| Author | Affiliation |
|---|---|
| J Christian Fox, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Craig L. Anderson, MPH, PhD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Suleman S. Ahmed, BS, BA | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Joanne McDonough, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Warren Wiechmann, MD, MBA | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Michael Waters, MD | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Graciela Barajas, BS | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Shahram Lotfipour, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
ABSTRACT
Introduction:
To determine whether a medical student emergency ultrasound clerkship has an effect on the number of patients undergoing ultrasonography and the number of total scans in the emergency department.
Methods:
We conducted a prospective, single-blinded study of scanning by emergency medicine residents and attendings with and without medical students. Rotating ultrasound medical students were assigned to work equally on all days of the week. We collected the number of patients scanned and the number of scans, as well as participation of resident and faculty.
Results:
In seven months 2,186 scans were done on the 109 days with students and 707 scans on the 72 days without them. Data on 22 days was not recorded. A median of 13 patients per day were scanned with medical students (CI 12–15) versus seven (CI 6–9) when not. In addition, the median number of scans was 18 per day with medical students (CI 16–20) versus eight (CI 6–10) without them.
Conclusion:
There were significantly more patients scanned and scans done when ultrasound medical students were present.
INTRODUCTION
Emergency ultrasonography is part of the core curriculum for emergency medicine (EM) residents.1Prior studies suggest the best way to train residents and attending physicians in emergency ultrasonography is through a combination of didactic and hands-on training.2–10 For example, Mandavia et al.7 states that emergency ultrasound can be taught with a high degree of accuracy with eight hours each of lecture and hands-on training. Lanoix et al.8 states that adequate efficiency can be obtained though a four-hour training course with three hours of hands-on training and a one-hour didactic session. Various policy statements from the American College of Emergency Physicians11, the American Academy of Emergency Medicine12, and the Society for Academic Emergency Medicine (SAEM)13 have proposed different standards for competency. SAEM recommends 40 hours of didactics and 150 scans across all applications.2 Other suggestions range from 25 scans of each primary application to 300–500 total scans.9,10 While all groups agree it is important to encounter pathologic findings for each application, no organization requires this for formal credentialing. Furthermore, skills necessary for competence have not achieved consensus.14Nonetheless, residents cannot learn emergency ultrasonography without hands-on experience.
There are many barriers to resident performance of emergency ultrasonography. An important impediment is time, or its perception.15 For a busy resident, time to scan (locating, cleaning, entering patient information, performing the scan) can seem prohibitive. At our institution, we have a medical student elective in emergency ultrasonography. Fourth-year students spend four weeks under the guidance of a Registered Diagnostic Medical Sonographer-certified, fellowship-trained director and emergency ultrasonography fellow. Students bring the machine to the bedside, perform their own scans, and then repeat the scans with the resident/faculty caring for the patient, for robust clinical teaching.
Our goal was to determine whether a medical student emergency ultrasound clerkship changes the number of patients undergoing ultrasound and the number of scans in the emergency department (ED).
METHODS
This prospective Institutional Review Board-approved study was conducted at a university hospital Level I Trauma Center with an annual ED census of 38,000 patients. All patients who received an emergency ultrasound by ED personnel were eligible. There were no exclusions.
From January 24, 2005 to August 15, 2005, ultrasound students were assigned to specific days of the week, with all days equally represented. The students worked from 7 am to 2 am. EM residents and faculty were not aware that the number of scans was being monitored, nor that students purposely were not scheduled on some days.
We recorded the number of patients scanned, the number of scans done, and if medical students were present that day. Some patients received more than one scan, for example, right upper quadrant and the kidney. We also recorded if a resident or faculty member participated in the scan. We defined participation as presence at the bedside during the scan, regardless of who held the probe. Of note, each trauma patient (approximately 7–8 per day) receives a Focused Assessment of Sonography for Trauma (FAST) regardless of medical student presence. At our institution, it is common to have several physicians/students at the bedside assisting in image acquisition and interpretation.
All scans were done with either a BK Medical Hawk 2102 or Sonosite TITAN machine. Each scan was recorded and reviewed in its entirety during weekly educational sessions in the division of emergency ultrasound led by the emergency ultrasound fellow and the fellowship director.
Research assistants added the total from each day and data were entered into Excel (Microsoft Corporation, Redmond, WA) and analyzed with Stata (version 9.2, StataCorp, College Station, TX). Because we did not expect the number of patients and scans to be normally distributed, we used nonparametric statistics. We compared the number of patients that received scans and the number of scans with and without a medical student present. The distributions of scans and patients with and without a medical student were compared using the Wilcoxon rank sum test. We calculated medians and 95% exact binomial confidence limits for scans and patients with and without a medical student present.
RESULTS
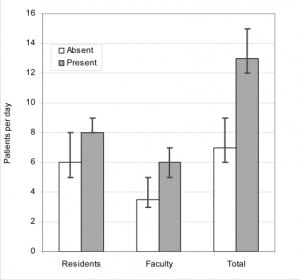
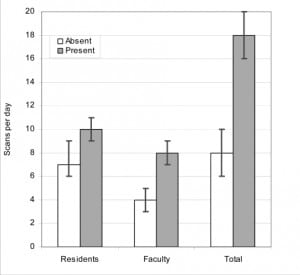
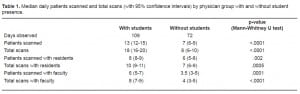
In seven months we performed 2,186 scans on the 109 days when students were present and 707 scans on the 72 days when students were not present. The ultrasound log sheets were missing for 22 days and these were excluded. Statistically more patients were scanned and more scans were performed per day when the medical students were present [patients:(n=13, CI 12–15); scans:(n=18, CI 16–20)] versus when they were not [patients:(n=7, CI 6–9); scans:(n=8, CI 6–10)] (Table 1). Figure 1 represents the median number of patients scanned per day, and Figure 2 represents the median number of scans performed per day.
