| Author | Affiliation |
|---|---|
| Brent M. Felton, DO | Michigan State University, Department of Emergency Medicine, Lansing, Michigan |
| Josh M. White, MD | Michigan State University, Department of Emergency Medicine, Lansing, Michigan |
| Michael A. Racine, MD | Michigan State University, Department of Emergency Medicine, Lansing, Michigan |
ABSTRACT
Superior mesenteric artery (SMA) syndrome is a rare cause of abdominal pain, nausea and vomiting that may be undiagnosed in patients presenting to the emergency department (ED). We report a 54-year-old male presenting to a community ED with abdominal pain and the subsequent radiographic findings.The patient’s computed tomgraphy (CT) of the abdomen and pelvis demonstrates many of the hallmark findings consistent with SMA syndrome, including; compression of the duodenum between the abdominal aorta and superior mesenteric artery resulting in intestinal obstruction, dilation of the left renal vein, and gastric distension. Patients diagnosed with SMA syndrome have a characteristically short distance between the superior mesenteric artery and the aorta (usually 2–8 mm) in contrast to healthy patients (10–34 mm). Our patient’s aortomesenteric distance was measured to be approximately 4 mm. Furthermore, the measured angle between the superior mesenteric artery and the aorta is reduced in patients with SMA syndrome from a normal range of 28°–65° to a measurement between 6°–22°. Our patient’s aortomesenteric angle was difficult to measure secondary to poor sagittal reconstructions, but appears to be approximately 30°. Following radiographic evidence suggesting SMA syndrome together with our patient’s constellation of presenting symptoms, a diagnosis of SMA syndrome was made and the patient was admitted to the general surgery service. However, our patient decided to leave against medical advice owing to improvement of his symptoms following the emptying of two liters of gastric contents via nasogastric tube evacuation.
A 54-year-old male presents with a chief complaint of frequent vomiting for 20 hours after drinking alcohol. Previous medical history was significant for peptic ulcer disease statuspost perforation and surgical repair 1 year ago. On exam, vital signs were within normal limits. Physical exam revealed a distended abdomen with diffuse guarding and tenderness. Laboratory studies were within normal limits. A computed tomography (CT) of the abdomen and pelvis was ordered to further evaluate the etiology of the patient’s symptoms revealing a severely distended stomach and distal duodenum with obstruction at the level of the superior mesenteric artery. These findings are consistent with superior mesenteric artery syndrome.
Superior mesenteric artery syndrome (SMA syndrome) is the result of compression of the third portion of the duodenum between the superior mesenteric artery and the abdominal aorta. Radiographically, SMA syndrome is characterized by several findings; compression of the duodenum between the abdominal aorta and superior mesenteric artery (Figure), dilation of theleft renal vein, and distension of the stomach. In normal patients, the distance between the aorta and SMA (aortomesenteric distance) is 10–34 mm with aortomesenteric angle of 28°–65°.1 Our patient had an aortomesenteric distance of approximately 4 mm (2–8 mm is common in patients with SMA syndrome) with an aortomesenteric angle of approximately 30° (Figure).1 Most cases occur in patients with weight loss due to a variety of reasons (surgery, malabsorption, trauma, etc.) reducing superior mesenteric fat stores.2,3,5 Common presenting symptoms include post-prandial abdominal pain, anorexia, nausea, emesis and subsequent weight loss.2–5 Surgical interventions (duodenojejunostomy most commonly) are employed if conservative measures fail.2,3 Our patient underwent nasogastric tube placement with suction resulting in evacuation of 2 liters of gastric contents and was admitted to general surgery only to leave against medical advice 4 hours following admission as his symptoms had resolved.
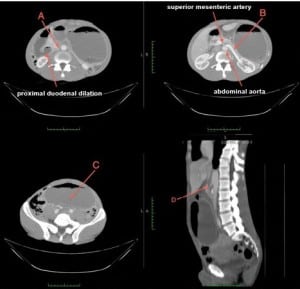
Computed tomography of the abdomen and pelvis demonstrating compression of the duodenum between the abdominal aorta and superior mesenteric artery (A), dilation of the left renal vein (B), distension of the stomach (C), and the aortomesenteric angle (D).
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted June 5, 2012; Accepted June 25, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.6.12762
Address for Correspondence: Brent M. Felton, DO, Michigan State University, Department of Emergency Medicine, 401 W. Greenlawn, Lansing, MI 48910
Email: feltonbr@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Agrawal GA, Johnson PT, Fishman EK. Multidetector row CT of superior mesenteric artery syndrome. J Clin Gastroenterol. 2007;41:62–5. [PubMed]
2. Pasumurthy LS, Ahlbrandt DE, Srour JW. Abdominal pain in a 20-year-old woman.Cleve Clin J Med. 2010;771:45–50.
3. Rudinsky SL, Matteucci MJ. Emergency department presentation of superior mesenteric artery syndrome: two cases in marine corps recruits. J Emerg Med.2012;42:155–8. [PubMed]
4. Lippl F, Hannig C, Weiss W, et al. Superior mesenteric artery syndrome: diagnosis and treatment from the gastroenterologist’s view. J Gastroenterol. 2002;37:640–3. [PubMed]
5. Raman SP, Neyman EG, Horton KM, et al. Superior mesenteric artery syndrome: spectrum of CT findings with multiplanar reconstructions and 3-D imaging. Abdom Imaging. 2012. [Epub ahead of print].


