| Author | Affiliation |
|---|---|
| Scott C. French, MD | Saint Francis Hospital, Department of Emergency Medicine, Evanston, Illinois |
| Shu B. Chan, MD, MS | Resurrection Medical Center, Department of Emergency Medicine, Chicago, Illinois |
| Jill Ramaker, RN, MSc, MA | North Shore University Health System, Highland Park Hospital, Highland Park, Illinois |
ABSTRACT
Introduction:
The most common reason patients seek medical attention is pain. However, there may be significant delays in initiating prehospital pain therapy. In a 2001 quality improvement (QI) study, we demonstrated improvement in paramedic knowledge, perceptions, and management of pain. This follow-up study examines the impact of this QI program, repeated educational intervention (EI), and effectiveness of a new pain management standard operating procedure.
Methods:
176 paramedics from 10 urban and suburban fire departments and two private ambulance services participated in a 3-hour EI. A survey was performed prior to the EI and repeated one month after the EI. We reviewed emergency medical services (EMS) runs with pain complaints prior to the EI and one month after the EI. Follow-up results were compared to our prior study. We performed data analysis using descriptive statistics and chi-square tests.
Results:
The authors reviewed 352 surveys and 438 EMS runs with pain complaints. Using the same survey questions, even before the EI, 2007 paramedics demonstrated significant improvement in the knowledge (18.2%; 95% CI 8.9%, 27.9%), perceptions (9.2%; 95% CI 6.5%, 11.9%), and management of pain (13.8%; 95% CI 11.3%, 16.2%) compared to 2001. Following EI in 2007, there were no significant improvements in the baseline knowledge (0%; 95% CI 5.3%, 5.3%) but significant improvements in the perceptions of pain principles (6.4%; 95% CI 3.9%, 9.0%) and the management of pain (14.7%; 95% CI 11.4%, 18.0%).
Conclusion:
In this follow up study, paramedics’ baseline knowledge, perceptions, and management of pain have all improved from 6 years ago. Following a repeat educational intervention, paramedics further improved their field management of pain suggesting paramedics will still benefit from both initial and also ongoing continuing education on the topic of pain management.
INTRODUCTION
The most common reason patients seek medical attention is because they are experiencing pain.1–11Despite a chief complaint of pain, there may be significant delays in the emergency department (ED) until initiating pain therapy.12,13 These delays include time to triage and patient assessments, followed by ordering, obtaining, and administration of the medication. As a result, the initial assessment and management of pain must begin in the prehospital setting.12,13 Knowledge of pain principles, assessment, documentation, and management, both pharmacologic and non-pharmacologic, of pain must be included in both initial and ongoing paramedic educational programs. The institution of quality improvement (QI) programs will serve to assess the effectiveness of prehospital providers’ practices.14
In 2003, the National Association of Emergency Medical Services (EMS) Physicians produced a position paper solely for prehospital pain management, stating that every EMS system must be dedicated to the assessment and treatment of pain. To be effective, a comprehensive program must be instituted, which includes education, assessment, documentation, intervention, and QI. This program must be in place in conjunction with a prehospital standard operating procedure (SOP).15
In 2001, this EMS system instituted a QI project to assess pain management in the prehospital setting and to evaluate the perception of pain principles and knowledge of pain management. Through our regularly scheduled continuing education (CE) sessions we instituted an education intervention (EI) focused on all aspects of pain. As a result of the EI, paramedics had an increased understanding of pain (17.5% P < 0.001), improved perceptions of pain principles (4.2% P < 0.003) and improved field management of pain (21% P < 0.001). More specifically, paramedics were more likely to provide prehospital non-pharmacologic pain therapy (32.2% improvement P < 0.001), and were more likely to document the results of their interventions (repeat vs 14.7% P < 0.001, repeat pain score 11.3% P< 0.001, pain reassessment 13% P < 0.001, pain reassessment on ED arrival 15.4% P < 0.001). From this study we approved the addition of a pain management SOP, giving paramedics the authority to manage pain without requiring permission from medical control via telemetry.16
As a follow-up to this study, we reassessed the paramedics in our EMS system to measure the long term impact of the EI, to determine if a repeat EI was necessary, and to determine if the new pain management SOP was effective.
