| Author | Affiliation |
|---|---|
| Bryce C. Pulliam, MD | University of California Davis Medical Center, Department of Emergency Medicine, Sacramento, California |
| Mark Y. Liao, BA | University of California Davis Medical Center, School of Medicine, Sacramento, California |
| Theodore M. Geissler, BS | University of California Davis Medical Center, School of Medicine, Sacramento, California |
| John R. Richards, MD | University of California Davis Medical Center, Department of Emergency Medicine, Sacramento, California |
ABSTRACT
Introduction:
The boarding of admitted patients in the emergency department (ED) is a major cause of crowding and access block. One solution is boarding admitted patients in inpatient ward (W) hallways. This study queried and compared ED and W nurses’ opinions toward ED and W boarding. It also assessed their preferred boarding location if they were patients.
Methods:
A survey administered to a convenience sample of ED and W nurses was performed in a 631-bed academic medical center (30,000 admissions/year) with a 68-bed ED (70,000 visits/ year). We identified nurses as ED or W, and if W, whether they had previously worked in the ED. The nurses were asked if there were any circumstances where admitted patients should be boarded in ED or W hallways. They were also asked their preferred location if they were admitted as a patient. Six clinical scenarios were then presented, and the nurses’ opinions on boarding based on each scenario were queried.
Results:
Ninety nurses completed the survey, with a response rate of 60%; 35 (39%) were current ED nurses (cED), 40 (44%) had previously worked in the ED (pED). For all nurses surveyed 46 (52%) believed admitted patients should board in the ED. Overall, 52 (58%) were opposed to W boarding, with 20% of cED versus 83% of current W (cW) nurses (P < 0.0001), and 28% of pED versus 85% of nurses never having worked in the ED (nED) were opposed (P < 0.001). If admitted as patients themselves, 43 (54%) of all nurses preferred W boarding, with 82% of cED versus 33% of cW nurses (P < 0.0001) and 74% of pED versus 34% nED nurses (P = 0.0007). The most commonly cited reasons for opposition to hallway boarding were lack of monitoring and patient privacy. For the 6 clinical scenarios, significant differences in opinion regarding W boarding existed in all but 2 cases: a patient with stable chronic obstructive pulmonary disease but requiring oxygen, and an intubated, unstable sepsis patient.
Conclusion:
Inpatient nurses and those who have never worked in the ED are more opposed to inpatient boarding than ED nurses and nurses who have worked previously in the ED. Primary nursing concerns about boarding are lack of monitoring and privacy in hallway beds. Nurses admitted as patients seemed to prefer not being boarded where they work. ED and inpatient nurses seemed to agree that unstable or potentially unstable patients should remain in the ED but disagreed on where more stable patients should board.
INTRODUCTION
Emergency department (ED) crowding, or access block, is a nationwide problem, with 90% of hospitals in the United States reporting it as a major problem.1,2 It is associated with poor patient outcomes, medication errors, delays in treatment, increased morbidity and deaths.3–7 It is also associated with decreased patient satisfaction, and higher rates of patients leaving against medical advice (AMA) and left without being seen (LWBS).8,9 Overall length of stay and boarding time for admitted patients increases during these periods of crowding.10 Many emergency physicians report excessive boarding times for intensive care unit (ICU) patients and those with specific room requirements (telemetry monitoring, isolation, etc.).11
The major component of ED crowding is admitted patients awaiting an inpatient ward (W) bed.12 One solution is the boarding of admitted patients in W hallways.13 While patients seem to prefer W boarding based on prior reports, no study of nurses’ opinions has been yet published.14–18 We undertook this survey study of ED and W nurses to determine and compare their opinions on this controversial topic. We were primarily interested if there was a difference in ED versus W nurse preference for W boarding of admitted patients. Our secondary objective was to assess where nurses would prefer to be boarded if they were patients, and finally to present them with clinical scenarios to assess whether special nursing requirements impacted the appropriateness of boarding in a given location.
