| Author | Affiliation |
|---|---|
| Jessa Williams, DO | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
| Jason D. Heiner, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
| Michael D. Perreault, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
| Todd J. McArthur, MD | Madigan Army Medical Center, Department of Emergency Medicine, Fort Lewis, WA |
A 45-year-old male with a history of poorly controlled hypertension arrived to the emergency department complaining of ripping chest pain radiating to his back and abdomen. Initial vital signs included a blood pressure of 202/112 mmHg bilaterally and a heart rate of 60 beats/minute. The patient had recently started a new antihypertensive medication regimen, including atenolol and amlodipine. Electrocardiogram and laboratory studies, including a complete blood cell count, serum chemistry panel, troponin, prothrombin time, partial thromboplastin time, lipase, and liver function tests, were unremarkable. On physical exam he had symmetrical peripheral pulses and only mild epigastric tenderness. A portable chest radiograph (CXR) demonstrated a widened mediastinum, and bedside ultrasound showed an intimal flap in the abdominal aorta (Figure 1). Computed tomography (CT) revealed an extensive aortic dissection extending from the descending portion of the aortic arch into both iliac arteries (Figure 2). By convention, this is classified as either a Stanford type B or a DeBakey type III aortic dissection.
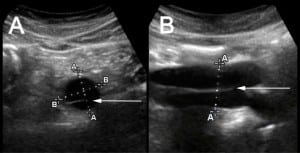
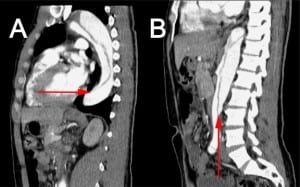
Aortic dissections form when shearing intravascular forces separate the layers of the aortic wall. If untreated, patients with proximal aorta involvement have a two-week mortality rate of approximately 80%.1 The CXR in 12–18% of patients with aortic dissection may be unremarkable.1,2Multi-planar transesophageal echocardiography, magnetic resonance imaging, and CT have largely replaced aortography as diagnostic modalities. Emergency physicians routinely use bedside ultrasound to evaluate the abdominal aorta for aneurysm. Visualization of an intimal flap by ultrasound may carry a sensitivity of 67–80% and specificity of 99–100% for dissection.3 This rapid, non-invasive method of diagnosis may aid in the early detection and treatment of this deadly diagnosis.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted July 6, 2009; Revision Received August 6, 2009; Accepted August 17, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jessa Williams, DO, Depart. of Emerg Med, Madigan Army Medical Center, 9040 Fitzsimmons Ave, Fort Lewis, WA 98431
Email: williamsjessa@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest.2002;122:311–28. [PubMed]
2. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283:897–903. [PubMed]
1. Fojtik JP, Costantino TG, Dean AJ. The diagnosis of aortic dissection by emergency medicine ultrasound. J Emerg Med. 2007;32:191–6. [PubMed]


