| Author | Affiliation |
|---|---|
| David R. Vinson, MD | Kaiser Permanente Roseville Medical Center, Department of Emergency Medicine, Roseville, California The Permanente Medical Group, Oakland, California |
| Casey L. Hoehn, BA | Loma Linda University School of Medicine, Loma Linda, California |
ABSTRACT
Introduction:
Much of the emergency medical research on sedation-assisted orthopedic reductions has been undertaken with two physicians––one dedicated to the sedation and one to the procedure. Clinical practice in community emergency departments (EDs), however, often involves only one physician, who both performs the procedure and simultaneously oversees the crendentialed registered nurse who administers the sedation medication and monitors the patient. Although the dual-physician model is advocated by some, evidence in support of its superiority is lacking.
Methods:
In this electronic health records review we describe sedation-assisted closed reductions of major joints and forearm fractures in three suburban community EDs. The type of procedure and sedation medication, need for specialty assistance, success rates, and intervention-requiring adverse events are reported.
Results:
During the 18-month study period, procedural sedation was performed 457 times on 442 patients undergoing closed reduction for shoulder dislocations (n = 111), elbow dislocations (n = 29), hip dislocations (n = 101), and forearm fractures (n = 201). In the vast majority of this cohort (98.4% [435/442]), a single emergency physician simultaneously managed both the procedural sedation and the initial orthopedic reduction without the assistance of a second physician. The reduction was successful or satisfactory in 96.6% (425/435; 95% confidence interval [CI], 95.8–98.8%) of these cases, with a low incidence of intervention-requiring adverse events (2.8% [12/435]; 95% CI, 1.5–4.8%).
Conclusion:
Sedation-assisted closed reduction of major joint dislocations and forearm fractures can be performed effectively and safely in the ED using a one physician/one nurse model. A policy that requires a separate physician (or nurse anesthetist) to administer medications for all sedation-assisted ED procedures appears unwarranted. Further research is needed to determine which specific clinical scenarios might benefit from a dual-physician approach.
INTRODUCTION
In many community emergency departments (ED) a single emergency physician simultaneously performs a complex painful procedure while directing procedural sedation—even deep sedation—administered by a credentialed emergency nurse. Most of the research on emergency procedural sedation, however, has not operated in this context. The study of the safety and efficacy of various sedatives during painful procedures has commonly been undertaken in academic settings with one physician dedicated to the sedation and a second physician dedicated to the procedure. Dual physician arrangements greatly facilitate data collection and have been employed with great success, for example, in propofol research with both prospective observational studies and controlled trials.1–12 Yet many community EDs do not have the resources to staff each sedation with two physicians, especially when experience suggests that a one physician/one nurse combination may well be adequate.
Insufficient research attention, however, has been paid to the study of a single physician managing both parts of the procedural sedation dynamic. No randomized trial has been published comparing the efficacy and safety of a one physician/one nurse model with a two physician/one nurse model. Miner and Krauss,13 in a recent report on the state of the art of procedural sedation in emergency medicine, rank the issue of personnel at the top of their list of areas needing further investigation. They state, “The first question that needs to be addressed is whether emergency physicians can perform the procedure and the sedation simultaneously. Given the nature of emergency medicine, it is important to determine which agents at what levels of sedation can be safely used by a single emergency physician relative to using separate operators for the sedation and the procedure.”
Only a handful of studies have been published that describe the safety and effectiveness of the one physician/one nurse model in emergency medicine procedural sedation. This model has been in operation in our EDs for decades.14,15 We undertook this study to describe the practice patterns of 3 community EDs in performing closed reductions of common orthopedic dislocations and fractures under procedural sedation. The type of procedure, use of sedation medications, need for specialty assistance, procedural success rates, and adverse events requiring intervention are reported.
METHODS
Study Design, Setting, and Population
We conducted this 18-month retrospective health records review between November 2007 and April 2009 in the EDs of 3 affiliated suburban community hospitals that are part of a large integrated healthcare delivery system. The annual censuses for the 3 EDs during the study period ranged from 65,000 to 79,000 patient visits. All are staffed by board-certified (or board-eligible) emergency physicians. Two departments serve as satellite sites for a nearby emergency medicine residency-training program. None was a designated trauma center during the study period. The study was approved by the Kaiser Foundation Research Institute’s Northern California Institutional Review Board.
The patient population consisted of a consecutive series of ED patients who received procedural sedation for reduction of one of the following four orthopedic diagnoses: shoulder dislocation, elbow dislocation, hip dislocation, and forearm fracture. We identified patients who underwent these orthopedic procedures using Current Procedural Terminology codes. The electronic medical record of each of these cases was reviewed for the concomitant use of procedural sedation. The ED patients who underwent their sedation-assisted orthopedic procedure without resident assistance during the study period constitute the study population. Cases that required immediate operative reduction without intervening ED sedation were not identified.
