| Author | Affiliation |
|---|---|
| Landon A. Jones, MD | Department of Emergency Medicine, SUNY Upstate Medical University, Syracuse, New York |
| Eric J. Morley, MD, MS | Department of Emergency Medicine, Stony Brook University Medical Center, Stony Brook, New York |
| William D. Grant, EdD | Department of Emergency Medicine, SUNY Upstate Medical University, Syracuse, New York |
| Susan M. Wojcik, PhD | Department of Emergency Medicine, SUNY Upstate Medical University, Syracuse, New York |
| William F. Paolo, MD | Department of Emergency Medicine, SUNY Upstate Medical University, Syracuse, New York |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction
Traumatic brain injury (TBI) is a significant health concern. While 70–90% of TBI cases are considered mild, decision-making regarding imaging can be difficult. This survey aimed to assess whether clinicians’ decision-making was consistent with the most recent American College of Emergency Physicians (ACEP) clinical recommendations regarding indications for a non-contrast head computed tomography (CT) in patients with mild TBI.
Methods
We surveyed 2 academic emergency medicine departments. Six realistic clinical vignettes were created. The survey software randomly varied 2 factors: age (30, 59, or 61 years old) and presence or absence of visible trauma above the clavicles. A single important question was asked: “Would you perform a non-contrast head CT on this patient?”
Results
Physician decision-making was consistent with the guidelines in only 62.8% of total vignettes. By age group (30, 59, and 61), decision-making was consistent with the guidelines in 66.7%, 47.4%, and 72.7% of cases, respectively. This was a statistically-significant difference when comparing the 59- and 61-year-old age groups. In the setting of presence/absence of trauma above the clavicles, respondents were consistent with the guidelines in 57.1% of cases. Decision-making consistent with the guidelines was significantly better in the absence of trauma above the clavicles.
Conclusion
Respondents poorly differentiated the “older” patients from one another, suggesting that respondents either inappropriately apply the guidelines or are unaware of the recommendations in this setting. No particular cause for inconsistency could be determined, and respondents similarly under-scanned and over-scanned in incorrect vignettes. Improved dissemination of the ACEP clinical policy and recommendations is a potential solution to this problem.
INTRODUCTION
Traumatic brain injury (TBI) is a significant health concern and accounts for approximately 1.2 million emergency department (ED) visits yearly, translating to about 1% of total ED visits annually.1,2 Of these TBI cases, 70–90% are considered mild and, although most are mild, decision-making regarding imaging can be difficult.3–6 Ionizing radiation from computed tomography (CT) imaging is not without risk, and recent literature has demonstrated an increased risk of both leukemias and brain tumors in children.7 While the negative health effects of ionizing radiation in adults is believed to be milder, judicious and cost-reductive use of CT imaging in an era of rising healthcare costs—without sacrificing patient care—is important.
In 2008, the American College of Emergency Physicians (ACEP) revised and disseminated their most recent clinical policy regarding recommendations for a non-contrast head CT in the setting of mild TBI.8 In this revised policy, the authors identified Level A, Level B, and Level C recommendations. In the setting of mild TBI—defined as non-penetrating trauma presentation within 24 hours in patients at least 16 years old with a Glasgow Coma Scale (GCS) of 14 or 15—10 Level A recommendations were made including: headache, vomiting, age older than 60 years, drug/alcohol intoxication, deficits in short-term memory, physical evidence of trauma above the clavicles, post-traumatic seizure, GCS<15, focal neurologic deficits, or coagulopathy. Patients who had experienced either loss of consciousness (LOC) or post-traumatic amnesia and 1 of the 10 previously-mentioned findings were recommended to receive a non-contrast head CT according to Level A recommendations.8
No determination has been made as to whether or not these most recent ACEP guidelines are routinely applied appropriately and, if they are not, what factors lead to a varied practice inconsistent with these guidelines. To assess this hypothesis, a survey was undertaken of 2 separate emergency medicine (EM) departments. We hypothesized that EPs are aware of the most recent ACEP clinical policy recommendations regarding indications for a non-contrast head CT in patients with mild TBI and that they appropriately apply these recommendations.
We created a set of realistic clinical vignettes, with a supplemental categorization survey, that describes a typical patient encounter in the ED. Each vignette describes a typical ED patient with mild TBI and then asks the respondent to make a single decision regarding whether or not to obtain a non-contrast head CT.
