| Author | Affiliation |
|---|---|
| Peter E. Sokolove, MD | University of California Davis, Department of Emergency Medicine, Davis, California |
| Nathan Kuppermann, MD, MPH | University of California Davis, Department of Emergency Medicine, Davis, California University of California Davis, Department of Pediatrics, Davis, California |
| Cheryl W. Vance, MD | University of California Davis, Department of Emergency Medicine, Davis, California University of California Davis, Department of Pediatrics, Davis, California |
| Moon O. Lee, MD, MPH | University of California Davis, Department of Emergency Medicine, Davis, California |
| Beth A. Morris, MPH | University of California Davis, Department of Emergency Medicine, Davis, California |
| James F. Holmes, MD, MPH | University of California Davis, Department of Emergency Medicine, Davis, California |
ABSTRACT
Introduction:
Children with blunt abdominal trauma (BAT) are often hospitalized despite no intervention. We identified factors associated with emergency department (ED) disposition of children with BAT and differing computed tomography (CT) findings.
Methods:
We surveyed pediatric and general emergency physicians (EPs), pediatric and trauma surgeons regarding care of 2 hypothetical asymptomatic patients: a 9-year-old struck by a slow-moving car (Case 1) and an 11-month-old who fell 10 feet (Case 2). We presented various abdominal CT findings and asked physicians about disposition preferences. We evaluated predictors of patient discharge using multivariable regression analysis, adjusting for hospital and ED characteristics, and clinician experience. Pediatric EPs served as the reference group.
Results:
Of 2,003 eligible surveyed, 636 (32%) responded. For normal CTs, 99% would discharge in Case 1 and 88% in Case 2. Prominent specialty differences included: for trace intraperitoneal fluid (TIF), 68% would discharge in Case 1 and 57% in Case 2. Patients with TIF were less likely to be discharged by pediatric surgeons (Case 1: OR 0.52, 95% CI 0.32, 0.82; Case 2: OR 0.49, 95% CI 0.30, 0.79). Patients with renal contusions were less likely to be discharged by pediatric surgeons (Case 1: OR 0.55, 95% CI 0.32, 0.95) and more likely by general EPs (Case 1: OR 1.83, 95% CI 1.25, 2.69; Case 2: OR 2.37, 95% CI 1.14, 4.89).
Conclusion:
Substantial variation exists between specialties in reported hospitalization practices of asymptomatic children after abdominal trauma with minor CT findings. Better evidence is needed to guide disposition decisions.
INTRODUCTION
Intra-abdominal injury (IAI) is a leading cause of morbidity and mortality in children older than 1 year of age. More than 600,000 children with blunt abdominal trauma are evaluated annually in United States (U.S.) emergency departments (EDs), many of whom undergo abdominal imaging. When abdominal imaging is performed after blunt trauma, computed tomography (CT) is the test of choice.1,2 However, IAIs are identified in fewer than 20% of children imaged after blunt abdominal trauma.3
Controversy remains regarding disposition of the child after blunt traumatic injury. It remains unclear whether hospitalization is necessary when a minor IAI has been identified, as relatively few patients with IAIs require acute, specific therapy.4,5 The great majority of children with solid organ injuries are managed non-operatively. For injuries to the liver or spleen, non-operative success rates of 90% to 95% have been reported, and for isolated Grade I or II injuries to the solid organs, surgical interventions or blood transfusions are uncommon.6
To best develop and evaluate clinical decision rules for identifying “clinically important” IAIs for purposes of imaging and patient disposition, one needs to understand how various physician groups currently manage children with minor IAIs after blunt trauma. Furthermore, trauma care is optimized when the care provided is standardized based on scientific evidence.7 Substantial variability in ED disposition of injured patients suggests an area of clinical inefficiency. Our objective was to identify: 1) variation in imaging and disposition decisions among clinicians who care for pediatric trauma patients; and 2) factors associated with disposition decisions of children with blunt abdominal trauma and differing abdominal CT findings. We suspected that substantial variation in practice patterns exists among physicians caring for children with normal abdominal examinations and minor IAIs on CT, and that factors associated with this variation can be identified. Specifically, we hypothesized that as a group, surgeons are more likely to hospitalize these children than are emergency physicians (EPs).