DISCUSSION
In this prospective, single-blinded non-randomized study of the effect of a medical student rotation on the number of scans performed by faculty and residents, significantly more scans were performed and more patients were scanned when medical students were present.
Much of the literature on training of EM residents cites the need for hands-on training to reach an appropriate competency level.2–12 As the number of scans for any resident increases, accuracy and efficiency increases. Since this study shows a statistical increase in the number of scans, the presence of medical students may contribute to competency in emergency ultrasound.
This residency program far exceeds the SAEM guidelines of 150 scans, requiring a minimum of 500 scans per resident by graduation. Having a medical student ultrasound rotation contributes significantly to fulfilling this requirement. For institutions where residents perform fewer scans, a medical student rotation may significantly increase the number of scans. Further prospective studies should test whether resident competency is enhanced by increasing the number of scans.
LIMITATIONS
This study has several limitations. First, results of a single-site study may not be generalized to other practice settings. Second, FAST scans were performed on trauma patients regardless of medical student presence or day of the week. This factor would act to equalize the number of scans done per day, and not mitigate the statistical difference we found. Third, we collected and reported data for full 24-hour days, but medical students, if assigned, were present only 19 hours per day. This factor would serve to dilute any difference found. We did not correct for the absence of medical students during the early-morning hours. Finally, there were 22 days unaccounted for due to missing log sheets. Had this data been available, it may have altered the results.
CONCLUSION
Our study showed there are statistically more patients scanned and more scans performed in the presence of an ultrasound medical student at our institution. Further prospective studies are needed to test if there are significantly more scans done in other EDs. As mentioned, since the volume of scans is critical for effective education of emergency physicians, implementation of an ultrasound medical student clerkship should be encouraged.
Footnotes
Supervising Section Editor: Seric S. Cusick, MD
Submission history: Submitted March 19, 2008; Revision Received May 26, 2009; Accepted May 27, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: J Christian Fox, MD, RDMS, Department of Emergency Medicine, University of California, Irvine School of Medicine, 101 The City Drive, Rte 128-01, Orange, CA 92868
Email: jchristianfox@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Chapman DM, Hayden S, Sanders AB, et al. Integrating the Accreditation Council for Graduate Medical Education Core competencies into the model of the clinical practice of emergency medicine.Ann Emerg Med. 2004;43:756–69. [PubMed]
2. Mateer J, Plummer D, Heller M, et al. Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med. 1994;23:95–102. [PubMed]
3. Ma OJ, Mateer JR, Ogata M, et al. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879–85. [PubMed]
4. Salen PN, Melanson SW, Heller MB. The focused abdominal sonography for trauma (FAST) examination: considerations and recommendations for training physicians in the use of a new clinical tool. Acad Emerg Med. 2000;7:162–8. [PubMed]
5. Lanoix R, Leak LV, Gaeta T, et al. A preliminary evaluation of emergency ultrasound in the setting of an emergency medicine training program. Am J Emerg Med. 2000;18:41–5. [PubMed]
6. Heller MB, Mandavia D, Tayal VS, et al. Residency training in emergency ultrasound: fulfilling the mandate. Acad Emerg Med. 2002;9:835–9. [PubMed]
7. Mandavia DP, Aragona J, Chan L, et al. Ultrasound training for emergency physicians–a prospective study. Acad Emerg Med. 2000;7:1008–14. [PubMed]
8. Lanoix R, Baker WE, Mele JM, et al. Evaluation of an instructional model for emergency ultrasonography. Acad Emerg Med. 1998;5:58–63. [PubMed]
9. Ali J, Rozycki GS, Campbell JP, et al. Trauma ultrasound workshop improves physician detection of peritoneal and pericardial fluid. J Surg Res. 1996;63:275–9. [PubMed]
10. Costantino TG, Satz WA, Stahmer SA, et al. Predictors of success in emergency medicine ultrasound education. Acad Emerg Med. 2003;10:180–3. [PubMed]
11. American College of Emergency Physicians Use of ultrasound imaging by emergency physicians [policy statement] Ann Emerg Med. 2001;38:469–70. [PubMed]
12. American Academy of Emergency Medicine Performance of emergency screening ultrasound examinations. Common Sense. 1999;6:8.
13. Society for Academic Emergency Medicine. Ultrasound Policy Statement. SAEM Newsletter. 1991 Summer;:2.
14. Counselman FL, Sanders A, Slovis CM, et al. The status of bedside ultrasonography training in emergency medicine residency programs. Acad Emerg Med. 2003;10:37–42. [PubMed]
15. Heegeman DJ, Kieke B., Jr Learning curves, credentialing, and the need for ultrasound fellowships. Acad Emerg Med. 2003;10:404–5. [PubMed]


