Archives
Emergency Department Operations
Machine Learning in Relation to Emergency Medicine Clinical and Operational Scenarios: An Overview
Westjem Read More
Emergency Department Operations
Transition of Care from the Emergency Department to the Outpatient Setting: A Mixed-Methods Analysis
Westjem Read More
Emergency Department Operations
A Novel Approach to Addressing an Unintended Consequence of Direct to Room: The Delay of Initial Vital Signs
Westjem Read More
Emergency Department Operations
Decreasing Emergency Department Walkout Rate and Boarding Hours by Improving Inpatient Length of Stay
Westjem Read More
Emergency Department Operations
Magnetic Resonance Imaging Utilization in an Emergency Department Observation Unit
Westjem Read More
Emergency Department Operations
Agreement Between Serum Assays Performed in ED Point-of-Care and Hospital Central Laboratories
Westjem Read More
Emergency Department Operations
Use of Physician-in-Triage Model in the Management of Abdominal Pain in an Emergency Department Observation Unit
Westjem Read More
Emergency Department Operations
Cross-Continuum Tool Is Associated with Reduced Utilization and Cost for Frequent High-Need Users
Westjem Read More
Emergency Department Operations
Mobile COWs (Computer on Wheels): Hamburger or VEAL?
Westjem Read More
Emergency Department Operations
Does Pneumatic Tube System Transport Contribute to Hemolysis in ED Blood Samples?
Westjem Read More
Emergency Department Operations
Wide Variability in Emergency Physician Admission Rates: A Target to Reduce Costs Without Compromising Quality
Westjem Read More
Emergency Department Operations
Emergency Department Length of Stay for Maori and European Patients in New Zealand
Westjem Read More
Emergency Department Operations
Comparison of Result Times Between Urine and Whole Blood Point-of-care Pregnancy Testing
Westjem Read More
Emergency Department Operations
Physician Quality Reporting System Program Updates and the Impact on Emergency Medicine Practice
Westjem Read More
Emergency Department Operations
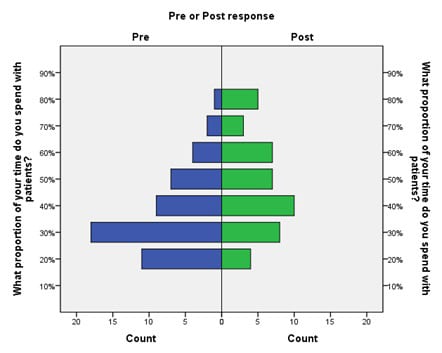
Scribe Impacts on Provider Experience, Operations, and Teaching in an Academic Emergency Medicine Practice
Westjem Read More
Emergency Department Operations
Identifying Patient Door-to-Room Goals to Minimize Left-Without-Being-Seen Rates
Westjem Read More
Emergency Department Operations
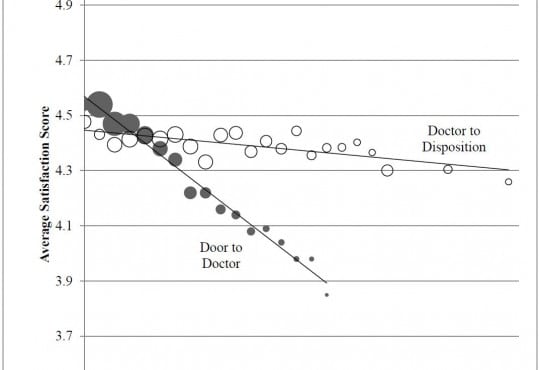
Demographic, Operational, and Healthcare Utilization Factors Associated with Emergency Department Patient Satisfaction
