| Author | Affiliation |
| Erik S. Anderson, MD | Alameda County Medical Center, Highland Hospital, Department of Emergency Medicine, Oakland, California |
| Evan Hodell, BS | University of California, San Francisco School of Medicine, San Francisco, California |
| Daniel Mantuani, MD | Alameda County Medical Center, Highland Hospital, Department of Emergency Medicine, Oakland, California |
| Jahan Fahimi, MD | Alameda County Medical Center, Highland Hospital, Department of Emergency Medicine, Oakland, California; University of California, San Francisco, Department of Emergency Medicine, San Francisco, California |
| Ingrid Pampalone, PA | Alameda County Medical Center, Highland Hospital, Department of Orthopedics, Oakland, California |
| Arun Nagdev, MD | Alameda County Medical Center, Highland Hospital, Department of Emergency Medicine, Oakland, California; University of California, San Francisco, Department of Emergency Medicine, San Francisco, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Our objective was to assess the efficacy of ultrasound-guided hip injections performed by emergency physicians (EPs) for the treatment of chronic hip pain in an outpatient clinic setting.
Methods
Patients were identified on a referral basis from the orthopedic chronic pain clinic. The patient population was either identified as having osteoarthritis of the hip, osteonecrosis of varying etiologies, post-traumatic osteoarthritis of the hip, or other non-infectious causes of chronic hip pain. Patients had an ultrasound-guided hip injection of 4ml of 0.5% bupivacaine and 1ml of triamcinolone acetate (40mg/1ml). Emergency medicine resident physicians under the supervision of an attending EP performed all injections. Pain scores were collected using a Likert pain scale from patients prior to the procedure, and 10 minutes post procedure and at short-term follow-up of one week and one month. The primary outcome was patient-reported pain score on a Likert pain scale at one week.
Results
We performed a total of 47 ultrasound-guided intra-articular hip injections on 44 subjects who met inclusion criteria. Three subjects received bilateral injections. Follow-up data were available for 42/47 (89.4%) hip injections at one week and 40/47 (85.1%) at one month. The greatest improvement was at 10 minutes after injection with a mean decrease in Likert pain score from pre-injection baseline of 5.57 (95% CI, 4.76-6.39). For the primary outcome at one week, we found a mean decrease in Likert pain score from pre-injection baseline of 3.85 (95% CI, 2.94-4.75). At one month we found a mean decrease in Likert pain score of 1.8 (95% CI, 1.12-2.53). There were no significant adverse outcomes reported.
Conclusion
Under the supervision of an attending EP, junior emergency medicine resident physicians can safely and effectively inject hips for chronic pain relief in an outpatient clinical setting using ultrasound guidance.
INTRODUCTION
Hip pain is a common complaint with a wide variety of etiologies. These range from the benign and chronic, such as osteoarthritis, to the acutely joint-threatening, such as septic arthritis. Chronic hip pain has an estimated prevalence of up to six percent and is a common cause of pain in patients presenting to orthopedic clinics and emergency departments (EDs).1 Joint injections with corticosteroids are first-line recommended therapy by the American College of Rheumatology,2 and the European League Against Rheumatism recommends intra-articular hip injections for flares of chronic hip osteoarthritis.3 A 2007 randomized controlled trial has also demonstrated clear efficacy without any complications.4
Ultrasound (US) guidance for either hip arthrocentesis or hip injections has since been described in the radiology, rheumatology, and orthopedic literature.5-9 Three trials in emergency medicine (EM) literature have shown efficacy of US to aid in diagnosis of hip effusions,10-12 but no EM trials to date have demonstrated US-guided hip injections as efficacious in the treatment of chronic hip pain. US-guided hip injections have been shown to be more safe and efficacious as compared to blind injections.6,7,13 However, these procedures are rarely performed in an ED setting, and many front-line practitioners who encounter patients with hip pain from degenerative diseases of the hip may not have the training to perform the procedure. Frequently the intra-articular corticosteroid hip injections are performed only in specialty clinics, limiting the access for optimal pain control in patients with non-infectious hip pathology. With adequate training and coordinated follow-up, clinicians could facilitate timely pain control (without overreliance on standard opioid and anti-inflammatory therapies) for these patients.
In a prospective cohort pilot study, we aim to analyze the effect of US-guided corticosteroid hip injections on pain scores as performed by EM trainees.
