| Author | Affiliation |
|---|---|
| C. Eric McCoy, MD, MPH | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
| Bharath Chakravarthy, MD, MPH | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
| Shahram Lotfipour, MD, MPH | University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California |
ABSTRACT
The Centers for Disease Control and Prevention (CDC) has published significant data and trends related to the national public health burden associated with trauma and injury. In the United States (U.S.), injury is the leading cause of death for persons aged 1–44 years. In 2008, approximately 30 million injuries resulted in an emergency department (ED) evaluation; 5.4 million (18%) of these patients were transported by Emergency Medical Services (EMS).1 EMS providers determine the severity of injury and begin initial management at the scene. The decisions to transport injured patients to the appropriate hospital are made through a process known as “field triage.” Since 1986, the American College of Surgeons Committee on Trauma (ACS-COT) has provided guidance for the field triage process though its “Field Triage Decision Scheme.” In 2005, the CDC, with financial support from the National Highway Traffic Safety Administration (NHTSA), collaborated with ASC-COT to convene the initial meeting of the National Expert Panel on Field Triage (the Panel) to revise the decision scheme. This revised version was published in 2006 by ASC-COT, and in 2009 the CDC published a detailed description of the scientific rational for revising the field triage criteria entitled, “Guidelines for Field Triage of Injured Patients.”2–3 In 2011, the CDC reconvened the Panel to review the 2006 Guidelines and recommend any needed changes. We present the methodology, findings and updated guidelines from the Morbidity & Mortality Weekly Report (MMWR) from the 2011 Panel along with commentary on the burden of injury in the U.S., and the role emergency physicians have in impacting morbidity and mortality at the population level.
CDC MORBIDITY & MORTALITY WEEKLY REPORT FINDINGS
In the January 2012 Morbidity & Mortality Weekly Report, the Centers for Disease Control and Prevention (CDC) published the 2011 recommendations of the National Expert Panel on Field Triage, the latest update on the “Guidelines for Field Triage of Injured Patients” since 2006. The MMWR report described the dissemination and impact of the 2006 Guidelines, outlined the methodology used by the Panel for its 2011 review, explained the revisions and modifications of the 4 triage criteria (physiologic, anatomic, mechanism-of-injury, and special considerations), updated the schematic of the 2006 guidelines, and provided the rationale used by the Panel. They noted that the report is intended to help prehospital–care providers in their daily duties recognize individual injured patients who are most likely to benefit from specialized trauma center resources, and not intended as a mass casualty or disaster triage tool.
BACKGROUND
Trauma and injury play a significant role in the disease burden suffered by the population. In the U.S., unintentional injury is the leading cause of death for persons aged 1–44 years.4 In 2008, injuries accounted for approximately 181,226 deaths in the U.S.5 In the same year, approximately 30 million injuries were serious enough to prompt an emergency department (ED) visit; 5.4 million (18%) of these injuries were transported by Emergency Medical Services (EMS) personnel.1 A national evaluation on the effect of trauma-center care on mortality published in the New England Journal of Medicine found that the risk of death is significantly lower when care is provided in a trauma center than in a nontrauma center.6 EMS personnel provide the entry point for which injured patients enter the health care system. They are responsible for the initial evaluation and management of injured patients in the field and play an integral role in the triage of the injured patient to the appropriate health care facility. The triage of injured patients to the appropriate health care facility plays a substantial role in patient outcome. The National Study on the Costs and Outcomes of Trauma (NSCOT) identified a 25% relative risk reduction in mortality for severely injured adult patients who received care at a Level I trauma center rather than at a nontrauma center.6 They concluded that the risk of death is significantly lower when care is provided in a trauma center than in a non-trauma center and argued for continued efforts at regionalization.