METHODS
Study Design and Population
We conducted a self-administered, electronic and paper mail survey of pediatric EPs, general EPs, pediatric surgeons, and trauma surgeons practicing in all U.S. pediatric Level I and Level II trauma centers, children’s hospitals, and trauma centers with a pediatric commitment between July 2006 and May 2007. We identified these institutions and physicians using information obtained through the American College of Surgeons (ACS), the National Association of Children’s Hospitals and Related Institutions (NACHRI), and from institutional websites of verified ACS and NACHRI members. Surveys were sent to the entire group of physicians identified. The local institutional review committee approved this study.
Survey Content and Administration
In our survey we asked about participants’ demographic characteristics and then presented 2 hypothetical patient scenarios involving children with blunt abdominal trauma: Case 1, a 9-year-old girl struck by a car traveling 10 mph while riding her bicycle with laboratory measurements notable only for an elevated ALT level of 135 U/L; and Case 2, an 11-month-old boy who fell 10 feet from a balcony and landed in dirt with laboratory measurements notable only for microscopic hematuria of 25 rbc/hpf. Both patients were described as being otherwise asymptomatic and having normal abdominal examinations after 4 hours of ED observation. Survey participants were asked whether they would be willing to discharge the patients home to reliable parents with good follow up given any of the following 8 isolated abdominal CT findings: normal CT, trace intraperitoneal fluid, small splenic contusion, Grade 1 subcapsular splenic hematoma, small liver contusion, Grade 1 subcapsular liver hematoma, intraparenchymal liver hematoma, and Grade 1 renal contusion.
Survey participants then were asked 2 general questions to assess their opinions regarding the diagnosis and management of children with blunt abdominal trauma: 1) “Should every child with a traumatic intra-abdominal injury identified by CT, no matter how small, be hospitalized even if no acute intervention is needed?” and 2) “Would you accept not identifying a traumatic intra-abdominal injury that would have appeared on CT (if a CT were obtained) in a well-appearing, verbal child if no acute intervention was necessary (e.g. blood transfusion, therapeutic embolization, laparotomy, or IV fluids)?”.
Participants initially were contacted by electronic mail in July 2006. They were invited to participate in the web-based survey and given a hypertext link to access the questionnaire. Physicians with undeliverable e-mail addresses were sent the survey via U.S. Postal Service. In September 2006, physicians who had not responded to the initial e-mail survey were sent a second e-mail request to participate, but with the survey attached as an electronic PDF document. In December 2006, we sent a cover letter and survey by mail to physicians who had not responded to either e-mail survey. In February 2007, we sent a final paper mailing to all remaining non-responders.
Data Analysis
We entered data into a Microsoft Access database (Microsoft Corp., Redmond, WA) and analyzed it using Stata/SE 8.2 for Windows (Version 8. StataCorp LP, College Station, TX). We used simple univariate statistics to analyze demographic variables and used Holm’s correction for Bonferroni multiple test procedure to conduct post hoc testing.8 Since there were so few surveys returned from practitioners in the “other” practice specialty group, these were removed from further analysis. We used the chi-square test to determine the association between practice specialty and patient disposition. We then performed backward stepwise logistic regression to examine the impact of physician characteristics (practice specialty, years in practice, and percentage of patients who are children) and hospital characteristics (annual ED pediatric patient volume, practice setting, and geographic location) on disposition decisions for the hypothetical patients with different abdominal CT findings. Reference groups for the analysis were pediatric emergency medicine specialty, > 15 years of clinical practice experience, pediatric ED volume of > 60,000 visits per year, and practices with > 95% pediatric patients. We selected these reference groups because (except for ED volume) they were the most populous of the subgroups. Finally, we performed standard multivariable logistic regression to determine differences between practice specialties for the general opinion questions regarding the diagnosis and management of children with blunt abdominal trauma, adjusting for years in practice, percentage of patients who are children, annual ED pediatric volume, practice setting, and geographic location. Results are presented with odds ratios (OR) with 95% confidence intervals (CI).
RESULTS
We distributed 2,395 surveys, of which 314 were undeliverable. Seventy-seven respondents did not care for patients younger than 18 years with trauma, and one was a nurse practitioner, giving a total of 78 respondents that were ineligible to participate in the survey analysis. Of the remaining 2,003 eligible participants, 636 (32%) responded to the survey. Practice specialty response rates were pediatric emergency medicine 336/878 (38%), general emergency medicine 161/645 (25%), pediatric surgery 76/387 (20%), and trauma surgery 48/93 (52%).
