia-associated and non-dementia, non-drug delirium hospitalizations in the United States, 1998–2005: an analysis of the national inpatient sample.Drugs Aging. 2010;27:51–61. [PubMed]
26. Van Rompaey B, Elseviers MM, Schuurmans MJ, et al. Risk factors for delirium in intensive care patients: a prospective cohort study. Crit Care. 2009;13:R77. [PMC free article] [PubMed]
27. Francis J. Prevention and treatment of delirium and confusional states. 2011 UpToDate Web site. Available at: http://www.uptodate.com.offcampus.lib.washington.edu/contents/image?imageKey=PC/21653. Accessed February 26.
28. Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic.Emerg Med Clin North Am. 2010;28:611–631. [PubMed]
29. Sanders AB. The elder patient. Emergency Medicine: A Comprehensive Study Guide. 6th ed. In: Tintinalli JE, Kelen GD, Stapczynski JS, editors. New York, NY: McGraw-Hill; 2004. pp. 1896–1900. eds.
30. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detections of delirium. Ann Intern Med. 1990;113:941. [PubMed]
31. Francis J, Young GB. Diagnosis of delirium and confusional states. 2011 UpToDate Web site. Available at: http://www.uptodate.com.offcampus.lib.washington.edu/contents/image?imageKey=PC/21891. Accessed February 26.
32. Shah K, Richard K, Edlow JA. Utility of lumbar puncture in the afebrile vs. febrile elderly patient with altered mental status: a pilot study. J Emerg Med. 2007;32:15–18. [PubMed]
33. Rund DA, Ewing JD, Mitzel K, et al. The use of intramuscular benzodiazepines and antipsychotic agents in the treatment of acute agitation or violence in the emergency department. J Emerg Med.2006;31:317–324. [PubMed]
34. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both for psychotic agitation? A multicenter, prospective, double-blind, emergency department study. Am J Emerg Med. 1997;15:335–340. [PubMed]
35. Currier GW, Allen MH, Bunney B, et al. Updated treatment algorithm: algorithm for patients who present to the ED with acute psychotic agitation and require physical or pharmacological restraint. J Emerg Med. 2004;27:S25–26. [PubMed]
36. Smith J, Seirafi J. Delirium and dementia. Rosen’s Emergency Medicine Concepts and Clinical Practices. 6th ed. In: Marx JA III, Hockberger RS, Walls RM, editors. Philadelphia, PA: Elsevier; 2006. pp. 1645–1655. In: eds.
37. Pisani MA, Kong SYJ, Kasl SV, et al. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009;180:1092–1097.[PMC free article] [PubMed]
38. Sanders AB. Recognition of cognitive problems in older adults by emergency medicine personnel.Ann Emerg Med. 1995;25:831–833. [PubMed]