METHODS
Study Design
This was a survey study of ED and W nurses. The actual survey was printed on paper and manually distributed, then collected after completion. The survey instrument is shown in the Appendix. Informed consent from participating nurses was not required, and since no patient information was obtained, this study received an exemption from our hospital’s institutional review board.
Study Setting and Population
The study setting was a single 631-bed academic medical center with 30,000 admissions per year and a 68-bed ED with 70,000 patient visits per year. This hospital is a Level 1 trauma center and tertiary care facility serving an urban community of approximately 2 million. Potential nurse study participants were approached both in the ED and W and asked to participate in the voluntary survey. Inclusion criteria were nurses currently working in the ED or adult W. Excluded were nurses working in the ICU, or pediatric W.
Study Protocol
The authors distributed and collected surveys at random times during the month of November 2011. A convenience sample of nurses were identified as ED or W, and if W, whether they had previously worked in the ED. They were asked whether there were circumstances where admitted patients waiting for a bed could be boarded in the ED or W hallways. Nurses opposed to boarding in the ED or W were queried as to their reasons why. They were also asked where they would prefer to be boarded if they were a patient. Six specific patient scenarios were then presented, and subjects were queried where they believed these patients should board. These scenarios included 1) a 55-year-old woman admitted for elective cholecystectomy (vital signs and medications every 6 hours), 2) a 55-year-old male admitted for syncope (vital signs every 4 hours and on continuous telemetry), 3) a 65-year-old male admitted for vomiting and dehydration (vitals every 2 hours and continuous intravenous fluids), 4) a 65-year-old female admitted for chronic obstructive pulmonary disease (COPD) exacerbation (vitals and nebulizers every 2 hours, continuous 3L/minute oxygen requirement), 5) an 85-year-old male admitted for altered mental status, hypoxia, hypotension (intubated and on pressors), 6) a mass casualty incident (MCI) involving 100 patients en route and 15 patients currently boarding in the ED. Nurses were asked whether the patient(s) in each scenario should be boarded in the ED hallway, W hallway, either, or should remain in a designated ED treatment bed. For the final MCI scenario, remaining in a designated ED treatment bed was not an option.
Data Analysis
With regard to subgroup analysis, we compared current ED nurses (cED) to current W nurses (cW); Nurses with previous ED experience (pED) were compared to those with no ED experience (nED). We analyzed the results using chi square test, and statistical significance is assumed at P ≤ 0.05.
RESULTS
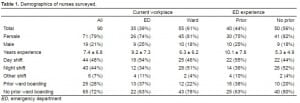
The survey was completed by 90 nurses after a total of 150 surveys were distributed randomly. With regard to demographics and experience, 71 (79%) were female and 44 (49%) identified themselves as primarily day shift nurses. Sixty-five (72%) had never worked at a hospital with a policy for W boarding. Thirty-five (39%) were cED nurses, and 40 (44%) were pED, which may have included ED experience during nursing school. As a group they had a combined average of 7 years’ experience, with cED nurses having 9 years’ experience and cW nurses having 6 years’ experience (Table 1).
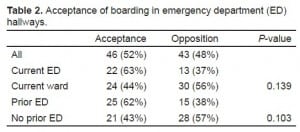
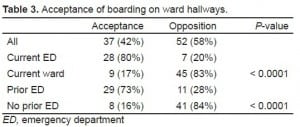
Overall, 46 (52%) approved of boarding admitted patients in the ED. Subgroup analysis (Table 2) revealed 63% of cED nurses approved of ED boarding, whereas only 44% of cW nurses accepted this practice but was not statistically significant (P = 0.139). For those nurses opposed to ED boarding, the most common reason given was the lack of monitoring (86%), lack of privacy (81%), concerns for patient safety (79%), patient comfort (74%), fire hazard (70%), lack of appropriate staffing (67%) and other concerns (14%). Overall, 52 (58%) were opposed to W boarding (Table 3), with 20% of cED versus 83% of cW nurses (P < 0.0001), and 28% of pED versus 84% nED nurses opposed (P < 0.001). For those nurses opposed to W boarding, the most common reason given was the lack of monitoring (87%), lack of privacy (85%), concerns for patient comfort (83%), patient safety (81%), fire hazard (71%), lack of appropriate staffing (71%) and other concerns (14%). If admitted as patients themselves (Table 4), overall 43 (54%) preferred W boarding, with 82% of cED versus 33% of cW nurses (P < 0.0001) and 74% of pED versus 34% nED nurses (P = 0.0007).