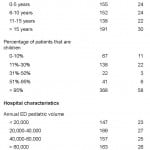
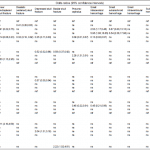
Physician and hospital characteristics of respondents are shown in Table 1. One-half of all participants (53%) specialize in pediatric emergency medicine. Nearly one-third (30%) have more than 15 years of clinical practice experience. More than one-half (58%) almost exclusively care for pediatric patients. While the participants were evenly distributed across the 4 categories representing annual pediatric patient volumes, most identified their practice setting as an academic or a children’s hospital. Most respondents (90%) practice in urban areas.
Table 1. Characteristics of survey respondents.
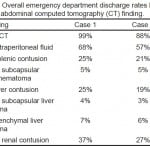
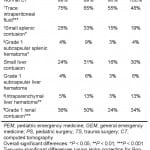
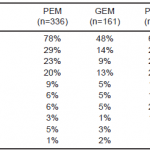
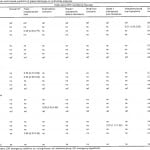
Overall ED discharge rates by CT finding for Cases 1 and 2 are shown in Table 2. Most respondents would discharge the hypothetical patients in both cases when CT findings were normal (Case 1: 99%, Case 2: 88%), although the number who would discharge patients with trace intraperitoneal fluid on their CT was substantially lower (Case 1: 68%, Case 2: 57%). Approximately one-fourth to one-third would discharge patients with a small splenic contusion (Case 1: 25%, Case 2: 21%), a small liver contusion (Case 1: 25%, Case 2: 19%), or a Grade 1 renal contusion (Case 1: 37%, Case 2: 27%). Few would discharge patients with a Grade 1 subcapsular splenic hematoma (Case 1: 5%, Case 2: 5%), a Grade 1 subcapsular liver hematoma (Case 1: 4%, Case 2: 3%), or an intraparenchymal liver hematoma (Case 1: 7%, Case 2: 6%). ED discharge rates of each practice specialty for the various isolated CT findings are reported in Tables 3 and and4,4, for Cases 1 and 2 respectively.
Table 2. Overall emergency department discharge rates by isolated abdominal computed tomography (CT) finding.
Table 3. Case 1 emergency department discharge rates by practice specialty.
Table 4. Case 2 emergency department discharge rates by practice specialty.
PEM, pediatric emergency medicine; GEM, general emergency medicine; PNSG, pediatric neurosurgery, GNSG, general neurosurgery; PS, pediatric surgery; TS, trauma surgery
Overall significant differences (by Chi-square test of homogeneity of proportions, with 5 degrees of freedom): *p<0.05; **p<0.01; *** p<0.001
Two-way significant differences (using Holm correction for Bonferroni multiple test procedure):
†PEM v. GEM, PNSG, GNSG, PS, and TS; GEM v. PS; PNSG v. PS
‡PEM v. GEM and PS
§PEM v. GEM and PS; PNSG v. PS; GNSG v. PS
||PEM v. PS; GEM v. PS; PNSG v. PS; GNSG v. PS; PS v. TS
¶PNSG v. PS; GNSG v. PS
††PNSG v. PS; GNSG v. PS and TS
‡‡PEM v. PNSG and GNSG; GEM v. PNSG and GNSG; PNSG v. PS and TS; GNSG v. PS
§§GEM v. GNSG; GNSG v. PS
||||PEM v. PNSG; GEM v. PNSG
Statistically significant results of the multivariable analysis are shown in Tables 5 and and6.6. Patients with trace intraperitoneal fluid were less likely to be discharged by pediatric surgeons (both cases) and trauma surgeons (Case 1). In Case 2, patients with trace intraperitoneal fluid were also less likely to be discharged by physicians seeing fewer than 30% children in their practices or by those practicing at an academic hospital.
Table 5. Case 1 physician and hospital predictors of patient discharge on multivariate analysis.
EM, emergency medicine; ns, not significant; ref, reference group
Table 6. Case 2 physician and hospital predictors of patient discharge on multivariate analysis.
