| Author | Affiliation |
|---|---|
| Nicholas D. Caputo, MD, MSc | Lincoln Medical and Mental Health Center, Department of Emergency Medicine, Bronx, New York |
| Christopher P. Shields, MD | Lincoln Medical and Mental Health Center, Department of Emergency Medicine, Bronx, New York |
| Cesar Ochoa, MD | Lincoln Medical and Mental Health Center, Department of Emergency Medicine, Bronx, New York |
| Jennifer Matarlo, RN | Lincoln Medical and Mental Health Center, Department of Surgery, Division of Trauma Surgery, Bronx, New York |
| Mark Leber, MD | Lincoln Medical and Mental Health Center, Department of Emergency Medicine, Bronx, New York |
| Robert Madlinger, DO | Lincoln Medical and Mental Health Center, Department of Surgery, Division of Trauma Surgery, Bronx, New York |
| Muhammed Waseem, MD | Lincoln Medical and Mental Health Center, Department of Emergency Medicine, Bronx, New York |
ABSTRACT
Introduction:
Accidents and assaults (homicides) are the leading causes of death among the youth of the United States, accounting for 53.3% of deaths among children aged 1 to19 years. Victim recidivism, defined as repeated visits to the emergency department (ED) as a victim of violent trauma, is a significantly growing public health problem. As 5-year mortality rates for recidivism are as high as 20%, it is important to determine whether victims with a history of violent trauma are at increased risk for fatal outcome with their next trauma. We hypothesized that victims of violent trauma who have had 1 prior ED visit for violent trauma will have increased odds of fatal outcome.
Methods:
A retrospective chart review was conducted for patients presenting with penetrating trauma to the ED from January 1, 1999 to December 31, 2009. All patients between the ages of 15 to 25 years who presented to the ED for any penetrating trauma were included. Patients with prior presentations for penetrating trauma were compared to those patients who were first-time presenters to determine the odds ratio of fatal outcome.
Results:
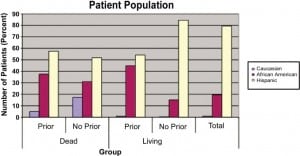
Overall, 15,395 patients were treated for traumatic presentations. Of these, 1,044 met inclusion criteria. Demographically, 79.4% were Hispanic, 19.4% were African American, and 0.96% were Caucasian. The average age was 21 years, and 98% of the population was male. One hundred and forty-seven (14%) had prior presentations, and 897 (86%) did not. Forty of the 147 patients (27%) with prior presentations had a fatal outcome as compared to 29 patients of the 868 (3%) without prior presentations, with odds ratio of 10.8 (95% confidence interval, 6.4–18.1; Pearson χ2, P < 0.001). The 5-year mortality rate for those patients with fatal outcomes was calculated at 16.5%.
Conclusion:
Patients who had prior ED visits for penetrating trauma were at greater risk for fatal outcomes compared to those with no prior visits. Therefore, trauma-related ED visits might offer an opportunity for education and intervention. This may help to prevent future fatalities.
