| Author | Affiliation |
|---|---|
| Samuel H.F. Lam, MD | Advocate Christ Medical Center, Department of Emergency Medicine, Oak Lawn, Illinois |
DIAGNOSIS
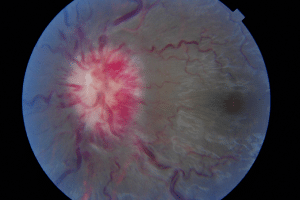
Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri, defined as elevated intracranial pressure with no evident cause found on extensive evaluation. Figures 1 and and22 show bilateral papilledema. Headache is absent in some patients with IIH, especially in the pediatric population.1,2 Abducens nerve palsy is a common finding. Oculomotor palsy (as in our case) and other cranial nerve deficits are rare symptoms.1,3,4 Loss of vision is the major morbidity in IIH. While most cases follow a slow and insidious course, some patients experience rapid development of vision loss within a few weeks of symptom onset. Aggressive surgical treatment is indicated in such fulminant cases, often with temporizing measures in place (e.g. serial lumbar puncture, lumbar drain) until surgery can be performed.5 The patient underwent a lumbar puncture in the ED, with an opening pressure recorded to be over 400 mmH2O. Magnetic resonance image of the brain was unremarkable. She was admitted to the hospital and started on intravenous methylprednisolone and acetazolamide. A lumboperitoneal shunt was eventually placed and she was discharged home. On follow up 1 year later, her vision was noted to be 20/50 in the left eye and 20/20 in the right eye with correction.
Footnotes
Supervising Section Editor: Sean O. Henderson, MD
Submission history: Submitted November 2, 2012; Accepted November 26, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.11.14670
Address for Correspondence: Samuel H.F. Lam, MD, Advocate Christ Medical Center, Department of Emergency Medicine, 4440 West 95th Street. Oak Lawn, IL 60453. Email: emedicine@yahoo.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Rangwala LM, Liu GT. Pediatric idiopathic intracranial hypertension. Surv Ophthal. 2007;52:597–617. [PubMed]
2. Lim M, Kurian M, Penn A, et al. Visual failure without headache in idiopathic intracranial hypertension. Arch Dis Child. 2005;90:206–10. [PMC free article] [PubMed]
3. Tan H. Bilateral oculomotor palsy secondary to pseudotumor cerebri. Pediatr Neuro.2010;42:141–142. [PubMed]
4. Chari C, Rao NS. Benign intracranial hypertension—its unusual manifestations. Headache.1991;31:599–600. [PubMed]
5. Thambisetty M, Levin PJ, Newman NJ, et al. Fulminant idiopathic intracranial hypertension.Neurology. 2007;68:229–232. [PubMed]