EM, emergency medicine; ns, not significant; ref, reference group
Patients with renal contusions were less likely to be discharged by pediatric surgeons (Case 1), physicians in practice < 10 years (both cases), physicians seeing fewer than 30% children in their practices (Case 2), or physicians practicing at an academic hospital (both cases). Patients with renal contusions were more likely to be discharged by general EPs (both cases).
Patients with intraparenchymal liver hematomas were more likely to be discharged by general EPs (both cases) and trauma surgeons (Case 1).
There were other differences between physician specialty groups regarding ED discharge of patients with various injuries. For example, general EPs were more likely to discharge patients with mall splenic contusions (Case 1), while pediatric surgeons were less likely to discharge patients with small liver contusions (Case 1).
For the 2 general opinion questions, 44% (range across specialties 37% – 61%) of participants answered that every child with a traumatic IAI identified by CT, no matter how small, should be hospitalized even if no acute intervention is needed; 74% (range across specialties 53% – 78%) would accept not identifying a traumatic IAI that would have appeared on a CT (if a CT were obtained) in a well appearing, verbal child if no acute intervention was necessary (Table 7). For both questions, pediatric surgeons and trauma surgeons gave the most conservative answers (i.e. were more likely to hospitalize patients and less likely to accept missing CT findings). On multivariate analysis, pediatric surgeons were more likely to believe that children with IAI should always be hospitalized (OR 2.21, 95% CI 1.33, 3.68), and they were less willing to accept not identifying all IAI on CT (OR 0.53, 95% CI 0.30, 0.93).
DISCUSSION
In our survey we found substantial variation between specialties in reported hospitalization practices of children after blunt abdominal trauma. We also found a number of areas of agreement. In both hypothetical cases, almost all physicians surveyed were willing to discharge patients given normal abdominal CTs. While abdominal CT is not perfectly sensitive for IAI, particularly pancreatic injuries, such injuries are unlikely in patients with normal CTs, normal mental status, and non-tender abdominal examinations.3, 9–12 In a meta-analysis of nearly 2,600 pediatric blunt trauma patients, the prevalence of IAI after a normal abdominal CT was 0.19% and the negative predictive value of a normal abdominal CT was 99.8%.13
Across all specialties, respondents were less likely to discharge an infant with a normal CT (Case 2: 11-monthold who fell 10 feet) than an older child with a normal CT (Case 1: 9-year-old struck by a car). Possible reasons for this difference include that physicians may have less familiarity with evaluating younger children or may practice more conservatively in preverbal children, where the physical examination may be less reliable. In addition, although the survey instructed that there was no concern for physical abuse in these cases, respondents may have had lingering concerns nonetheless.
In both cases, although the majority of physicians were willing to discharge patients with isolated trace intraperitoneal fluid on CT, a substantial percentage would hospitalize such patients. In Case 2, physicians who see fewer than 30% children in their practices were less willing to discharge patients with isolated trace intraperitoneal fluid on CT. It is not surprising that physicians who treat smaller proportions of children are more conservative in their hospitalization practices, as they may feel uncomfortable even with a minor finding on CT that rarely requires an intervention. In one study, isolated intraperitoneal fluid was seen in 14% of hospitalized pediatric patients following blunt abdominal trauma.14 Of the 94 study patients, 91 (97%) did not require an intervention during hospitalization, while 3 patients developed peritonitis within 12–14 hours of observation. Of note, all 3 had external signs of abdominal trauma and had tenderness on initial abdominal examination. This is consistent with a previous study of children with blunt trauma, in which an IAI was identified in 7/42 (17%) patients with isolated intraperitoneal fluid, all of whom had either abdominal tenderness or a decreased level of consciousness.15
Few physicians surveyed in our study would discharge patients with Grade 1 subcapsular splenic hematomas, Grade 1 subcapsular liver hematomas, or intraparenchymal liver hematomas. While general EPs and, in Case 1, trauma surgeons were more likely to discharge patients with intraparenchymal liver hematomas, the vast majority of both groups would still admit children with such injuries. Thus, there appears to be a consensus among these various specialist groups that patients with such injuries warrant hospitalization.