METHODS
For this survey study, we created 6 realistic clinical vignettes, followed by a supplemental categorization survey, which described a common patient encounter in the ED. Voluntary participants were directed to a web-based online survey. The survey program (DataMomentum [Ithaca, NY]) then presented, in a random order, 1 of the 6 head CT scenarios. Each vignette described a typical ED patient with mild TBI and then asked the respondent to make a single decision regarding whether or not to obtain a non-contrast head CT. In addition, all respondents were then asked to complete the same additional 8 supplemental categorization questions—none of which gathered any identifiable information. Each survey responder received only 1 random vignette total.
Two separate academic EM department chairs were sent a single invitation email. This email briefly explained the goal of the study and contained a link to an online web-based survey. If agreeable, the department chairmen were requested to forward the email once to their respective intra-departmental list-serve of physicians, including both residents and faculty. This process was repeated a second time 14 days later. Voluntary participants were directed to a web-based online survey.
The survey program then presented, in a random order, 1 of the 6 head CT scenarios. The survey software randomly varied 2 factors: age (30, 59, or 61 years old) and presence or absence of visible trauma above the clavicles. A representative sample of the vignette appears in Figure. These variations provided 6 different realistic clinical vignettes with a single independent variable in each. Ultimately, this survey asked a single important question: “Would you perform a non-contrast head CT on this patient?”
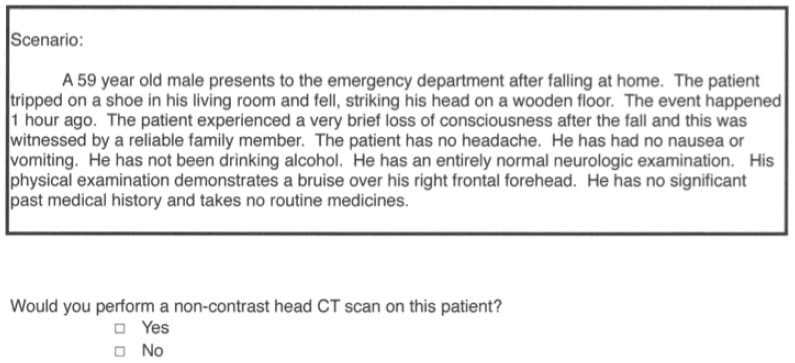
Figure
Representative vignette sample in a survey of emergency physician adherence to head computed tomography (CT) guidelines.
Responses were recorded—without identifiable information—by a web-based online service. The online survey remained open and collected responses for 6 weeks from the time of initial email to the department chairmen. We obtained IRB exemption from the local institutional review committees at both these respective institutions.
We tabulated and analyzed result data with MedCalc®, version 12.3.0.0 (MedCalc Software, Ostend, Belgium). We assessed decision-making results, both consistent and inconsistent with the ACEP guidelines, in regards to both age (30, 59, and 61 years) and presence or absence of trauma above the clavicles.
RESULTS
“The introductory email and web-based survey link were forwarded by the department chairmen of 2 separate academic EM programs to their respective faculty and residents.” Of the 241 total potential survey respondents at these institutions, 121 responded (50.2%).
Of those who did respond, 94.2% (114/121) completed the voluntary 8-question supplemental categorization survey. Respondents categorized their practice as a combination of “Some adults/Some pediatrics” in 79.8%, “Adults only” in 14.9%, and “Pediatrics only” in 5.3%. Ninety-nine of 114 respondents (86.8%) identified themselves as EM residency trained. There was no statistical difference between appropriate application of the guidelines in respondents who did and did not train in EM residency programs (62.6% versus 60.0%). Respondents also identified their practice setting as “Academic” in 99/114 (86.8%) of surveys. “Community” (8.8%) or “Other” (4.4%) was identified as the practice setting in the remainder of surveys completed. One hundred of 114 (87.7%) respondents identified their ED as a “Level I” trauma center, while 7.0% (8/114) and 5.3% (6/114) identified their practice location as a “Level II” trauma center or “Not a trauma center,” respectively. Finally, 91.2% (104/114) of categorization surveys responded “yes” when asked if they had a “dedicated CT scanner located in your emergency department.”
Physician decision-making in the setting of mild TBI was consistent with the most recent ACEP recommendations in only 62.8% (76/121) of total vignettes. By age group (30, 59, and 61), responses were consistent with the guidelines in 66.7% (26/39), 47.4% (18/38), and 72.7% (32/44) of cases, respectively. When comparing results by age group, there was a statistically-significant difference between the results comparing the 59- and 61-year-old age groups (p=0.034). There was no statistical significance when comparing the results of the 30- versus 59-year-old age groups (p=0.139) or when comparing the 30- versus 61-year-old age groups (p=0.723).