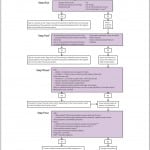
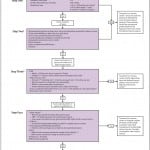
In 2005, the CDC, with financial support from NHTSA, collaborated with American College of Surgeons Committee on Trauma (ACS-COT) to convene the initial meetings of the Panel. The Panel comprises persons with expertise in acute injury care, including EMS providers and medical directors, state EMS directors, hospital administrators, adult and pediatric trauma surgeons, persons in the automotive industry, public health personnel, and representatives of federal agencies.1 The Panel is charged with periodically reevaluating the Guidelines in the context of recently published literature and community experience and, as appropriate, making revisions. In 2006, the end product of that comprehensive revision process was published by ACS-COT with the name “Field Triage Decision Scheme.” (Figure 1) In 2009, the CDC published a detailed description of the scientific rational for revising the field triage criteria entitled “Guidelines for Field Triage of Injured Patients: recommendations of the National Expert Panel on Field Triage.” In 2011, the Panel reconvened to review the 2006 Guidelines and made revisions where appropriate. A major outcome produced from these meetings was the latest iteration of the Guidelines. (Figure 2)
METHODS
The Morbidity & Mortality Weekly Report on the Guidelines for Field Triage of Injured Patients described the methodology used by the Panel for its 2011 review. Published peer-reviewed research was the primary basis for making revisions to the Guidelines. Articles were identified by a structured Medline literature search for articles related to the overall field triage process that were published between January 1, 2006 and May 1, 2011. A total of 2,052 articles were identified for further review. Through an iterative and collaborative process, 4 CDC injury researchers reviewed abstracts to determine their appropriateness for presentation to the Panel. This process identified 241 articles pertaining to field triage. To supplement the structured literature searches, a working group of the Panel reviewed the selected articles, identified additional relevant literature that had not been examined, and made recommendations regarding individual components of the Guidelines. This process identified an additional 48 articles, which, together with the originally identified 241 articles, were provided to the Panel for review. The final recommendations of the Panel were based on the best available evidence and expert opinion where the evidence was lacking.
2011 FIELD TRIAGE GUIDELINE RECOMMENDATIONS
The MMWR elaborated on the Panel recommendations and broke each step of the triage process into its own respective section. There are four steps to the triage process: Step One: Physiologic Criteria, Step Two: Anatomic Criteria, Step Three: Mechanism-of-Injury Criteria, and Step Four: Special Considerations. They also provided a summary of the modifications to the previously published 2006 Guidelines. (Box 1) For the following sections pertaining to the four steps, the reader is encouraged to refer to Figure 2.
Summary of modifications to the 2006 Guidelines.
Step One: Physiologic Criteria
In Step One, the Glasgow Coma Scale score (GCS), and Respiratory Rate criteria were modified. Step One is intended to allow for rapid identification of critically injured patients by assessing level of consciousness (GCS) and measuring vital signs. Vital sign criteria have been used since the 1987 version of the ACS Field Triage Decision Protocol, and systolic blood pressure (SBP) <90 mmHg and respiratory rate <10 or >29 breaths per minute remain significant predictors of severe injury and need for a high level of trauma care.1 The report commented on how the GCS criteria guidelines were changed from GCS <14 to GCS ≤13 owing to many readers of the previous guidelines perceiving GCS <14 criterion to mean a recommendation to take patients with at GCS ≤14 to a trauma center. After reviewing the literature, the Panel added “or need for ventilatory support” to the respiratory rate criterion, recognizing that adults and children requiring advanced airway interventions represent a very high-risk group, whether or not other physiologic abnormalities were present.