Acceptance of boarding in emergency department (ED) hallways.
Acceptance of boarding on ward hallways.
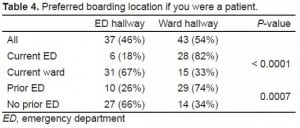
Preferred boarding location if you were a patient.
For the 6 clinical scenarios, statistically significant differences in opinion regarding inpatient boarding existed in all but 2 cases (Table 5): the patient with COPD requiring continuous oxygen and frequent nebulizers, and the intubated sepsis patient on pressors. With regards to the MCI scenario, overall 42% believed patients should be moved to W hallways, 25% condoned ED hallways, and 33% felt either location was acceptable. Among cED nurses 62% believed admitted patients should be moved to W hallways, while only 29% of cW nurses felt this way, while 37% of cW versus 6% of cED nurses felt they should be placed in the ED hallways (P = 0.001). This difference in opinion was also detected for pED and nED nurses (P = 0.04)
DISCUSSION
To our knowledge, this is the only study to date specifically addressing nursing perspectives on ED and W boarding of admitted patients. In a study of perception of compromised care during ED crowding, Pines14 and associates surveyed patients, physicians, and nurses and found that nurses identified waiting room time, number of patients in the waiting room, and number of admitted patients waiting for inpatient beds as factors involved in compromised care.14 Obtaining nursing input is important, as they are most directly impacted by policy changes in the location of admitted patients. Furthermore, the possibility of resistance to the practice of inpatient boarding by W nurses needs to be further explored. Korn and colleages developed an assessment tool to monitor ED nurse workload that took into account care of boarded patients.19 They concluded that the addition of caring for ED boarders, especially those waiting for ICU and telemetry beds, frequently created an “overload” situation for ED nurses and compromised care of incoming acute patients.
In several prior survey studies, admitted patients given a preference of location prefer boarding in W hallways, as opposed to ED hallways if no inpatient rooms are available.15–18 Many of the reasons cited by patients preferring W boarding concerned privacy, noise, and comfort issues. Viccellio and co-workers at Stony Brook University Hospital successfully implemented W boarding and reported a lower mortality rate for boarded hallway patients compared to those admitted to standard W beds over a 4-year period.13 In the aforementioned study patients appropriate for inpatient boarding were selected by emergency physicians with the following exclusion criteria: ICU/step-down unit criteria, chest pain with abnormal troponin, need for suction or high flow oxygen, admissions for seizure, diarrhea, neutropenia, high risk of eloping, and respiratory or other isolation. In addition to improving patient satisfaction and safety, inpatient hallway boarding may also significantly impact ED crowding and left without being seen (LWBS) rates, as well as be financially attractive with regard to hospital revenue.20,21
While the hypothesis that working in the ED would be associated with greater acceptance of W boarding was confirmed by our data, the high level acceptance of ED boarding (62%) among ED nurses was surprising, although it did not reach statistical significance. In both ED and W settings, nurses’ primary concerns about boarding were lack of monitoring and lack of privacy. The preference among ED nurses for W boarding, and W nurses for ED boarding when they are patients may suggest that nurses prefer not to board where they work. This may be understandable from a privacy aspect. The significant differences between cED/pED and cW/nED nurses as to where the clinically stable patients in scenarios 1–3 should board were expected based on our earlier results. Additionally, there was agreement between these groups for the relatively unstable patients in scenarios 4 and 5. However, there was a significant difference in opinion on where to board admitted patients in the ED in anticipation of receiving victims of a large-scale MCI passenger jet crash. One reason for this dichotomy is that W nurses may expect to be called to the ED to help in the care of these incoming patients and would not be able to care for patients boarded in W hallways. There also may be a desire for W nurses who rarely visit or are unfamiliar with the ED to “keep everything in the ED” for focused care without realizing the actual space limitation.