Patients with isolated Grade 1 renal contusions were less likely to be discharged by physicians with less than 10 years of practice experience or practicing at an academic hospital. Such patients were also less likely to be discharged by physicians who see fewer than 30% children in Case 2 and by pediatric surgeons in Case 1. In contrast, such patients were more likely to be discharged by general EPs, and in Case 2, by physicians practicing at a general hospital. It is not surprising that adult practitioners appear to have less concern about renal contusions, as much of the trauma literature discourages evaluation of microscopic hematuria in normotensive, adult blunt trauma patients and there is general acknowledgment that renal contusions will be missed.16–22 Renal contusions rarely require intervention and have been reported to not result in subsequent renal parenchymal scarring on follow-up CT.23 In a study of adults with renal injuries, hematomas or contusions were managed non-operatively in 99% of cases, and a more recent study of children with blunt trauma reported that none of the children with Grade 1 renal injuries required surgical intervention.24,25 While pediatric surgeons may be more conservative as a group, 1 out of 5 would discharge patients with isolated Grade 1 renal contusions.
Ideally, physicians should limit the use of abdominal CT in children to avoid the associated risks from radiation exposure as up to 2% of all cancers in the U.S. may be attributed to CT use.26 The risk of fatal malignancy from a single abdominal CT is estimated to range from 1/700 – 1/1400, and the risk increases as patient age at time of exposure decreases.26 While most pediatric and trauma surgeons were willing to accept not identifying injuries when no acute intervention is necessary and no suspicion for abuse exists, they were less willing to do so than pediatric EPs. The reasons for this difference are unclear, but this finding has implications for the implementation of selective imaging protocols, as some groups are likely to be less accepting than others. Overall, 74% of survey respondents were willing to accept not identifying injuries when no acute intervention is necessary and no suspicion for abuse exists, giving hope that successful implementation of validated predictions rules may result in change of clinical practice.
Overall, while we found some areas of agreement, substantial variability exists between specialties in their reported hospitalization practices of children after blunt abdominal trauma. This variation in practice is likely a marker of clinical inefficiency and opportunity for improvement in quality of care. Furthermore, this variability in physician practice patterns may limit full acceptance of selective abdominal CT imaging without further generation of evidence-based guidelines, as well as education and discussions, both within and between various practice specialty groups. Future work to generate evidence-based guidelines for obtaining CTs on children with abdominal trauma, and hospitalization of children with minor IAIs is needed.
LIMITATIONS
This study has several limitations. We achieved a response rate of 32%, and it is unclear if the reported practice patterns of non-responders might differ from those who responded to the survey. This may have limited the power to detect significant differences between specialties in some of our analyses. Nonetheless, we found important and significant variation between specialties among survey responders. Physicians were asked to respond to 2 hypothetical cases, and their responses on a survey may or may not accurately reflect their actual clinical practice when caring for children with blunt abdominal trauma.
We surveyed physicians practicing at major pediatric trauma centers and children’s hospitals. Thus, our study results may not reflect the full spectrum of physician practice patterns in all clinical settings. However, the physicians we surveyed are those most likely to manage children with substantial injury mechanisms and likely have the most experience in management and with outcomes of such children. Finally, we did not assess the reasons that respondents decided to discharge or admit patients, so we are unable to determine what were the exact concerns driving the decision-making.
CONCLUSION
Substantial variation exists among specialties in reported hospitalization practices of clinically-asymptomatic children after blunt abdominal trauma and with minor traumatic abdominal CT findings. Pediatric surgeons and those seeing fewer than 30% children in their practices are less likely to discharge patients from the ED, and general EPs are more likely to discharge patients from the ED. Better evidence is needed to guide disposition decision-making in asymptomatic patients with normal abdominal examinations and various intra-abdominal injuries on CT after blunt abdominal trauma.
Footnotes
Supervising Section Editor: Judith Klein, MD
Submission history: Submitted October 9, 2011; Revision received February 16, 2012; Accepted March 27, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.3.6911
Address for Correspondence: Peter E. Sokolove MD, University of California Davis Medical Center, Department of Emergency Medicine, 4150 V street, Sacramento, CA
Email: pesokolove@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001 Feb;176(2):289–96. [PubMed]
2. Jindal A, Velmahos GC, Rofougaran R. Computed tomography for evaluation of mild to moderate pediatric trauma: are we overusing it? World J Surg. 2002 Jan;26(1):13–16. [PubMed]
3. Awasthi S, Mao A, Wooton-Gorges SL, et al. Is hospital admission and observation required after a normal abdominal computed tomography scan in children with blunt abdominal trauma? Acad Emerg Med. 2008 Oct;15(10):895–9. Epub 2008 Sep 5. [PubMed]
4. Holmes JF, Sokolove PE, Brant WE, et al. Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med. 2002 May;39(5):500–9. [PubMed]
5. Isaacman DJ, Scarfone RJ, Kost SI, et al. Utility of routine laboratory testing for detecting intra-abdominal injury in the pediatric trauma patient. Pediatrics. 1993 Nov;92(5):691–4. [PubMed]
6. Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma.2009 Aug;67(2):S135–9. [PubMed]
7. American College of Surgeons Committee on Trauma Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons Committee on Trauma; 2006. 2006.