The Panel recommended transport to a facility that provides the highest level of care within the defined trauma system if any of the following are identified:
-
Glasgow Coma Scale ≤13, or
-
SBP of <90 mmHg, or
-
Respiratory rate of <10 or >29 breaths per minute (<20 in infant aged <1 year), or need for ventilatory support
Step Two: Anatomic Criteria
Step Two of the Guidelines recognizes that certain patients, on initial presentation in the field, have normal physiology but have an anatomic injury that might require the highest level of care within the defined trauma system. The criteria pertaining to chest and extremity injury were modified. The “crushed, degloved, or mangled extremity” criterion was modified to include “pulseless” extremities after review of the literature and because vascular injury of the extremity might lead to significant morbidity and mortality, require a high level of specialized trauma care involving multiple medical specialties, and be present in the absence of a crushed, degloved, or mangled extremity.1,7 The “flail chest” criterion was modified to “chest wall instability or deformity (e.g., flail chest).” The report commented on how the Panel recognized that the field diagnosis of a flail chest is rare and that this criterion might be too restrictive, citing studies where flail chest was identified in 0.002% of patients and in 0.02% of patients with chest injuries.8–9 The Panel decided that the terminology “chest wall instability or deformity (e.g., flail chest)” more accurately describes what EMS providers are asked to identify in the field, and the broader terminology ensures that additional blunt trauma to the chest will be identified and the patient transported to the appropriate facility. The “All penetrating injuries to the head, neck, torso, and extremities proximal to the elbow and knee” criterion was slightly modified to read “elbow or knee.” Consequently, the “amputation proximal to wrist and ankle” criterion was slightly modified to read “wrist or ankle.”
The Panel recommended transport to a facility that provides the highest level of care within the defined trauma system if any of the following are identified:
-
All penetrating injuries to head, neck, torso, and extremities proximal to the elbow or knee;
-
Chest wall instability or deformity (e.g., flail chest);
-
Two or more proximal long-bone fractures;
-
Crushed, degloved, mangled, or pulseless extremity;
-
Amputation proximal to the wrist or ankle;
-
Pelvic fractures;
-
Open or depressed skull fractures; or
-
Paralysis
Step Three: Mechanism of Injury
An injured patient who does not meet Step One or Step Two should be evaluated in terms of mechanism of injury (MOI) to determine if the injury might be severe but occult. The “high-risk auto crash: intrusion >12 inches occupant site; >18 inches any site” criterion was modified to include roof intrusion. The report cites studies demonstrating the utility of MOI in decreasing the rate of undertriage compared to when physiologic and anatomic criterion were used alone, as well as MOI being an independent predictor of mortality and functional impairment of blunt trauma patients.10–12 The Panel decided to add “including roof” to the intrusion category because the 2006 guidelines did not convey clearly that vertical intrusion has the same implication for increased injury severity as horizontal intrusion.
The Panel recommended transport to a trauma center if any of the following are identified:
-
Falls
-
○ Adults: >20 feet (one story = 10 feet)
-
○ Children: >10 feet or two to three times the height of the child
-
-
High-risk auto crash
-
○ Intrusion, including roof: >12 inches occupant site; >18 inches any site
-
○ Ejection (partial or complete) from automobile
-
○ Death in the same passenger compartment
-
-
Vehicle telemetry data consistent with a high risk for injury
-
Automobile versus pedestrian/bicyclist thrown, run over, or with significant (>20 mph) impact; or
-
Motorcycle crash >20 mph
Step Four: Special Considerations
In Step Four, EMS personnel must determine whether persons who have not met physiologic, anatomic, or mechanism steps have underlying conditions or comorbid factors that place them at higher risk of injury or that aid in identifying the seriously injured patient. Persons who meet Step Four criteria might require trauma center care. In Step Four, the criteria for older adults and anticoagulation were modified, and the criteria for end stage renal disease requiring dialysis and time-sensitive extremity injury were removed.
The “Older adults” criterion was modified to include statements that recognize that a SBP <110 might represent shock after age 65 and that low-impact mechanisms might result in severe injury. The report commented on a retrospective chart review noting an increase in mortality of geriatric patients (aged ≥65 years) presenting to a Level I trauma center with SBP <110mmHg as well as a study finding that occult hypotension being present in 42% of patients with “normal” vital signs.13–14 In addition, the Panel reviewed literature that indicated that older adults might be severely injured in low-energy events such as ground level falls. The report cited a study indicating that ground level falls accounted for 34.6% of deaths in patients ≥65 years of age, and another study of 57,302 patients with ground level falls demonstrating higher rates of intracranial injury and in-hospital mortality among adults aged ≥70 years of age.15–16 The changes made to Step Four regarding older adults reflects the Panels view on strengthening the criteria in the context of the latest literature.