In the setting of presence/absence of trauma above the clavicles at ages 30 and 59, respondents appropriately applied the guidelines in 57.1% (44/77) of cases. Calculations regarding presence or absence of supraclavicular trauma were not performed in the 61-year-old group because all patients over 60 years are recommended to receive a non-contrast head CT in this setting according to guidelines. In the presence of trauma above the clavicles, responses were consistent with the most recent ACEP recommendations in only 43.2% (16/37) of vignettes. In the absence of trauma, the guidelines were appropriately applied in 70% (28/40) of cases. These results were statistically significant (p=0.032) when comparing the presence versus absence of supraclavicular trauma. Appropriate application of the guidelines was better (70.0% versus 43.2%) in the absence of trauma above the clavicles.
DISCUSSION
Clinical guidelines exist to offer the best evidence-based diagnostic or therapeutic recommendations in clinical scenarios where evidence exists. These recommendations are traditionally categorized as Level A, B, or C recommendations according to the strength of evidence on that topic. When strong evidence exists, guidelines give Level A recommendations. When either poor or conflicting data exist—or there is an absence of data on the topic—these recommendations are labeled as Level C recommendations. Evidence with moderate clinical certainty falls into the Level B recommendations. In instances where there is a paucity of data on a topic, clinical guidelines will usually make recommendations based upon “expert consensus.”
Guideline recommendations serve to increase the quality of care, introduce and educate practitioners on best-evidence practice, increase the uniformity of care, and reduce cost.9,10 They have also been shown to minimize increases in practice variation.9 Interestingly, though, guideline recommendations have a wide adherence range from 20% to nearly 100%.11 Since practice recommendations themselves, do not automatically change clinician practice, the reasons for variation also need to be explored. For example, the stakeholder’s impact—meaning the reputation of the professional college or professional network producing it—has been reported to be important in the adoption of these best-evidence practices.10 For this reason, we also sought to determine reasons behind clinician decision-making that varied from the recommendations.
In 2008, ACEP revised and disseminated their most recent clinical policy regarding recommendations for a non-contrast head CT in the setting of mild TBI.8 In this revised policy, the authors identified Level A, Level B, and Level C recommendations. In the setting of mild TBI—defined as non-penetrating head trauma presentation within 24 hours in patients at least 16 years old with a GCS of 14 or 15—10 Level A recommendations were made including: headache, vomiting, age older than 60 years, drug/alcohol intoxication, deficits in short-term memory, physical evidence of trauma above the clavicles, post-traumatic seizure, GCS<15, focal neurologic deficits, or coagulopathy. Patients who had experienced either loss of consciousness (LOC) or post-traumatic amnesia AND 1 of the 10 previously-mentioned findings were recommended to receive a non-contrast head CT according to Level A recommendations.8
After performing a literature review, we were unable to identify any studies that addressed the application of the ACEP clinical guidelines in the setting of mild TBI. In reviewing the Level A recommendations, we believe that patient age and the presence of supraclavicular evidence of trauma are the 2 best objective data points to evaluate how emergency providers might determine whether or not to image these patients with a non-contrast head CT. These indicators can be easily and objectively assessed by the clinician and are the least ambiguous of the 10 previously-mentioned findings. Indicators such as headache, vomiting, drug/alcohol intoxication, and coagulopathy were felt to be subjective in nature. The vignette patient ages of 30, 59, and 61 years were chosen purposefully in an effort to better differentiate the responders’ awareness of the important age of 60 years in the clinical policy recommendations. Our hypothesis was that EPs are aware of the guidelines and their decision-making is consistent with the most recent ACEP guidelines in the setting of mild TBI.