METHODS
Study Design and Setting
This is a prospective pilot study of US-guided intra-articular hip injections performed by EM trainees with bupivacaine and triamcinolone for hip pain due to osteoarthritis, avascular necrosis, and other chronic conditions. Patients were consecutively enrolled from an orthopedic surgery clinic at a busy, urban hospital and trauma center. The Institutional Review Board of Alameda County Medical Center approved this study.
Selection of Participants
Enrollment occurred from September 2012 to February 2013. Adult patients (age>18) were eligible for inclusion if deemed to have chronic hip pain related to osteoarthritis, avascular necrosis, post-traumatic degenerative changes, late sequelae of septic arthritis, or hip dysplasia as determined by the referring orthopedic surgery attending. All patients were consented for the procedure and enrollment into the study. Exclusion criteria were any signs of systemic infection such as fever, recent illnesses in the past two weeks, contraindication or allergy to the injection agents, anti-coagulant therapy other than aspirin, previous hip injection within the last four months, planned total hip arthroplasty in the coming four months, if an interpreter was not available for the consent process, or if the patient was receiving a diagnostic injection as part of a hip or back pain work up. Patients found ineligible for the study or who declined study enrollment still had the opportunity to receive a hip injection.
Interventions
All patients received the study injection solution of 4ml of 0.5% bupivacaine and 1ml of triamcinolone (40mg). The dosing and medication selection for analgesia and steroid injection were selected based on prior research on fluoroscopically-guided hip injections.4 An EM attending physician, fellowship trained in emergency US, supervised all procedures. First and second-year EM resident physicians performed all procedures after receiving an instructional handout and a standardized five-minute bedside training session. All trainees had completed a one-month US rotation that included instruction on needle-guided procedures, such as US-guided central lines, peripheral venous access, and nerve blocks. They also received a five-minute bedside tutorial on the anatomy of the femoral neck and anterior synovial recess. Trainees had also completed a one-month orthopedics rotation during which they performed landmark-based knee and shoulder injections as part of their clinical rotation. None of the residents had performed hip injections prior to this study, and each resident performed 1-2 injections during the clinic. An ultrasound fellowship-trained EM attending physician supervised all procedures.
Procedure
An ultrasound system (Sonosite M-Turbo; Bothell, WA) with a low frequency curvilinear probe (2-5MHz) was used to identify the hip joint. Local anesthesia over the injection site was applied using ethyl chloride spray. Using standard sterile procedure and local analgesia, a 10cc syringe filled with a 5cc mix of bupivacaine and 40mg of triamcinolone attached to a 20g 3.5 inch spinal needle was guided into the joint space with real-time in-plane ultrasound guidance (Figure 1) (Video). This solution was then injected after ultrasonographic confirmation that the needle tip was in the joint space (Figure 2). Patients were observed for a period of twenty minutes after the procedure.
Figure 1. Set-up of ultrasound machine and patient for injection.
Methods and Measurements
We used a standardized data collection tool to collect demographic and clinical information of all enrolled subjects, including age, sex, race, etiology for pain, whether or not the patient previously had a hip injection performed, and whether or not there were any complications or adverse events as described by the patient. Pain scores before and at various times after the hip injection were collected using a 0 to 10 Likert scale. A research assistant performed telephone follow-up to obtain pain scores after clinic discharge and determine whether or not any complications occurred according to a standardized questionnaire.
Figure 2. Real-time ultrasound view of needle insertion. The needle tip in the anterior synovial recess just distal to the femoral head is indicated with the long arrow. The femoral neck identified is indicated with the shorter arrow.
Outcomes
Our primary outcome was decrease in pain score at one week. We chose this as the primary outcome interval because the effect of local anesthetics will have worn off and the corticosteroid effect should have become evident. We additionally collected pain scores at five minutes, 10 minutes, and one month after the procedure.
Analysis
We collected descriptive statistics for our cohort and report median pain scores, with interquartile range (IQR), pre-injection, then post-injection at five minutes, 10 minutes, one week, and one month. We calculated mean change in pain scores within a 95% CI, from the pre-injection score to the post-injection intervals. Graphical and statistical methods were used to assess for normality of the pain score and pain score change distributions. Additionally, we determined mean changes in pain score stratified by pre-injection pain levels (mild<4, moderate 4-7, or severe >8). Finally, we used a multivariate linear regression model to assess whether covariates (age, sex, race, etiology of hip pain, or pre-injection pain score) were associated with reduction in pain score at one week. Statistical analyses were performed with Stata SE version 11 (StataCorp LP, College Station, TX).