METHODS
Study Design
This prospective study assessed the effects of an EI on change in the knowledge base of pain assessment, documentation, and treatment of pain in the prehospital setting. We then compared the results found in this identically designed follow-up study to the original results.
Study Setting and Population
This study included emergency medical technician-paramedic (paramedic) providers from 10 fire departments and 2 private ambulance services, including both volunteer and non-volunteer organizations. The study took place in an EMS system that included both urban and suburban populations. Approximately 800 paramedics participate in the EMS system with a 95% Advanced Life Support (ALS) response. Average transport times for the system are 8 minutes with a maximum of 30 minutes, dependent mostly on traffic patterns in this urban to suburban region.
Study Protocol
This EMS system instituted the same QI protocol as performed in 2001 to evaluate the knowledge and perception of pain management by EMS providers and to assess pain management in the prehospital environment.16 All paramedics who were present for the regularly scheduled 3-hour CE session were chosen to participate in the EI. The students were blinded to the study. The CE sessions were taught using the same material for PowerPoint presentation with discussion. Nine nurse coordinators who regularly give monthly CE sessions participated in the study. Prior to the CE sessions, the nurses met to review the PowerPoint presentation and discuss the material to standardize the presentation. All nurse coordinators are Illinois emergency communications registered nurse (ECRN) certified. Two also had current Illinois paramedic licenses during the study. Additionally, those paramedics who were present during the 2001 EI were also identified via the questionnaire. All were given 15 minutes to complete an individual demographic survey. All paramedics present for the EI completed and turned in the questionnaire (100%). Some paramedics placed their names on the survey but, for the purpose of the study, anonymity was maintained. A 3-hour EI was then implemented by the nurse educators. Every survey question topic was discussed during the EI session without notifying the paramedics that it was a survey question. A second evaluation was conducted the following month. Paramedics again completed the same questionnaire. Paramedics who did not complete the first questionnaire did not complete the second questionnaire. Following the second evaluation, the same paramedic medical officers performed a repeated 2-month review of run reports for all patients with a complaint of pain.
Paramedic medical officers are appointed a supervisory role within their organizations to maintain paramedic records, assist with education, review competencies, and establish policies and procedures. A paramedic medical officer participated from each organization. All of the paramedic medical officers were given an in-service on the importance of quality improvement projects and EMS research. We educated the paramedic medical officers in the use of the data collection forms. Three of the 12 medical officers participated in the initial EI in 2001. As part of their daily activities, the paramedic medical officers have training and experience in reviewing run reports. The run reports are patient care reports containing demographic data with history, physical exam, and treatment documentation. There was no change in the run report format since 2001.
Approval was obtained for this study from the Institutional Review Board. Communications to medical control via telemetry radio were received by either a physician or a nurse. Morphine sulfate (MS) was the only pharmacologic agent incorporated into the pain management SOP during this study. Paramedics could give MS 2 mg IV every 5 minutes to a maximum dose of 10 mg without obtaining approval from medical control for patients with any complaint of pain except for abdominal pain. These patients must also have a normal mental status and a systolic BP > 100 mmHg. Paramedics could also use non-pharmacologic methods to treat pain such as ice, splinting, repositioning, and communicative support.
Measurements
The paramedic surveys contained the same questions as the initial EI regarding their perceptions and knowledge of basic pain management principles except for the last question asking about their comfort level using the new pain management SOP. During this follow-up study, the initial and repeated EMS run reviews collected data regarding documentation, assessment and prehospital pain therapy given. The 9 characteristics of pain assessment reviewed were pain location, radiation, quality, onset, type, relieving factors, provoking factors, pain timing, and sleep disturbances. We analyzed the percentages of each of these 9 characteristics documeted before and after the EI. Paramedic and patient demographic information was also collected.