Overall, physician decision-making was consistent with the guidelines in only 62.8% (76/121) of total vignettes. When analyzed by patient age—30, 59, and 61 years—the clinical guidelines were applied appropriately in 66.7% (26/39), 47.4% (18/38), and 72.7% (32/44) of cases, respectively. When these age groups were compared, there was no significance when comparing the results of the 30- versus 59-year-old groups (p=0.139) or the 30- versus 61-year-old groups (p=0.723), suggesting that respondents correctly identify the 30-year-old patient as a lower risk age group. Conversely, when comparing the results of the 59- versus 61-year-old groups, there was a significant difference (p=0.034). This inconsistent application of the most recent ACEP guidelines suggests 1 of 2 things—either these respondents inappropriately apply the guidelines, whether purposefully or not, or are unaware of the ACEP clinical guidelines. Furthermore, this argues that survey responders poorly differentiate the 59-year-old from the 61-year-old patient. Our results suggest that practitioners see these 2 age groups as a single “older” patient and their application of the guidelines to some members of this “older” group are inconsistent with the most recent ACEP clinical guidelines. Our hypothesis was that EM physicians are aware of the guidelines and appropriately apply the guidelines in mild TBI. This may only be the case in approximately 60% of patient encounters. Both instances argue that better dissemination and diffusion of the guidelines—whether in hard copy or electronic version—are indicated.
In the setting of the presence or absence of trauma above the clavicles, the guidelines were appropriately applied in only 57.1% (44/77) of cases. With the appropriate application of the guidelines significantly higher in the absence, compared to the presence, of trauma (70.0% versus 43.2%, p=0.032), this might suggest that practitioners appropriately apply the guidelines better when there is no evidence of trauma above the clavicles. Again, a potential solution to this problem is improved dissemination of the ACEP clinical policy.
Since survey respondents inappropriately applied the guidelines in 37.2% (45/121) of vignettes, we sought to figure out why this is the case. For this purpose, we included a voluntary supplemental categorization study that included no identifiable information. This was completed by 94.2% of these survey responders. Of survey responders, 94.7% (108/114) described their practice as either “Some Adults/Some Pediatrics” or as “Adults Only,” suggesting that the survey responders were an appropriate survey population and have experience with treating adults. The vignettes included only patients in the “Adult” range. Only 5.3% (6/121) of respondents have only pediatric patient experience.
This categorization study also evaluated whether responders were EM residency trained. Ninety-nine of 114 (86.8%) respondents were EM residency trained and there was no statistical difference between vignette responses consistent with the most recent ACEP clinical policy between respondents who did and did not train in EM residency programs (62.6% versus 60.0%). Similarly, 86.8% (99/114) of responders described their practice as “Academic” while the remainder described their practice setting as either “Community” or “Other.” The responders who were not EM residency trained were not the same population as the “Community” or “Other” population, meaning these were not the same 15/114 survey responders. With the categorization data collected, our survey study is unable to determine whether community-based physicians apply the guidelines differently than academic-based physicians and this was not a goal of our study. Finally, 91.2% (104/114) of categorization surveys responded “yes” when asked if they had a “dedicated CT scanner located in your emergency department.” This question was asked to determine whether distance to a CT scanner potentially affected a responder’s answer. Ultimately, no particular cause for this variation in practice pattern could be identified.
A final topic of interest was in regards to over- versus under-scanning individuals with a potential need for a head CT. Ionizing radiation has significant risks and a recent study by Pearce et al7 has demonstrated an increase in relative risk of both leukemia and brain tumors in children receiving CT scans. While the negative health effects of ionizing radiation in adults is believed to be milder, judicious and cost-reductive use of CT imaging in an era of rising healthcare costs—without sacrificing patient care—is important. It would be an interesting finding if responders tended to over-scan and were inconsistent with the ACEP clinical policy guidelines. According to our collected survey data, though, respondents did not consistently over-scan. There was no significant difference. In cases where the guidelines were applied inappropriately, over-scanning occurred in 30.0% (12/40) of cases and under-scanning occurred in 40.7% (33/81) of cases. This data suggests that respondents over-scanned and under-scanned in a similar percentage of incorrect vignettes. They did not consistently over-scan the vignette patients.
LIMITATIONS
Limitations to our survey study include the small size of the study and the predominantly academic practice population of the survey responders. Clinicians in the community may practice differently compared to academic practitioners. Academic EM residency programs include designated journal club discussions and may remain more up-to-date on current topics. Conversely, though, EM residency programs also include residents with less experience compared to seasoned community clinicians. For this reason, the effect of a larger community-based clinician population is unpredictable.