LIMITATIONS
While this study highlights the difference in attitudes towards boarding by ED and W nurses, it also has several limitations. There was a small sample size, and it was performed at a single academic center limiting its generalizability. Also, the 2 groups surveyed had differences in years of experience: cED nurses had an average of 3 additional years’ experience compared with cW, and pED nurses had nearly twice the experience of nED. It is not clear if this influenced their answers. Furthermore, this survey was administered at a hospital where inpatient boarding is not allowed, and the majority of nurses surveyed had never worked in an institution that implemented inpatient boarding.
CONCLUSION
Inpatient nurses and those who have never worked in the ED are more opposed to inpatient boarding than ED nurses and nurses who have worked previously in the ED. Nurses admitted as patients seemed to prefer not being boarded where they work. ED and inpatient nurses seemed to agree that unstable or potentially unstable patients should remain in the ED, but disagreed on where more stable patients should board. They also disagreed on where admitted patients should board in the case of a mass casualty incident; ED nurses favored inpatient boarding to make space for a large number of incoming trauma victims, whereas inpatient nurses preferred retaining admitted patients in the ED.
Appendix
Many hospitals are implementing policies where admitted patients are boarded in ward hallways if the ED is overcrowded and there are no floor beds immediately available. This survey is designed to determine your opinion about this practice. Your honest answers are appreciated. Unless otherwise specified, please mark the one choice that you feel best answers the question. Your responses are anonymous. Thank you for agreeing to take this brief survey.
- What is your gender?
- _ Male
- _ Female
- How many years of nursing experience do you have?______________
- What type of floor/department do you primarily work on (ex: med/surg, heme/onc, cardiology, trauma, ICU, emergency department (ED), etc.)?_________________________________________________________________
- At some point in your career, have you worked in an ED?
- _ Yes
- _ No
- Which of the following best describes the majority of your shifts?
- _ Day shifts
- _ Night shifts
- _ Other (please explain_______________________)
- Have you ever worked in a hospital where admitted patient were boarded in ward hallways if no beds were available?
- _ Yes
- _ No
- Are there any circumstances where admitted patients should be boarded in the ED hallway while waiting for a bed on the floor?
- _ Yes
- _ No
- _ Maybe (Why?_______________________________________________________)
- If you checked “No” to question 7, what are the reasons for your decision? (check all that apply)
- _ Adverse effect on patient safety
- _ Lack of sufficient nursing staff (It would be prohibited by nursing ratios)
- _ Lack of monitoring
- _ Adverse effects on patient comfort
- _ Adverse effects on patient privacy
- _ Fire hazard
- _ Other (please list) _____________________________________________________
- Are there any circumstances where admitted patients should be boarded in ward hallways while waiting for a bed on the floor?
- _ Yes
- _ No
- _ Maybe (Why? _________________________________________________________)
- If you checked “No” to question 9, what are the reasons for your decision? (check all that apply)
- _ Adverse effect on patient safety
- _ Lack of sufficient nursing staff (It would be prohibited by nursing ratios)
- _ Lack of monitoring
- _ Adverse effects on patient comfort
- _ Adverse effects on patient privacy
- _ Fire hazard
- _ Other (please list) _____________________________________________________
- If you were a patient in the ED who was being admitted, but no beds were available, where would you prefer to be boarded?