Data Analysis
Descriptive statistics were used to compare findings before and after EI and between 2001 and 2007. Differences were reported with 95% confidence intervals (CIs) along with P-values from z tests of 2 proportions. All P-values were two-tailed. Statistical calculations were performed using Minitab version 12.1 (Minitab Inc., State College, Pennsylvania).
RESULTS
There were 176 paramedics involved in the study. The population was 95% male, with a mean age of 38.7 years (range: 20–65) and 11.6 years of paramedic experience (range: 1–31). More than half (54%) of the paramedics received education beyond high school with 16% receiving associate’s degrees, 32% having bachelor’s degrees and 4% receiving master’s degrees. Twenty-six percent of the paramedics attended paramedic school in 2001 or later. On average, the paramedics reported receiving 4.6 education hours on pain, although 26% did not respond to this question. Only 21% of the paramedics stated that they had received the same EI in 2001, although 31% stated that they did not recall if they did or not. Paramedics completed 176 questionnaires before and after the intervention. This study also reviewed 283 EMS runs before the intervention and 155 after the intervention, for a total of 438 runs.
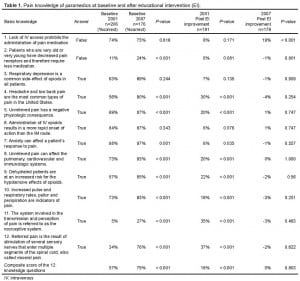
The basic knowledge of the paramedics regarding pain management is shown in Table 1 and Figure 1. There was a significant improvement between the baseline knowledge of the paramedics in 2001 and the baseline knowledge in 2007 (18.2; 95% CI 8.97%, 27.9%). However, in 2001 there were significant improvements of knowledge following the educational intervention, while in 2007 there were hardly any improvements. It is interesting that on the question of IV access, there was much more improvement in 2007 than 2001, even though the baseline scores were the same.
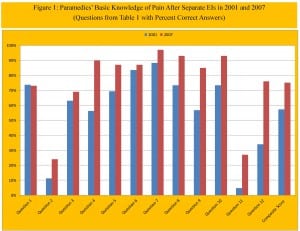
Paramedics’ basic knowledge of pain after separate educational interventions in 2001 and 2007 (questions from Table 1 with percent correct answers).
Paramedics were also asked about their perceptions of pain in transported patients. Details of their perceptions are shown in Table 2. In 2007 there were significantly fewer paramedics with incorrect perceptions of pain management. For example, in 2001 57% felt that EMS had a restricted role in pain relief, while in 2007 only 5% had this belief. However, perhaps because of these improved perceptions, there were hardly any significant changes following education in 2007. The one exception concerns patients’ unique perceptions of pain. Following education in 2007, many fewer paramedics felt that past experience or culture influenced pain perception, suggesting less cultural bias in 2007.
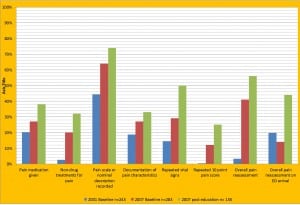
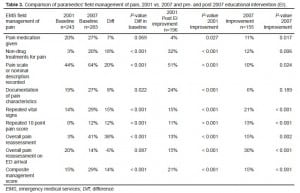
The effects of the EI on prehospital pain management practice by the paramedics are shown in Table 3 and Figure 2. As compared to 2001, in 2007, there were significant improvements in the baseline field management of pain prior to the EI. However, as opposed to the results on knowledge or perceptions, in 2007 there was almost as much further significant improvement following education as occurred in 2001.
DISCUSSION
Following our last study, we instituted a pain management SOP in our entire region made up of 4 EMS systems. Our goal in this study was to determine if the EI and pain management SOP had long-term effects for paramedics. We also wanted to collect data to determine if a regular EI was helpful to maintain baseline skills regarding pain management. Given that pain is the most common chief complaint of our patients, it must be assessed and managed adequately especially given the delays to treatment that take place on presentation to the ED. 12,13 In this follow-up study, when we reviewed the paramedics’ run reports, we again saw significant improvements in baseline documentation and management of pain prior to the EI. There was, however, also significant improvement in prehospital documentation and management of pain following the EI in 2007.