RESULTS
We performed a total of 47 US-guided intra-articular hip injections on 44 subjects who met inclusion criteria. Three subjects received bilateral injections. Follow-up data were available for 42/47 (89.4%) hip injections at one week and 40/47 (85.1%) at one month. The median age was 56 years (IQR 45-62), and the majority of patients were female (63.6%). The age of patients ranged from 19 to 75 years. Additional demographic and clinical information of the cohort are available in Table 1. Osteoarthritis was the most common cause of chronic hip pain, present in 37/47 (78.2%) of included patients, followed by avascular necrosis 5/47 (10.6%), hip dysplasia 2/47 (4.3%), and other causes 3/47 (6.4%). Previous injections had been performed in 5/47 (10.6%) of patients.
Median pain scores at all-time intervals and mean changes in Likert pain score at the follow-up intervals are available in Table 2. We found clinically and statistically significant decreases in pain scores at all-time intervals, with the greatest improvement at 10 minutes after injection.
Table 1. Demographic features of 44 patients enrolled in ultrasound-guided corticosteroid hip injection study.*
| Characteristics | n (%) |
| Mean age (years +/- SD) | 53.02 +/- 11.5 |
| Male sex | 28 (63%) |
| Race/ethnicity | |
| Black | 17 (37%) |
| White | 14 (31%) |
| Latino | 9 (20%) |
| Asian | 4 (9%) |
| Etiology of hip pain | |
| Osteoarthritis | 37 (79%) |
| Avascular necrosis | 5 (11%) |
| Hip dysplasia | 2 (4%) |
| Unclear etiology | 2 (4%) |
| Post-infectious arthritis | 1 (2%) |
*44 patients, 47 hips injected.
For the primary outcome at one week, we found a mean decrease in Likert pain score from the pre-injection baseline of 3.85 with a 95% CI from 2.94-4.75. Additionally at one month, there was a mean decrease in Likert pain score from pre-injection baseline of 1.8 with a 95% CI from 1.12-2.53.
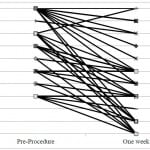
Graphical representation of individual pain scores for the 42 patients available for follow-up at the primary outcome of one week appears in Figure 3. Patients with both high and low levels of pre-procedural pain had improvement in their pain scores at one week. At one week follow-up one patient had an increase in his pain, three patients had no change in their pain, and seven patients had no pain at all after one week.
One patient reported transient dizziness after the procedure (lasting one minute). No other complications were reported or noted.
Multivariate analysis did not identify an association between age, sex, race, etiology of hip pain, or pre-injection pain score and change in hip pain at one week.
Table 2. Pain scores and differences at established intervals.
| Outcome | N (hips) | Median pre-injection pain score (IQR) |
Mean decrease in pain score from pre-injection baseline (95% CI) |
| Pre-injection | 47 | 8 (7-10) | – |
| 5 minutes | 47 | 2 (0-5) | 4.98 (4.18-5.78) |
| 10 minutes | 47 | 1 (0-4) | 5.57 (4.76-6.39) |
| 1 week | 42 | 4 (1-5) | 3.85 (2.94-4.75) |
| 1 month | 40 | 5 (4-8) | 1.8 (1.12-2.53) |
Figure 3. Individual patient pain scores from pre-injection to one week after hip injection.*
*Includes 42/47 injections available for follow up at one week.
DISCUSSION
Our study demonstrates that EM trainees can effectively perform US-guided corticosteroid hip injections as a method for the treatment of chronic hip pain. We noted a statistically significant reduction in pain scores at one week, and while the effect waned somewhat, patients continued to have modest pain relief at one month.
Our analysis demonstrates that US-guided corticosteroid intra-articular hip injection as performed by EM trainees is effective at decreasing chronic hip pain acutely and over a one-week period. This is a well-established and safe procedure practiced in various settings,4-9 and has been reported in the ED setting.14 In our study, junior EM providers with modest comfort with point-of-care US were able to successfully perform a US-guided hip injection after a brief tutorial.
Our results suggest that the technical difficulty of the procedure is low. The trainees performing the study were supervised, though the attending physician did not intervene during any of the procedures. Successful performance of the procedure was evident due to the dramatic improvement in pain after just ten minutes consistent with expected analgesia using bupivacaine.