8. Holm S. A simple sequentially rejective multiple test procedure. Scand J Statist. 1979;6(2):65–70.
9. Ford EG, Senac MO., Jr Clinical presentation and radiographic identification of small bowel rupture following blunt trauma in children. Pediatr Emerg Care. 1993;9:139–42. [PubMed]
10. Moss RL, Musemeche CA. Clinical judgment is superior to diagnostic tests in the management of pediatric small bowel injury. J Pediatr Surg. 1996;31:1178–81. [PubMed]
11. Sivit CJ, Taylor GA, Newman KD, et al. Safety-belt injuries in children with lap-belt ecchymosis:CT findings in 61 patients. AJR Am J Roentgenol. 1991;157:111–14. [PubMed]
12. Phelan HA, Velmahos GC, Jurkovich GJ, et al. An evaluation of multidetector computed tomography in detecting pancreatic injury: results of a multicenter AAST study. J Trauma.2009;66(3):641–6. [PubMed]
13. Hom J. The risk of intra-abdominal injuries in pediatric patients with stable blunt abdominal trauma and negative abdominal computed tomography. Ann Emerg Med. 2010;17(5):469–75.
14. Christiano JG, Tummers M, Kennedy A. Clinical significance of isolated intraperitoneal fluid on computed tomography in pediatric blunt abdominal trauma. J Pediatr Surg. 2009 Jun;44(6):1242–8.[PubMed]
15. Holmes JF, London KL, Brant WE, et al. Isolated intraperitoneal fluid on abdominal computed tomography in children with blunt trauma. Acad Emerg Med. 2000;7(4):335–41. [PubMed]
16. Cass AS, Luxenberg M, Gleich P, et al. Clinical indications for radiographic evaluation of blunt renal trauma. J Urol. 1986;136:370–1. [PubMed]
17. Eastham JA, Wilson TG, Ahlering TE. Radiographic evaluation of adult patients with blunt renal trauma. J Urol. 1992;148:266–7. [PubMed]
18. Guice K, Oldham K, Eide B, et al. Hematuria after blunt trauma: when is pyelography useful? J Trauma. 1983;23:305–11. [PubMed]
19. Kisa E, Schenk WG., 3rd Indications for emergency intravenous pyelography (IVP) in blunt abdominal trauma: a reappraisal. J Trauma. 1986;26:1086–9. [PubMed]
20. McAndrew JD, Corriere JN., Jr Radiographic evaluation of renal trauma: evaluation of 1103 consecutive patients. Br J Urol. 1994;73:352–4. [PubMed]
21. Mee SL, McAninch JW, Robinson AL, et al. Radiographic assessment of renal trauma: a 10-year prospective study of patient selection. J Urol. 1989;141:1095–8. [PubMed]
22. Nicolaisen GS, McAninch JW, Marshall GA, et al. Renal trauma: re-evaluation of the indications for radiographic assessment. J Urol. 1985;133:183–7. [PubMed]
23. Dunfee BL, Lucey BC, Soto JA. Development of renal scars on CT after abdominal trauma: does grade of injury matter? AJR Am J Roentgenol. 2008;190:1174–9. [PubMed]
24. Wessells H, Suh D, Porter JR, et al. Renal injury and operative management in the United States: results of a population-based study. J Trauma. 2003;54:423–30. [PubMed]
25. Nance ML, Lutz N, Carr MC, et al. Blunt renal injuries in children can be managed nonoperatively: outcome in a consecutive series of patients. J Trauma. 2004;57:474–8. [PubMed]
26. Brenner DJ, Hall EJ. Computed tomography—An increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84. [PubMed]