After review of the literature, the Panel also elected to strengthen the “anticoagulation and bleeding disorders” criterion, underscoring the potential for anticoagulated patients who do not meet any of the previous criteria but who have evidence of head injury that may undergo rapid decompensation and deterioration. The modification was the addition of the statement “patients with head injury are at high risk for rapid deterioration.” The report noted that patients who meet this criterion should be transported preferentially to a hospital capable of rapid evaluation and imaging of these patients and initiation of reversal of anticoagulation if necessary.
The Panel elected to remove the “end-stage renal disease requiring dialysis” criterion, noting that research demonstrating the value of dialysis as a triage criterion for identifying patients with serious injury is lacking, and that concerns regarding anticoagulation in this population are addressed under the anticoagulation and bleeding disorders criterion. The “time-sensitive extremity injury” criterion was also removed. With the addition of “pulseless” of Step Two criteria, the Panel felt this criterion to be redundant, and removed it from the 2011 guidelines.
The Panel recommended transport to a trauma center or hospital capable of timely and thorough evaluation and initial management of potentially serious injuries for patients who meet the following criteria:
-
Older adults
-
○ Risk for injury/death increases after age 55 years
-
○ SBP <110 might represent shock after age 65 years
-
○ Low impact mechanisms (e.g., ground-level falls) might result in severe injury
-
-
Children
-
○ Should be triaged preferentially to pediatric capable trauma centers
-
-
Anticoagulants and bleeding disorders
-
○ Patients with head injury are at high risk for rapid deterioration
-
-
Burns
-
○ Without other trauma mechanism: triage to burn facility
-
○ With trauma mechanism: triage to trauma center
-
-
Pregnancy >20 weeks
-
EMS provider judgment
COMMENTARY
Trauma and injury play a significant role in the burden of disease on the population. As the CDC reports, injury is the leading cause of death for persons aged 1–44 years in the U.S., with approximately 30 million injuries resulting in an ED visit annually. In 2008, injuries accounted for approximately 181,226 deaths in the U.S.5 With 1 American dying approximately every three minutes, the disease burden of trauma and injury in the U.S. is one that cannot be ignored. Efforts to address this issue must come from collaborative efforts from health care providers, public health personnel, policy makers, administrators, automotive industry personnel, law enforcement, healthcare related agencies, and the public. These communities must utilize the available research pertaining to trauma and injury related morbidity and mortality to affect change at the policy level.
Research has demonstrated the benefit that regionalized trauma centers provide those individuals suffering an injury. The National Study on the Costs of Outcomes of Trauma identified a 25% relative risk reduction in mortality for severely injured adult patients who received care at a Level I trauma center rather that at a nontrauma center.6 Similarly, a retrospective cohort study of 11,398 severely injured adult patients who survived to hospital admission in Ontario, Canada, indicated that mortality was significantly higher in patients initially undertriaged to nontrauma centers (odds ratio [OR] = 1.24; 95% confidence interval [CI] = 1.10 – 1.40).17 Studies by Gervin et al and Ivatury et al found that rapid transport to a trauma center for patients sustaining penetrating injuries was associated with increased survival.18–19 Gervin et al found that patients with potentially salvageable injuries had a survival rate of 38%. In this group, a salvage rate of 80% was achieved if transport delays were minimized, as compared to a zero percent salvage rate in patients with prolonged prehospital delay. Similarly, Ivatury et al found a zero percent survival rate in those patients receiving penetrating thoracic injuries who were not immediately transported to the hospital. Many other studies have demonstrated a survival benefit of treating seriously injured patients in trauma centers, suggesting that the time lost when bypassing nontrauma centers is recouped by the benefits of receiving care at trauma centers.20–23
With the significant burden of disease that trauma and injury have on the U.S. population, along with the myriad of studies demonstrating the hospital-based beneficial effect trauma centers have on survival, a major strategy to decrease the morbidity and mortality of injured patients is to care for them at the appropriate health care facility. The concept of field triage addresses this issue specifically. At the individual level, EMS providers are tasked with the initial evaluation and treatment of injured patients. One of the critical decisions they must make is whether the patient has suffered an injury that would be best managed at a trauma center. At the population level, EMS providers make decisions that could potentially decrease injury related mortality by up to 25%. It is this fact that makes field triage resources so vitally important to the population, and also one of the major reasons the CDC has committed resources to disseminating the Guidelines for Field Triage of Injured Patients.