Prior to the EI, in 2007 there were significant improvements in 9 of the 12 baseline knowledge questions. While in 2001 we saw significant improvements in knowledge following the EI, we did not see that in 2007. It is possible that because their baseline knowledge was already so high in 2007, there was little room for improvement. Additionally, the curriculum of current paramedic programs includes more material on the topic of pain. Twenty-six percent of the paramedics in this study may have had a better baseline knowledge base since they attended paramedic school in 2001 or later. With 1 question pertaining to the topic of IV access, we saw significant improvement following the EI.
Our results regarding paramedics’ perceptions followed a similar trend. There were significant improvements in 3 of the 12 baseline perceptions questions. While in 2001 we saw significant improvements in perceptions following the EI, we did not see that in 2007, again likely because they already had good perceptions of pain management. More commonly in 2007 paramedics understand the importance of applying pain management principles. Again, there was one question with a significant improvement following the EI on the topic of past or cultural experiences with pain. Cultural backgrounds can affect a person’s response to pain.15,17 while those same cultural biases can affect a prehospital provider’s management of pain.18,19
Given the noted findings regarding paramedic knowledge and perceptions of pain, we were surprised to identify a different trend in regards to the field management of pain. In addition to there being significant improvements in the baseline field management of pain, there were also further significant improvements following the EI in 2007. Paramedics not only improved their baseline field management of pain but we discovered through this study that further continuing education is effective.
The pain management SOP allows for the administration of MS. Since the institution of the pain management SOP we expected to see a significantly higher administration rate of MS. We did not see that 20% gave pain medication in 2001 prior to the MS protocol, while 27% (P = 0.069) gave pain medication in 2007 after the MS protocol. In a similar study where paramedics were allowed to administer MS according to written protocols, a higher percentage of patients were also not given MS after the protocol was implemented.20 We, however, did see significant increases in the application of non-pharmacologic treatments for pain. These included the use of ice, splinting, repositioning, and communicative support to relieve pain. We believe that because of a more comprehensive understanding of pain management, the paramedics were able to obtain pain relief without the administration of a narcotic pain medication.
As demonstrated in this study, paramedics retained baseline knowledge, perceptions, and field management of pain. We also learned that we can further improve the prehospital management of pain by incorporating this topic into a QI project. This study demonstrates that a fully comprehensive CE program is still warranted to improve prehospital management of pain. It is unique in that we obtained this understanding through the diligent work of the paramedic medical officers who reviewed every completed run report pertaining to transported patients with pain during a 2-month timeframe before and after the EI. It is also the first follow-up study of its kind to evaluate the long-term effects of an EI focusing on the knowledge, perceptions, and documentation of pain in conjunction with the institution of a pain management SOP.
LIMITATIONS
We reviewed a large number of run reports within one large EMS system located in one geographic region. Expanding this study to the region made up of 4 EMS systems or expanding it statewide would help to reduce potential selection bias. We also reviewed a small number of run reports relative to a large number of paramedics in the system, which may not fully represent the EMS system. Since we retrospectively reviewed run reports and not actual paramedic practice, the same number of non-pharmacologic procedures may have been performed but better documented. The retrospective nature of the chart review also made it challenging to elucidate the specific factors that may have led to the changes in knowledge, perceptions, or documentation.
With the institution of the pain management SOP we studied the number of patients who received any dose of MS. We expected to see a higher number of patients receiving MS. While we did not see an increase in the number of patients receiving MS, we did not study the dose of MS that was given. As a result, the same number of patients may have received MS, but those same patients may have received a higher dose of MS to achieve more effective pain control.
CONCLUSION
In this follow-up study, paramedics’ baseline knowledge, perceptions, and management of pain have all improved from 6 years ago. Following a repeat educational intervention, paramedics further improved their field management of pain suggesting paramedics will still benefit from both initial and also ongoing continuing education on the topic of pain management.