The American College of Rheumatology advises corticosteroid injections as a first-line therapy for osteoarthritis of the hip.2 To our knowledge, the American College of Emergency Physicians has no comment on intra-articular steroid injections. Integration of this treatment to the care of ED patients should be considered for a number of reasons. Degenerative diseases of the hip, as well as other painful chronic musculoskeletal conditions, may be treated primarily in the ED setting with non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, opioid pain medications, and referral to specialists. There are significant risks associated with long-term use of NSAIDs and a growing concern over opioid drug abuse.15-17 In settings where access to primary care, pain management, and orthopedic specialists are limited, wait-times to see a practitioner may exceed months.18-20 This temporizing procedure may assist with chronic pain management, but, nonetheless, should only be performed in conjunction with appropriate consultation and referral to providers who will ultimately care for these patients. With this in mind, providing timely corticosteroid injections are an appealing approach to pain management for degenerative diseases of the hip to decrease repeat ED visits for chronic pain and opioid prescriptions. More specifically, similar attempts at moving towards multi-modal approaches to pain management have been shown to decrease the need for opioids, and ultimately may help curb the adverse effects and abuse associated with these and other controlled drugs.22
Integration of intra-articular hip injections into practice in the ED may not be successful without careful planning. The scope of this study does not assess the efficacy or feasibility in an ED and it if it is implemented the higher acuity and undifferentiated patient population needs to be considered. As with any procedure, clinicians should be adequately trained and comfortable and require the necessary credentialing. They should screen for patients with any signs of septic arthritis and should not perform the procedure in patients with signs of an infectious etiology for their pain, prosthetic hip joints, allergies to the medications, or overlying cellulitis.13 We would suggest that any patient with suspicion of a septic joint and a visualized effusion should have their joint aspirated using this same US-guided technique. In cases where the risks or benefits of an intra-articular hip injection are not clear, providers should not perform it or should obtain expert consultation. Additionally, patient consent is paramount. Known rare but significant complications of this procedure include avascular necrosis, post-procedural septic joint, and increased risk of post-operative septic joint when performed in proximity to surgery,13 and as such, patients must be informed and appropriately counseled. Finally, coordination of care beyond the ED is important, specifically with primary care and specialty clinic follow-up. Again, we reiterate that this procedure should not be done in lieu of appropriate referral. Rather, it can serve as an effective temporizing intervention for pain reduction, and should be followed by referral to an orthopedic surgeon, general practitioner, physical therapist, and/or pain specialist. Similarly, an understanding by the community of physicians who will be caring for these patients should be reached. It will be important, for example, that orthopedic surgeons seeing these patients in follow-up are aware of and comfortable with the performance of this procedure by emergency providers. In our experience at our medical center, there has been wide acceptance of intra-articular steroid injections of the hip by emergency providers, orthopedic specialists, and primary care physicians.
LIMITATIONS
There are inherent limitations to our study. Our non-blinded and uncontrolled method does not show that this method is superior compared to placebo, though this has already been established.2-6 As in most ultrasound studies, the issue of operator dependence is a limitation; however, EM providers may have extensive experience with US-guidance during procedures. There is no doubt that this procedure is unique as compared to vascular access or nerve blockade, and, as such, our training module and supervision by ultrasound fellowship-trained attending physicians was aimed at ensuring familiarity with the anatomy, needle insertion approach and angle, as well as appropriate injection of anesthetic and steroid. Training of providers on the unique technical aspects of this procedure will be paramount before adoption into clinical practice.
Additionally, for the purposes of this study, we enrolled patients directly from an orthopedic clinic. While it remains unclear if the benefit of this procedure would be as evident in ED patients, its benefit has been shown in various settings performed by providers of different specialties,4-9,13 suggesting that the benefit would also be realized in the ED setting. ED patients with hip pain are likely a more heterogeneous and higher acuity population in terms of presenting complaint, etiology of pain, or reliability for follow-up. While our clinic’s patient population represented a more heterogeneous population than previous studies in terms of etiology of disease, it may not approximate the heterogeneity likely to be seen in the ED. The patients in our study were identified by an orthopedic attending and selected as patients who would safely benefit from such a procedure, and as such we must temper our results in light of this limitation. Taken together, this limitation stresses the importance of careful ED patient selection and screening, and, in some instances, may support the use of consultation prior to performing the procedure.