- _ In the ED hallway
- _ In the ward hallway
Please read the following patient scenarios and state whether you think the patient is appropriate to board in the location listed assuming there are sufficient nurses to board this patient and maintain appropriate nursing ratios. Every gurney in the ED is occupied and the waiting room is full. There are no available beds upstairs, but these patients have admission orders from the admitting team.
Scenario 1: 55-year old female presenting to the ED with 6 months of crampy right upper quadrant pain which is worse with meals. In the ED she was found to have gallstones, but normal labs and stable vitals throughout her ED stay. Surgery was consulted and has admitted the patient for elective cholecystectomy. She has admission orders for q6 hour vitals, is NPO, and is only requiring pain medications Q6 hours. She does not require telemetry or supplemental oxygen.
Where should the patient be boarded?
- _ In the ED hallway
- _ In the Ward hallway
- _ Either location would be appropriate
- _ This patient is not an appropriate candidate for boarding and should remain in an ED treatment room until a Ward bed becomes available.
Scenario 2: 55-year old male with history of kidney stones, presenting to the ED after he passed out in church. He has no prior history of syncope and has never had a syncope workup. In the ED he has stable vitals and does not have any chest pain, shortness of breath, headache or neurologic symptoms. His CT head is negative for any bleeding or fractures. He is admitted for a syncope workup. He has admission orders for Q4 hour vitals, regular diet and continuous telemetry monitoring. He does not require supplemental oxygen.
Where should the patient be boarded?
- _ In the ED hallway
- _ In the Ward hallway
- _ Either location would be appropriate
- _ This patient is not an appropriate candidate for boarding and should remain in an ED treatment room until a Ward bed becomes available.
Scenario 3: 65-year old male with history of hypertension and high cholesterol, presenting to the ED with dehydration after 3 days of recurrent vomiting. In the ED he was found to have dry mucous membranes, but a normal BP. He initially had tachycardia which resolved with 1L IV fluids. He has acute renal failure and is admitted for rehydration and observation. He has admission orders for Q2 hour vitals, regular diet and requires continuous IV fluids. He does not require telemetry or supplemental oxygen.
Where should the patient be boarded?
- _ In the ED hallway
- _ In the Ward hallway
- _ Either location would be appropriate
- _ This patient is not an appropriate candidate for boarding and should remain in an ED treatment room until a Ward bed becomes available.
Scenario 4: 65-year old female with history of poorly controlled COPD and hypertension presenting to the ED with shortness of breath and wheezing. In the ED she was found to have wheezes in both lung fields, which have improved with repeated rounds of nebulizers. Currently, she has stable respiratory rate, but continues to have some wheezes on exam. She is admitted for COPD exacerbation for ongoing nebulizer treatments. She has admission orders for Q2 hour vitals and is written for Q4 hour nebulizers, with Q2 hour nebulizers written PRN wheezing. She requires 3L/hour supplemental oxygen via nasal canula.
Where should the patient be boarded?
- _ In the ED hallway
- _ In the Ward hallway
- _ Either location would be appropriate
- _ This patient is not an appropriate candidate for boarding and should remain in an ED treatment room until a Ward bed becomes available.
Scenario 5: 85yo male with history of COPD and CAD presenting to the ED with altered mental status following 1week of fever, chills, and difficulty breathing. He was intubated for hypoxia and airway protection upon arrival to the ED and was briefly hypotensive with systolic BPs in the 70s. He is still intubated and sedated and requiring pressors to maintain his BP.
Where should the patient be boarded?
- _ In the ED hallway
- _ In the Ward hallway
- _ Either location would be appropriate
- _ This patient is not an appropriate candidate for boarding and should remain in an ED treatment room until a Ward bed becomes available.