INTRODUCTION
Accidents (unintentional injury) and assaults (homicides) are the leading causes of death among the youth of the United States.1,2 Together, they account for 53.3% of deaths among children aged 1 to 19 years. Of these, assaults, whether penetrating or blunt, account for 10.9% of all deaths. Penetrating injuries account for up to 20% of all pediatric trauma admissions. Homicides are the second leading cause of death among people aged 15 to 24 years, responsible for 5,284 deaths (12.4/100,000).3 Youth violence is a significant and growing public health problem, especially in urban areas.4,5 Gunshot wounds are responsible for the overwhelming majority of penetrating traumatic injuries and have a high mortality rate.1,6 Neighborhood factors that affect youth violence include employment opportunities, local businesses, trash management, vacant housing, street lighting, gang prominence, and the illicit drug market.7 Other risk factors for the incidence of violent traumatic death include socioeconomic status, race, and place of residence (rural vs urban).1,8–12 Although these factors may not be modifiable in the acute setting, explaining the consequences of behavior leading to these presentations may stave off future visits. Emergency medicine physicians are frequently at the forefront of the problem, treating young victims of violent crimes. Studies have shown that violence and injury prevention programs can be successful at educating at-risk youths.13,14 With 5-year mortality rates for recidivism (>2 prior presentations) as high as 20%,15 it is important to determine whether or not victims of violent trauma are at increased risk for fatal outcomes with only a single prior presentation. These patients may have only 1 opportunity for intervention to help change their behavior and break the cycle putting them at risk. The primary objective of this study was to determine the odds of a fatal outcome for patients with violent trauma and with a single prior presentation of the same. In addition, we sought to determine the 5-year mortality rate of these patients. We hypothesize that victims of violent trauma who have 1 prior visit for violent trauma will have increased odds of a fatal outcome. Secondly, we hypothesize that the 5-year mortality rate will be as high as the national average for all patients with violent trauma.
METHODS
We conducted a retrospective chart review for patients presenting with penetrating trauma to the emergency department (ED) of an inner city hospital. We reviewed the medical records from January 1, 1999 to December 31, 2009. Three separate abstractors (research assistants in the department of emergency medicine) were assigned to review the charts of any patient presenting for penetrating trauma, which are catalogued in the New York State Trauma Registry (NYSTR). The abstractors were trained with practice cases (10 each) of patients outside the study age range. They were blinded to the hypotheses of the study. All 3 abstractors used a standardized form to collect information about penetrating trauma, defined as any gunshot or stab wound not self-inflicted, as coded in the medical record. The abstractors did not review the same cases, as time did not permit for the number of cases being reviewed. The study was conducted at an urban, 347-bed level 1 trauma center, which serves about 155,000 patients in the ED annually. This study was approved by the institutional review board.
Inclusion criteria for this study were patients between the ages of 15 and 25 years who presented to the ED for any penetrating trauma, defined as gunshot or stab wound. Patients who were dead on arrival were included in this study. Patients were excluded if penetrating trauma was self-inflicted.
A list of patient medical record numbers was generated from the NYSTR by using International Classification of Diseases, 9th Revision codes for gunshot and stab wounds. From this list, the electronic records of these patients were obtained. The patient’s problem list was then accessed to determine whether or not the patient had presented to our institution in the past for a prior penetrating trauma. Fatal outcomes were determined by electronic death note records. Demographic information was obtained, which included age, gender, ethnicity, and zip code, from the registration information of each patient. Type of injury and location of injury were also recorded. It was not possible to obtain data on patients from other institutions or facilities to determine if patients had had prior visits, as these data were not readily available.
Statistical analyses were performed with the SPSS (IBM, New York, New York) statistical computer software package. Risks of fatal outcome for patients with prior presentations for penetrating trauma were compared to those of patients who were first-time presenters to determine the odds ratio, with statistical significance set at the P < 0.05 level. Patient demographics were presented as mean data (± standard deviation). To calculate the difference in occurrence of prior stab wounds and gunshot wounds between the groups, z values were determined. The 5-year mortality rate was calculated by determining the number of patients with prior trauma who had died within 5 years of their original episode and dividing this number by all patients with prior trauma visits, both living and dead [5-year mortality rate = prior dead within 5 years/(all prior dead + prior living) × 100].
RESULTS
During the study period, 15,395 patients were treated for traumatic presentations. Of these, 1,044 patients met the inclusion criteria set forth (age, penetrating injury, etc). This represents 6.78% of the total population sampled. The sample was then further divided into those patients with prior traumatic presentations (147 patients, 14% of population meeting inclusion criteria), and those without such prior presentations (897, 86%). The Table demonstrates the basic demographics of these 2 groups. Our population is mostly composed of Hispanics (829, 79%), followed by African Americans (203, 19%) and Caucasians (11, 1%).