Measurements
The investigators obtained data from an explicit, systematic review of each patient’s electronic medical record. Both abstractors agreed to the content and coding of each data element, procedures for data handling and data transmission, and protocols to handle possible questions or problems during the study. A structured data-abstraction tool was used.
We reviewed all physician and nursing notes from the index ED visit, any accompanying consultant notes, all associated radiology reports, and the immediate follow-up records. Demographic variables included age, sex, and date of ED visit. Orthopedic variables included radiographic and clinical diagnoses, nature of the closed reduction, presence of a prosthetic joint, bedside involvement of an orthopedic surgeon or additional emergency physician, post-procedural radiographic alignment (reduction for dislocations or improved alignment for forearm fractures), reduction complications, post-ED disposition, follow-up arrangements and management. Sedation variables included the American Society of Anesthesiologists Physical Status Classification Scale (ASA score 1–6), primary sedation agent, and adverse events that required intervention, defined a priori by the authors to include the following: oxygen desaturation (<90%) or apnea, airway obstruction, laryngospasm, vomiting, pulmonary aspiration, bradycardia (pulse less than 60 bpm in adults), hypotension (systolic blood pressure less than 90 mmHg in adults), dysrhythmia, and arrest.16,17 Adverse events were recorded as such if they were attended by one of the following interventions: vigorous tactile stimulation, airway repositioning (chin lift, jaw thrust, neck extension, midline repositioning), suctioning, supplemental or increased oxygen delivery, placement of oral or nasal airway, application of positive pressure or ventilation with bag mask, tracheal intubation (laryngeal mask airway or endotracheal tube intubation), administration of reversal agents (flumazenil or naloxone), administration of anti-dysrhythmic agents, and chest compressions. The agent, dose, and effect of pre-procedural analgesia were not abstracted for this study. We identified and excluded from analysis cases with missing or incomplete records.
Procedural Sedation Protocol
Regional procedural sedation guidelines were implemented prior to, and were in effect throughout, the study period. The guidelines mandate the bedside presence of 2 licensed personnel, which in our setting equates to a board-certified (or board-eligible) emergency physician and an emergency nurse specifically trained and certified in procedural sedation. The emergency physician is required to conduct a history and physical examination, including an airway assessment and an ASA score, prior to the procedure to determine the patient’s eligibility for ED procedural sedation. Supplemental oxygen is administered (at least 2L via nasal cannula, though usually 10L with a non-rebreather mask), intravenous access is secured, and age-appropriate resuscitation equipment is placed at the bedside.
Continuous cardiac and transcutaneous oxygen saturation are in place throughout the procedure until complete recovery monitoring also has been achieved. Continuous end-tidal CO2 is recommended. Blood pressure, pulse rate, respiratory rate, cardiac rhythm, oxygen saturation and level of consciousness are measured and documented serially a minimum of every 5 minutes during the procedure, then after the procedure every 15 minutes, for at least 30 minutes, or until vital signs stabilize near pre-sedation levels. The Procedure and Anesthesia Scoring System (PASS) is used to quantify the patient’s overall status and to determine when the patient is safe for discharge. 18 PASS measures include level of consciousness, physical activity, hemodynamic stability, respiration, oxygen saturation, pain, and nausea/vomiting. Our procedural sedation protocol requires a pre-sedation, intra-sedation and post-sedation PASS score. The patient’s discharge PASS score must have returned to their pre-procedure baseline score. All measurements are recorded by the nurse for each procedure on a standardized electronic form integrated into the ED record. The choice and dose of sedative, as well as the use of adjunct medication(s), are at the physician’s discretion.
Data Analysis
Continuous variables are presented as medians with their interquartile range (IQR) (25–75). Categorical data are presented as percent frequency of occurrence. We calculated the 95% confidence intervals (CI) using the modified Wald method. We performed descriptive statistics using standard software (Microsoft® Excel, 2008, version 12.0). Chi-squared analysis was undertaken using STATA 11 software (StataCorp, College Station, Texas). Statistical significance was set at P < 0.05.
RESULTS
During the 18-month study period we identified 1,322 patients in the 3 EDs who underwent closed reduction for a dislocated shoulder, elbow, or hip, or a fractured forearm. Of these, 442 (33.4%) received procedural sedation during their reduction and constitute our study cohort. Patient demographics and characteristics are described in Table 1. No cases were excluded from analysis because of missing or incomplete records.
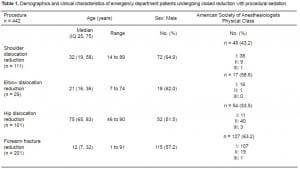
Demographics and clinical characteristics of emergency department patients undergoing closed reduction with procedural sedation.