Scenario 6: A large jet arriving from the East Coast crashes while landing at the airport. It was carrying 238 passengers, many were dead on scene, but initial reports have from 100–200 patients requiring transport and treatment at local hospitals. Many of these patients have critical injuries such as multiple fractures, head injuries, burns and severe smoke inhalation. The first ambulances are expected at the ED within 20 minutes. There are currently 15 patients in the ED who have ward admission orders, but are waiting for a bed upstairs. In order to make room for the incoming mass casualties, these patients MUST be moved from their ED beds immediately.
Where should the patients be boarded?
- _ In the Emergency Department hallway
- _ In the ward hallway
- _ Either location would be appropriate
Footnotes
Supervising Section Editor: Erik D. Barton, MD, MBA
Submission history: Submitted June 20, 2012; Revision received October 30, 2012; Accepted December 11, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.12.12830
Address for Correspondence: John R. Richards, MD, Department of Emergency Medicine, U.C. Davis Medical Center, PSSB 2100, 4150 V Street, Sacramento, CA 95817. Email: jrrichards@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Derlet RW, Richards JR. Overcrowding in the nation’s emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35:63–68. [PubMed]
2. Derlet R, Richards J, Kravitz R. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med. 2001;8:151–155. [PubMed]
3. Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010;28:304–309. [PubMed]
4. Bernstein SL, Aronsky D, Duseja R, et al. Society for Academic Emergency Medicine, Emergency Department Crowding Task Force. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. [PubMed]
5. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–216. [PubMed]
6. Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust.2006;184:208–212. [PubMed]
7. McCarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009;54:492–503.[PubMed]
8. Richardson DB, Mountain D. Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust. 2009;190:369–374. [PubMed]
9. Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med. 2008;15:825–831. [PubMed]
10. Twanmoh JR, Cunningham GP. When overcrowding paralyzes an emergency department. Manag Care. 2006;15:54–59. [PubMed]
11. Richards JR, Navarro ML, Derlet RW. Survey of directors of emergency departments in California on overcrowding. West J Med. 2000;172:385–388. [PMC free article] [PubMed]
12. Derlet RW, Richards JR. Ten solutions for emergency department crowding. West J Emerg Med.2008;9:24–27. [PMC free article] [PubMed]
13. Viccellio A, Santora C, Singer AJ, et al. The association between transfer of emergency department boarders to inpatient hallways and mortality: a 4-year experience. Ann Emerg Med.2009;54:487–491. [PubMed]
14. Pines JM, Garson C, Baxt WG, et al. ED crowding is associated with variable perceptions of care compromise. Acad Emerg Med. 2007;14:1176–1181. [PubMed]
15. Garson C, Hollander JE, Rhodes KV, et al. Emergency department patient preferences for boarding locations when hospitals are at full capacity. Ann Emerg Med. 2008;51:9–12. [PubMed]
16. Walsh P, Cortez V, Bhakta H. Patients would prefer ward to emergency department boarding while awaiting an inpatient bed. J Emerg Med. 2008;34:221–226. [PubMed]
17. Bartlett S, Fatovich DM. Emergency department patient preferences for waiting for a bed. Emerg Med Australas. 2009;21:25–30. [PubMed]
18. Richards JR, Ozery G, Notash M, et al. Patients prefer boarding in inpatient hallways: correlation with the national emergency department overcrowding score. Emerg Med Int. 2011:1–4.[PMC free article] [PubMed]
19. Korn R, Mansfield M. ED overcrowding: an assessment tool to monitor ED registered nurse workload that accounts for admitted patients residing in the emergency department. J Emerg Nurs.2008;34:441–446. [PubMed]
20. Bair AE, Song WT, Chen YC, et al. The impact of inpatient boarding on ED efficiency: a discrete-event simulation study. J Med Syst. 2010;34:919–929. [PMC free article] [PubMed]
21. Pines JM, Batt RJ, Hilton JA, et al. The financial consequences of lost demand and reducing boarding in hospital emergency departments. Ann Emerg Med. 2011;58:331–440. [PubMed]