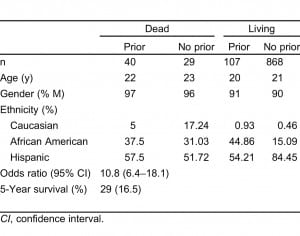
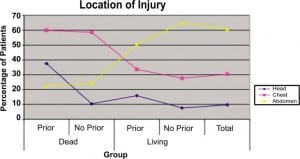
Forty of the 147 patients (27%) with prior presentations had a fatal outcome compared to 29 patients of the 868 (3%) without prior presentations. This led to a calculated odds ratio of 10.8 with 95% confidence interval (CI) of 6.4 to 18.1, P < 0.001 when tested with Pearson χ2. This indicates that patients with 1 prior presentation for penetrating trauma had greater odds of having a fatal outcome than those who did not have any prior visits. The 5-year mortality rate for those patients with fatal outcomes was calculated at 16.5%. Overall, 82% of prior presentations were for stab wounds, while only 18% of patients had previously been shot. Patients with prior visits and fatal outcomes had a higher rate of previous gunshot wounds (22.5%) versus stab wounds (77.5%), while patients with prior visits and nonfatal outcomes had a higher rate of stab wounds (84%) versus gunshot wounds (16%). There was no significant difference between the 2 groups when comparing the proportion of prior stab wounds (z value, 0.772; CI, 77.2%) or prior gunshot wounds (z value, 0.606; CI 72.8%). Figure 1 shows the location of injury for patients in each group as well as for the total sample studied. Interestingly, patients were more likely to have a fatal outcome if the injury sustained was to the chest, as opposed to the head or abdomen.
During the course of the study, summer and fall were found to be the busiest seasons for traumatic presentations to the emergency department. These were followed by the winter season, with spring being the least busy time of year. Figure 2 demonstrates the monthly breakdown of visits as an average of the 10-year period. Finally, traumatic presentations were seen more commonly at night (defined as 8pm–8 am) when compared to the day (defined as 8 am–8 pm), with a rate of 71% for violent trauma occurring at night.
DISCUSSION
This study demonstrates that the last 10 years have seen a continued increase in the risk for violent trauma recurrence and that interventions should be implemented by public health organizations to evaluate whether the problem can be combated. Although the 14% rate of recidivism in our study is lower than the 18% to 21% rate demonstrated by other recent studies, it nevertheless indicates a failure in prevention.12,14 Even more considerable is the substantially increased probability of fatal outcome from violent trauma for those young individuals with a history of only 1 prior violent event. Specifically, those with a history of a single prior visit to the ED for violent penetrating trauma were more at risk (odds ratio of 10.8) of death from subsequent violent trauma as compared to those with no prior incidents. The importance of this finding lies in the fact that there may be only a single opportunity for intervention to help reduce a fatal outcome in this vulnerable population. This argument is further supported by our finding of a 5-year mortality rate of 16.5%, highlighting the grave problem that persists despite a reduction in the 5-year mortality, from a rate of 20%, in the last 2 decades.3
In our study, victims of violent trauma were almost uniformly of male gender more often than not (98%). This is consistent with prior studies wherein males were found to be the victims of violent trauma 64% to 85% of the time.14,16,17,20 Distribution of ethnicity, although consistent with the increased number of minority subjects, was weighed more heavily toward Hispanics in our study, representing 79% of sample subjects. This sample distribution not only reliably represents the demographics of the area surrounding our trauma center but also may indicate a shift in susceptible minority groups.