Since 2009, the CDC has undertaken an effort to ensure dissemination, implementation, and evaluation of the Guidelines including the development of training guides, educational material, and resources for EMS providers.1 The 2009 report was reprinted in its entirety in the Journal of Emergency Medical Services, and reproduced in multiple textbooks targeting the EMS, emergency medicine, and trauma care community.1 In 2010, the national Association of EMS Physicians (NAEMSP) and ACS-COT issued a joint position paper recommending adoption of the Guidelines for local trauma and EMS systems.24 The National Registry of Emergency Medical Technicians (NREMT) adopted the Guidelines as a standard upon which all certification examination test items relating to patient disposition will be based. The efforts of the CDC to disseminate the field triage criteria as well as the widespread acceptance and implementation of the Guidelines reflect the collective value that many health care organizations, affiliates, and providers place on decreasing trauma and injury related morbidity and mortality.
The “Guidelines for Field Triage of Injured Patients” provide a valuable tool to assist health care providers in the management of injured patients. Given the heterogeneity of EMS systems, this tool must be utilized to maximize the benefit individual patients receive in the context of the available human and capital resources in their communities. Not all systems are the same and not all patients will fit neatly into one of the specified categories. Indeed the heterogeneity of the patient population and EMS system and structure lends to the difficulty in identifying which risk factors may have an effect on patient outcome. The heterogeneity of health care delivery through the EMS system can in part be explained by its development. The North American EMS system developed precipitously in the early 1970s with significant federal grant support and guidance that defined essential system components; however, that guidance did not include a national organizational model for providing EMS services. That decision was left to local communities, and thus, in contrast with many other countries, local EMS systems in the U.S. vary considerably on how they are organized and financed.25,26 The Guidelines provide the framework for assisting individual EMS systems in providing evidenced based quality care, keeping in mind the local, state, and regional variances on how care is delivered. Accordingly, the Panel recommended that the Guidelines not be referred to as a “national protocol” because using the term “protocol” has an unintended proscriptive inference for the end-user that could restrict local adaptation required for optimal implementation.1
At the physician level, emergency physicians and trauma surgeons play a critical role in the evaluation and management of the injured patient. The ED is the gateway for which practically all patients suffering injury enter the health care system to begin receiving definitive treatments. Emergency physicians manage injured patients at the interface between the prehospital and inpatient setting. Having knowledge of EMS systems operations as well as being the first physician to manage injured patients allows emergency physicians the opportunity to have a substantial impact on patient outcome both at the individual and population level. The “Guidelines for Field Triage of Injured Patient” is a vital resource the emergency medicine physician has to combat the morbidity and mortality associated with trauma and injury in the population.
Footnotes
Supervising Section Editor: Mark I Langdorf, MD, MHPE
Submission history: Submitted October 29, 2012; Revision received January 6, 2013; Accepted January 24, 2013
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2013.1.15981
Address for Correspondence: Bharath Chakravarthy, MD, MPH University of California Irvine, School of Medicine, Department of Emergency Medicine, Irvine, California
Email: bchakrav@uci.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Centers for Disease Control and Prevention (CDC) Guidelines for Field Triage of Injured Patients. Recommendations of the National Expert Panel on Field Triage, 2011. MMWR Morbidity and Mortality Weekly Report. 2012;61(1):1–21.
2. American College of Surgeons Resources for the optimal care of the injured patient. Chicago, IL: American College of Surgeons; 2006. 2006.