Westjem Read More
Emergency Department Operations
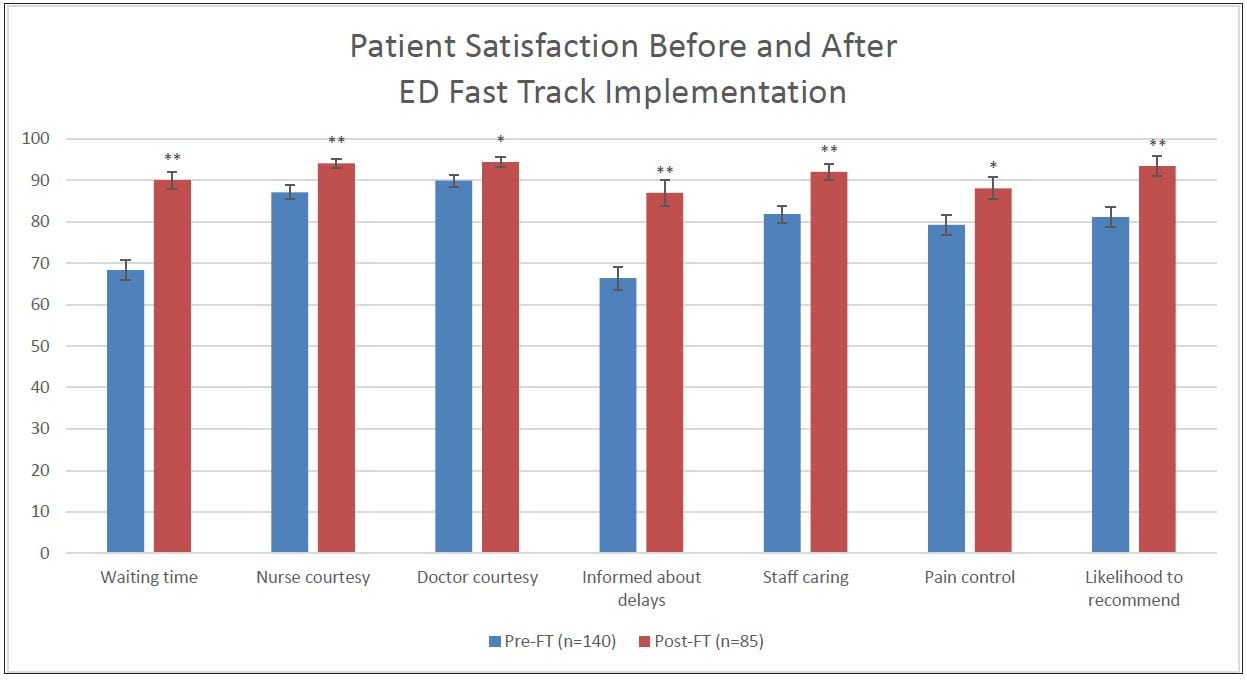
Effect of an Emergency Department Fast Track on Press-Ganey Patient Satisfaction Scores
Westjem Read More
Emergency Department Operations
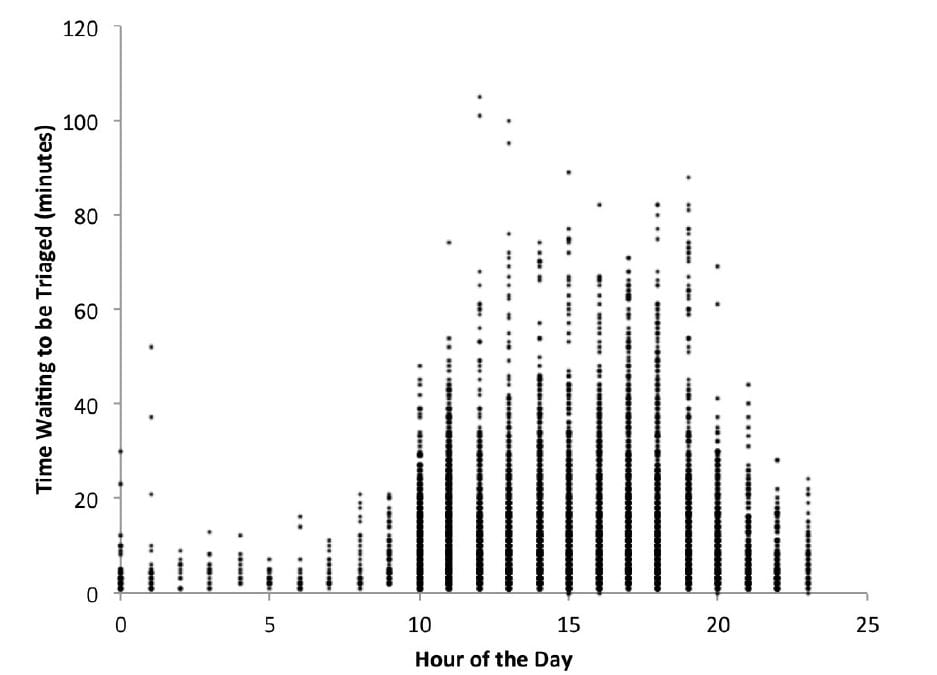
Waiting for Triage: Unmeasured Time in Patient Flow
Westjem Read More
Emergency Department Operations
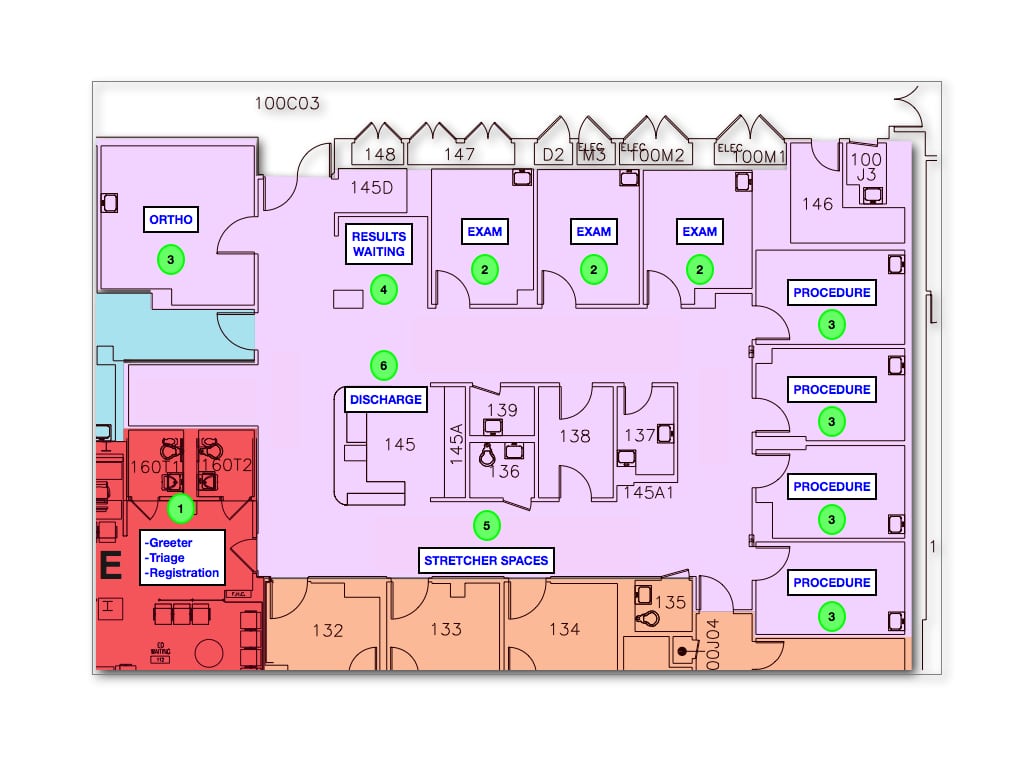
Using Lean-Based Systems Engineering to Increase Capacity in the Emergency Department
Westjem Read More
Emergency Department Operations
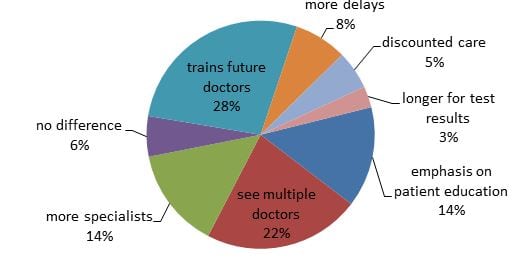
What Do Patients Want? Survey of Patient Desires for Education in an Urban University Hospital
Westjem Read More
Emergency Department Operations
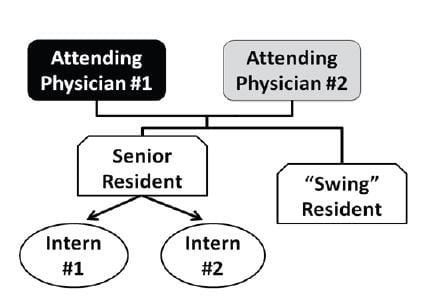
Implementation of a Team-based Physician Staffing Model at an Academic Emergency Department
WestJEM Read More
Emergency Department Operations
Reducing Patient Placement Errors in Emergency Department Admissions: Right Patient, Right Bed
WestJEM Read More
Emergency Department Operations
Adherence to Head Computed Tomography Guidelines for Mild Traumatic Brain Injury
WestJEM Read More
Emergency Department Operations