Racial and socioeconomic parameters including urban setting, low income, unemployment, and access to firearms have been associated with increased violence and death risk.12,14 Although lower socioeconomic status was not formally evaluated in this study as a potential risk factor for death from violent trauma, it may yet play a role. Information obtained from the US Census Bureau indicates that the population percentage below the poverty level in the Bronx is 27% as compared to 13.8% in New York State and 12.6% in the United States.18 This suggests that our population suffers from low socioeconomic status, with the risk factors for violence associated with such status (unemployment, gang violence, fewer educational opportunities, etc). Although most of these previously described risk factors cannot be modified, others, such as access to firearms, avoidance of higher-risk situations, and access to care and education, may be improved and result in decreased death rates in this age group. Interestingly, stabbings make up most prior wounds, but subjects with prior gunshot wounds represent most deaths. Consequently, reduction in access to guns may decrease the mortality associated with victim recidivism. This information is especially important in our population, given that deaths from firearms affect minority youth disproportionally both in our sample as well as in others.14,17,19
Temporal associations were identified and they indicated that 77% of violent trauma visits occurred during the summer and fall months, with an overwhelming majority occurring in the late night hours. Although no data were available for further analysis, the increased rates of penetrating trauma during these months may be associated with summer recess periods. Prolonged periods of idleness and loitering in this age group, caused by being out of school or unemployed, have been implicated in increased risk-taking behaviors.12,20,21 Death due to violence has been described as a chronic disease due to recidivism that ultimately can result in death. Several secondary prevention programs have been implemented in major cities including Chicago, Philadelphia, Milwaukee, and Oakland, showing that these programs can reduce future criminal involvement and possibly result in a reduction in death rates.22 Several screening tools, including the FiGHTS screen, have been shown to decrease violent injury and death.18 A study (n = 829) performed by Walton et al23 in Flint, Michigan, showed reduction in violent behavior (risk reduction: intervention, −10.4%; control, +4.7%; relative risk, 0.70; 95% CI, 0.52–0.95) and substance use (risk reduction: intervention, −32.2%; control, −17.7%; odds ratio, 0.56; 95% CI, 0.34–0.91) after a brief intervention in the ED.23 Although the study differed from ours in that the patient population comprised mostly African Americans (55.9%) and patients were only enrolled at a specific time (between 12 pm and 11 pm), the study still demonstrated a considerable risk reduction through short interventions by ED therapists. Presentation to the ED represents a teachable moment for educating about the risk of future death even after a single violent event. Similar programs may prove successful for the population of the South Bronx.
LIMITATIONS
There are 2 limitations to this study. First, this is a single-center study. The patient population was drawn from those patients admitted to the trauma service and entered into the NYSTR. Consequently, any presentations and deaths due to violent trauma occurring outside of our center were not included in our analysis. Also, patients admitted for trauma to our center may have had prior visits to other medical centers, including for prior penetrating trauma. Second, the population demographics also show a shift in the minority group at risk (ie, Hispanics) as compared to prior studies whose populations are mostly composed of African Americans. Our center is also located in the poorest congressional district in the United States. This demographic tendency may not be typical of other areas, and therefore may decrease the generalizability of our findings. Nonetheless, the problem of victim recidivism itself has been shown to be a significant one in almost all major cities, and we believe the effect of ethnicity is relatively minor. Finally, it may stand to reason that patients with prior traumatic injuries may have died at second presentation because they had a lesser physiologic reserve. These patients may have been weaker (ie, physiologically sicker) to begin with because of a prior traumatic injury. This would be an interesting question to examine in future studies.
CONCLUSION
This study demonstrates a significantly higher odds ratio for fatal outcome, following violent penetrating trauma after just 1 prior presentation for the same. This observation may not allow sufficient time to implement long-term prevention programs as those started for patients with multiple prior presentations. It may therefore be beneficial that the emergency medicine physician try and intervene to change the behavioral pattern of these youths. Brief screening tools and ED interventions with victims of violent trauma have been previously evaluated in prospective trials and have shown promising results in decreasing violent injury and death in young people.