3. Centers for Disease Control and Prevention (CDC) Guidelines for Field Triage of Injured Patients. Recommendations of the National Expert Panel on Field Triage, 2009. MMWR Morbidity and Mortality Weekly Report. 2009;58 (No. RR-1)
4. CDC WISQARS: web-based injury statistics query and reporting system. Available atwww.cdc.gov/injury/wisqars/LeadingCauses.html. Accessed October 5, 2012.
5. DCD WISQARS: web-based injury statistics query and reporting system: injury mortality reports, 2008, United States. Available at http://www.cdc.gov/injury/wisqars/fatal.html. Accessed October 5, 2012.
6. Mackenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma center care on mortality. N Engl J Med. 2006;354:366–78. [PubMed]
7. Heis HA, Bani-Hani KE, Elheis MA. Overview of extremity arterial trauma in Jordan. Int Angiol.2008;27:522–8. [PubMed]
8. Borman JB, Aharonson-Daniel L, Savitsky B, et al. Israeli Trauma Group. Unilateral flail chest is seldom a lethal injury. Emerg Med J. 2006;23:903–5. [PMC free article] [PubMed]
9. Bastos R, Calhoon JH, Baisden CE. Flail chest and pulmonary contusion. Semin Thoracic Cardiovasc Surg. 2008;20:39–45.
10. Brown JB, Stassen NA, Bankey PE, et al. Mechanism of injury and special consideration criteria still matter: an evaluation of the National Trauma Triage Protocol. J Trauma. 2011;70:38–44.[PubMed]
11. Haider AH, Chang DC, Haut ER, et al. Mechanis of injury predicts patient mortality and impairment after blunt trauma. J Surg Res. 2009;153:138–42. [PubMed]
12. Newgard C, Zive D, Holmes JF, et al. A multi-site assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213(6):709–21. [PMC free article] [PubMed]
13. Heffernan DS, Thakkar RK, Monaghan SF, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Truama. 2010;69(4):813–20.
14. Martin JT, Alkhoury F, O’Connor JA, et al. “Normal” vital signs belie occult hypoperfusion in geriatric trauma patients. Am Surg. 2010;76:65–9. [PubMed]
15. Chisholm KM, Harruff RC. Elderly deaths due to ground-level falls. Am J Forensic Med Pathol.2010;31:350–4. [PubMed]
16. Spaniolas K, Cheng JD, Gestring ML, Sangosanya A, Stassen NA, Bankey PE. Ground level falls are associated with significant mortality in elderly patients. J Trauma. 2010;69:821–5. [PubMed]
17. Haas B, Gomez D, Zagorski B, et al. Survival of the fittest: the hidden cost of undertriage of major trauma. J Am Coll Surg. 2010;211:804–11. [PubMed]
18. Gervin AS, Fishers RP. The importance of prompt transport in salvage of patients with penetrating heart wounds. J Trauma. 1982;22:443–8. [PubMed]
19. Ivatury RR, Nallathambi MN, Roberge RJ, et al. Penetrating thoracic injuries: in-field stabilization vs. prompt transport. J Trauma. 1987;29:1066–73. [PubMed]
20. Mullins Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–24. [PubMed]
21. Mullins RJ, Mann NC, Hedges JR, et al. Preferential benefit of implementation of a statewide trauma system in one of two adjacent states. J Trauma. 1998;44:609–17. [PubMed]
22. Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40:536–45. [PubMed]
23. Demetriades D, Martin M, Salim A, Rhee P, et al. The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg. 2005;242:512–19.[PMC free article] [PubMed]
24. National Association of EMS Physicians Field triage of the injured patient. Available atwww.naemsp.org/documents/FieldTriageoftheInjuredPatient.pdf Accessed October 5, 2012.
25. Boyd DR. The history of emergency medical services in the United States of America. In: Boyd DR, Edlich RF, Micik S, editors. Systems Approach to Emergency Medical Care. Norwalk, Conn: Appleton-Century-Crofts; 1983.
26. Overton J, Stout J. System design. In: National Association of EMS Physicians, editor. Prehospital Systems and Medical Oversight. Dubuque, Iowa: Kendall/Hunt; 2002.