Another limitation to our study was the inability to determine if survey responders were aware of the guidelines. Our aim was to evaluate the surveyors’ application of the most recent ACEP guidelines without their knowledge, so as to minimize bias. We did not seek to “alert” them that we were evaluating the ACEP mild-TBI clinical guidelines. One inherent limit to this, though, is that it is difficult to differentiate whether they inconsistently apply the guidelines or have minimal or no knowledge of the guidelines’ recommendations. Our study inherently hypothesized that the ACEP mild-TBI guidelines were both reproducible and reasonable and represented “best practice evidence” in regards to mild TBI. Poor compliance with the recommendations could simply be the failure of practitioners to apply the best evidence-based care. Conversely, though, non-compliance could be secondary to an intrinsic limitation in the applicability of the guidelines (i.e., they are difficult to apply) or poor penetrance of the ACEP guidelines’ recommendations. We sought to minimize intrinsic limitation by minimizing ambiguity in our clinical vignettes. Low penetrance of the ACEP guidelines, though, could also lead to the poor guideline application results found in our study and would further strengthen the argument of needed improvement in clinical guideline dissemination and diffusion. We were unable to determine whether the survey responders simply inappropriately applied the guidelines or did not know about the guidelines. Additionally, while other studies, such as the New Orleans Criteria and Canadian Head CT Rule, are incorporated into the ACEP clinical recommendations, some responders may have chosen to only apply the age cut-off of the Canadian Head CT Rule (age≥65).12,13
Lastly, like all survey studies, there are the limitations that exist between vignettes and actual practice. Practitioners may practice in the way their vignette responses indicated, but we are unable to confirm whether their actual practice is consistent. A number of other factors such as anecdotal experience, medico-legal concern, and other confounders may influence their real world practice.
CONCLUSION
In the setting of mild TBI, physician decision-making was consistent with the most recent ACEP guidelines in only 62.8% (76/121) of total vignettes. Age and the presence/absence of supraclavicular trauma were the 2 objective Level A recommendations evaluated in our survey study. Respondents poorly differentiated the “older” patients from one another, suggesting that respondents either inappropriately apply the guidelines or are unaware of the guideline recommendations in this setting. Also, surveyor responses were more consistent with the ACEP guidelines in the absence of supraclavicular trauma compared to the presence of trauma above the clavicles. No particular reasons for responses inconsistent with the ACEP guidelines could be determined, and respondents similarly under-scanned and over-scanned in incorrect vignettes. One potential solution to this issue is improved dissemination—whether in hard copy or electronic version—of the most recent ACEP clinical policy on imaging in the setting of mild TBI.
Footnotes
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Eric J. Morley, MD, MS. Department of Emergency Medicine, SUNY Upstate, 750 E Adams St, Syracuse, NY 13210. Email: ericohnmorley@gmail.com. 7 / 2014; 15:459 – 464
Submission history: Revision received October 3, 2013; Submitted December 9, 2013; Accepted January 6, 2014
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1 Rutland-Brown W, Langlois JA, Thomas KE Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006; 21:544-548
2 Faul M, Xu L, Wald MM Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control Web site. ;
3 Numminen HJ The incidence of traumatic brain injury in an adult population–how to classify mild cases?. Eur J Neurol. 2011; 18:460-464
4 Holm L, Cassidy JD, Carroll LJ Summary of the WHO collaborating centre for neurotrauma task force on mild traumatic brain injury. J Rehabil Med. 2005; 37:137-141
5 Rickels E, von Wild K, Wenzlaff P Head injury in Germany: A population-based prospective study on epidemiology, causes, treatment and outcome of all degrees of head-injury severity in two distinct areas. Brain Inj. 2010; 24:1491-1504
6 Shukla D, Devi BI Mild traumatic brain injuries in adults. J Neurosci Rural Pract. 2010; 1:82-88
7 Pearce MS, Salotti JA, Little MP Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet. 2012; 380:499-505
8 Jagoda AS, Bazarian JJ, Bruns JJ Clinical policy: Neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008; 52:714-748
9 de Jong JD, Grownewegen PP, Spreeuwenberg P Do guidelines create uniformity in medical practice?. Soc Sci Med. 2010; 70:209-216
10 McKinlay E, McLeod D, Dowell A Clinical practice guidelines’ development and use in New Zealand: an evolving process. N Z Med J. 2004; 117:U999
11 Halm EA, Atlas SJ, Borowsky LH Understanding physician adherence with a pneumonia practice guideline: effects of patient, system, and physician factors. Arch Intern Med. 2000; 160:98-104
12 Haydel MJ, Preston CA, Mills TJ Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000; 13:100-105
13 Stiell IG, Wells GA, Vandemheen K The canadian CT head rule for patients with minor head injury. Lancet. 2001; 5:1391-1396