Footnotes
Supervising Section Editor: Sean Henderson, MD
Submission history: Submitted April 8, 2011; Revision received April 29, 2011; Accepted June 13, 2011
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.6.6765
Address for Correspondence: Nicholas D. Caputo, MD, MSc,
Lincoln Medical and Mental Health Center, Department of Emergency Medicine, 234 E 149th St, Bronx, NY 10451
Email: ncaputo.md@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding, sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Martin JA, Kung HC, Mathews TJ, et al. Annual summary of vital statistics: 2006. Pediatrics.2008;121:788–801. [PubMed]
2. Wesson DE. Pediatric trauma: pathophysiology, diagnosis, and treatment. New York, NY: Taylor and Francis;; 2006.
3. Xu J, Kochanek KD, Tejada-Vera B. Deaths: preliminary data for 2007. National Vital Statistics Reports. 2009:58.
4. Sims DW, Buivins FA, Obeid FN. Urban trauma: a chronic recurrent disease. J Trauma.1989;29:940–947. [PubMed]
5. Goins WA, Thompson J, Simpkins S. Recurrent intentional injury. J Natl Med Assoc. 1992;84:431–435. [PMC free article] [PubMed]
6. Cotton BA, Nance ML. Penetrating trauma in children. Semin Pediatr Surg. 2004;13:87–97.[PubMed]
7. Yonas MA, O’Campo P, Burke JG, et al. Neighborhood-level factors and youth violence: giving voice to the perceptions of prominent neighborhood individuals. Health Educ Behav. 2007;34:669–685.[PubMed]
8. Claassen CA, Larkin GL, Hodges G, et al. Criminal correlates of injury-related emergency department recidivism. J Emerg Med. 2007;32:141–147. [PubMed]
9. Caufeild J, Singhal A, Moulton R, et al. Trauma recidivism in a large urban Canadian population. J Trauma. 2004;57:872–876. [PubMed]
10. Meuleners LB, Hendrie D, Lee AH. Hospitalizations due to interpersonal violence: a population-based study in Western Australia. Med J Aust. 2008;188:572–575. [PubMed]
11. Madan A, Beech DJ, Drugs Flint L. guns, and kids: the association between substance use and injury caused by interpersonal violence. J Pediatr Surg. 2001;36:440–442. [PubMed]
12. Cunningham RM, Murray R, Walton MA, et al. Prevalence of past year assault among inner-city emergency department patients. Ann Emer Med. 2009;53:814–823.
13. Whiteside LK, Cunningham RM. Youth violence: effective screening and prevention. AMA J Ethics.2009;11:117–123.
14. Lim HJ, McCart M, Davies WH, et al. Risk for repeated emergency department visits for violent injuries in youth firearm victims. Clin Med Trauma Intensive Med. 2009;2:1–7.
15. Cunningham RM, Knox L, Fein J, et al. Before and after the trauma bay: the prevention of violent injury among youth. Ann Emerg Med. 2009;53:490–500. [PubMed]
16. Teplin LA, McClelland GM, Abram KM, et al. Early violent death among delinquent youth: a prospective longitudinal study. Pediatrics. 2005;115:1586–1593. [PMC free article] [PubMed]
17. Cheng TL, Haynie D, Brenner R, et al. Effectiveness of a mentor-implemented, violence prevention intervention for assault-injured youths presenting to the emergency department: results of a randomized trial. Pediatrics. 2008;122:938–946. [PMC free article] [PubMed]
18. US Census Bureau. American Community Survey: Poverty Data 2006–2008
19. Shibru D, Zahnd E, Becker M, et al. Benefits of a hospital-based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205:684–689. [PubMed]
20. Kunkel P, Thomas CJ, Seguin C, et al. A hospital-based violence prevention tour: a collaborative approach to empower youth. J Trauma. 2010;68:289–293. [PubMed]
21. Edens JF, Campbell JS, Weir JM. Youth psychopathy and criminal recidivism: a meta-analysis of the psychopathy checklist measures. Law Hum Behav. 2007;31:53–75. [PubMed]
22. Snider C, Lee J. Youth violence secondary prevention initiatives in emergency departments: a systemic review. CJEM. 2009;11:161–168. [PubMed]
23. Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304:527–535. [PubMed]