CONCLUSION
This current study suggests that intra-articular hip injections for chronic pain conditions can be reliably taught to EM providers and, similar to previous studies, we have shown that it is safe and effective. It is entirely possible, however, that intra-articular hip injections may not be a feasible, efficient, or effective intervention when introduced into clinical practice in the ED. Prospective observational or randomized trials in this setting are warranted prior to wider acceptance of this procedure.
Future research should study the efficacy of this procedure in a larger population of ED patients. Analyses should specifically focus on proper patient selection, and identification of factors associated with higher efficacy (i.e., which etiology of hip pain benefits more from the injection). Meanwhile, educational resources should be made available to emergency providers who wish to learn this skill for their practice or study its use.
Footnotes
Supervising Section Editor: Anita Eisenhart, DO
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Erik Sorem Anderson, MD, 1411 E 31st Street, Oakland, CA 94602. Email: esoremanderson@gmail.com.
Submission history: Submitted November 25, 2013; Revision received June 1, 2014; Accepted September 2, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Video. Hip Injection
REFERENCES
- Hoaglund FT, Steinbach LS. Primary osteoarthritis of the hip: etiology and epidemiology. J Am Acad Orthop Surg. 2001;9(5).
- Hochberg M, Altman R, April K, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4).
- Zhang W, Doherty M, Arden N, et al. EULAR Evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Diseases. 2005;64(5).
- Lambert R, Hutchings E, Grace M, et al. Steroid injection for osteoarthritis of the hip: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2007;56(7).
- Sofka CM, Saboeiro G, Adler RS. Ultrasound-guided adult hip injections. J Vasc Interv Radiol. 2005;16(8).
- Caglar-Yagci H, Unsal S, Yagci I, et al. Safety and efficacy of ultrasound-guided intra-articular hylan G-F 20 injection in osteoarthritis of the hip: a pilot study. Rheumatol Int. 2005;25(5).
- Migliore A, Giovannangeli F, Granata M, et al. Safety profile of 185 ultrasound-guided intra-articular injections for treatment of rheumatic diseases of the hip. Reumatismo. 2004;56(2).
- Smith J, Hurdle MF, Weingarten TN. Accuracy of sonographically guided intra-articular injections in the native adult hip. J Ultrasound Med. 2009;28(3).
- Micu MC, Bogdan GD, Fodor D. Steroid injection for hip osteoarthritis: efficacy under ultrasound guidance. Rheumatology. 2010;49(8).
- Freeman K, Dewitz A, Baker WE. Ultrasound-guided hip arthrocentesis in the ED. Am J Emerg Med. 2007;25(1).
- Smith SW. Emergency physician-performed ultrasonography-guided hip arthrocentesis. Acad Emerg Med. 1999;6(1).
- Tsung JW, Blaivas M. Emergency department diagnosis of pediatric hip effusion and guided arthrocentesis using point-of-care ultrasound. J Emerg Med. 2008;35(4).
- Kruse DW. Intra-articular cortisone injection for osteoarthritis of the hip. Is it effective? Is it safe? Curr Rev Musculoskelet Med. 2008;1(3-4).
- Anderson ES, Herring AA, Bailey C, et al. Ultrasound-guided Intra-articular Hip Injection for Osteoarthritis Pain in the Emergency Department. West J Emerg Med. 2013;14(5).
- Henry D, McGettigan P. Epidemiology overview of gastrointestinal and renal toxicity of NSAIDs. Int J Clin Pract Suppl. 2003;135.
- Ballantyne J, Mao J. Opioid Therapy for Chronic Pain. N Engl J Med. 2003;349.
- Compton W, Volkow N. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81(2).
- Mandl P, Naredo E, Conaghan P, et al. Practice of ultrasound-guided arthrocentesis and joint injection, including training and implementation, in Europe: results of a survey of experts and scientific societies. Rheumatology. 2012;51(1).
- Clancy CM, Franks P. Utilization of specialty and primary care: the impact of HMO insurance and patient-related factors. J Fam Pract. 1997;45(6).
- Cook N, Hicks L, O’Malley AJ, et al. Access to specialty care and medical services in community health centers. Health Aff. 2007;26(5).
- Mort EA, Edwards JN, Emmons DW, et al. Physician response to patient insurance status in ambulatory care clinical decision-making. Implications for quality of care. Med Care. 1996;34(8).
- Tsui P, Scheuermann J, Hildebrand S, et al. A multidisciplinary outpatient pain management opioid reduction pilot program pain. J Pain. 2013;14(4).