Footnotes
Supervising Section Editor: Christoper A. Kahn, MD, MPH
Submission history: Submitted Novermber 29, 2010; Revision received Novermber 1, 2011; Accepted July 16, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.7.6678
Address for Correspondence: Scott C. French, MD. Resurrection Medical Center, Department of Emergency Medicine, 7435 West Talcott Avenue, Chicago, IL, 60631. Email: sfrench@infinityhealthcare.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Vergnion M, Degesves S, Garcet L, et al. Tramadol, an alternative to morphine for treating posttraumatic pain in the prehospital situation. Anesth Analg. 2001;92(6):1543–1546. [PubMed]
2. Diop D, Aghababian RV. Definition, classification, and pathophysiology of acute coronary ischemic syndromes. Emerg Med Clin North Am. 2001;19(2):259–267. [PubMed]
3. Knight S, Vernon DD, Fines RJ, Dean NP. Prehospital emergency care for children at school and nonschool locations. Pediatrics. 1999;103(6):e81. [PubMed]
4. Bold SP, Luedtke G. Time is muscle. The Cape Cod Chest Pain Task Force helps shorten AMI discovery-to-treatment times. J Emerg Med Serv. 2001;26(4):52–55. [PubMed]
5. Grzybowski M, Zalenski RJ, Ross MA, et al. A prediction model for prehospital triage of patients with suspected cardiac ischemia. J Electrocardiol. 2000;33(Suppl):253–258. [PubMed]
6. White LJ, Cooper JD, Chambers RM, et al. Prehospital use of analgesia for suspected extremity fractures. Prehosp Emerg Care. 2000;4(3):205–208. [PubMed]
7. Carr E. Myths and fears about pain-relieving drugs. Nurs Times. 1997;93(40):50–51. [PubMed]
8. de Rond ME, de Wit R, van Dam FS, Muller MJ. A pain monitoring program for nurses: effects on communication, assessment and documentation of patients’ pain. J Pain Symptom Manage.2000;20(6):424–439. [PubMed]
9. Paris PM, Stewart RD. Pain Management in Emergency Medicine. West Hartford, CT: Appleton & Lange; 1987. Preface.
10. Cordell WH. Pain Research Opportunities and Future Direction. Ann Emerg Med. 1996;27:474–478. [PubMed]
11. Cordell WH, Keene KK, Giles BK, et al. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20(3):165–169. [PubMed]
12. Vassiliadis J, Hitos K, Hill CT. Factors influencing prehospital and emergency department analgesia administration to patients with femoral neck fractures. Emerg Med. 2002;14(3):261–266.(Fremantle) [PubMed]
13. McEachin CC, McDermott JT, Swor R. Few emergency medical services patients with lower-extremity fractures receive prehospital analgesia. Prehosp Emerg Care. 2002;6(4):406–410.[PubMed]
14. McManus JG, Jr, Sallee DR., Jr Pain management in the prehospital environment. Emerg Med Clin North Am. 2005;23(2):415–431. [PubMed]
15. Alonso-Serra HM, Wesley K. Prehospital pain management. Prehosp Emerg Care. 2003;7(4):482–488. [PubMed]
16. French SC, Salama NP, Baqai S, et al. Effects of an educational intervention on prehospital pain management. Prehosp Emerg Care. 2006;10(1):71–76. [PubMed]
17. Walker AC, Tan L, George S. Impact of culture on pain management: an Australian nursing perspective. Holist Nurs Pract. 1995;9(2):48–57. [PubMed]
18. Todd KH, Deaton C, D’Adamo AP, et al. Ethnicity and analgesic practice. Ann Emerg Med.2000;35(1):11–16. [PubMed]
19. Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002;20(3):139–143. [PubMed]
20. Fullerton-Gleason L, Crandall C, Sklar DP. Prehospital administration of morphine for isolated extremity injuries: a change in protocol reduces time to medication. Prehosp Emerg Care.2002;6(4):411–416. [PubMed]