The 111 shoulder dislocations included 110 anterior dislocations and 1 posterior dislocation. Three of the anterior dislocations were noted to have minor pre-reduction fractures of the humeral head. Only 1 of the 29 elbow dislocations had a concomitant pre-reduction fracture—a small avulsion fracture of the lateral epicondyle. All 101 hip dislocations involved prosthetic hips; none was fractured. The 201 closed forearm fractures included 134 (66.7%) combined radius and ulna fractures, 66 (32.8%) isolated radius fractures and 1 (0.5%) isolated ulna fracture.
Procedural sedation was performed 457 times on 442 patients. The additional 15 rounds of sedation were required for a second reduction attempt when the first one had failed to achieve adequate anatomical results. Five medications were used during these 457 sedations: propofol (303; 66.3%), etomidate (67; 14.7%), ketamine (57; 12.5%), methohexital (17; 3.7%), midazolam alone (13; 2.8%). Midazolam alone was used exclusively for forearm fracture reduction, and ketamine was used exclusively in children.
In the vast majority of this cohort (98.4% [435/442]; 95% CI, 96.7 – 99.3%), a single emergency physician simultaneously managed both the procedural sedation and the initial orthopedic reduction without the assistance of a second physician. The reduction was successful or satisfactory in 96.6% (425/435; 95% CI, 95.8 – 98.8%) of these cases, with a low incidence of intervention-requiring adverse events (2.8% [12/435]; 95% CI, 1.5 – 4.8%). A two physician/one nurse model was employed in select cases in lieu of the one physician/one nurse model for orthopedic reasons (n = 7; 1.6%) and when the one physician/one nurse model failed to achieve adequate results (n = 15; 3.4%). The two physician team in all 22 cases included an emergency physician and an orthopedic surgeon. The results achieved for each model specific to each of the 4 orthopedic procedures are reported in Table 2.
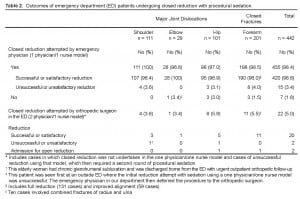
Outcomes of emergency department (ED) patients undergoing closed reduction with procedural sedation.
Overall, procedural sedation was administered 457 times. Adverse events requiring intervention occurred in 12 (2.8%) of 435 cases using the one physician/one nurse model and in none of the 22 two physician/one nurse cases (P = 0.43). Note that the 15 cases initially in the one physician/one nurse group underwent an unsuccessful first attempt at reduction and then were moved into the two physician/one nurse group for the second attempt at reduction. None of these 15 patients experienced an adverse event during their first procedure while in the one physician/one nurse group.
In all cases the ED intervention was sufficient to resolve the adverse event without further sequelae. Most of the adverse events were respiratory in nature. No patients required endotracheal intubation, prolonged observation, or admission for complications. There were no cardiopulmonary arrests and no deaths. The adverse events and their interventions were as follows: One patient who had received etomidate developed apnea, which resolved after 30 seconds of a chin-lift procedure. Eight patients who had received propofol alone developed ventilatory insufficiency (4 with hypoxemia below 90% and 4 with apnea), all of whom were successfully treated with less than 2 minutes of supplemental ventilation via bag-valve mask. One patient who had received propofol developed hypotension, which was treated with a bolus of intravenous saline. Another patient who had received propofol and midazolam developed apnea and hypotension, both of which resolved with intravenous flumazenil. One child who had received ketamine developed urticaria, which resolved with intravenous diphenhydramine. No complication required prolonged observation or hospital admission.
DISCUSSION
This multicenter descriptive study of sedation-assisted closed reduction of major orthopedic injuries demonstrates the safety and effectiveness of the one physician/one nurse approach. In nearly all cases in this series, a single emergency physician performed the complex painful procedure while simultaneously directing procedural sedation—even deep sedation—administered by a credentialed emergency nurse.
The safety of this approach is suggested by the low incidence of adverse events that required intervention. These uncommon outcomes were all readily and fully resolved in the ED and had no impact on the patients’ dispositions. The effectiveness of this approach is seen in the high success rate of our reductions. Over 95% of shoulder, elbow, and hip dislocations were successfully reduced, a rate comparable with or exceeding other published reports.19–28 Our success rate with the reduction of forearm fractures was also comparable with figures reported in the emergency medicine literature.29–32
The bulk of the research on procedural sedation in emergency medicine has been undertaken using two physicians in addition to a registered nurse. This could imply that such a staffing model is the standard approach. One review of the recent literature on procedural sedation in emergency medicine went so far as to aver that “it is generally accepted that a separate professional administers sedation and another performs the procedure.”33 These authors go on to acknowledge that their preferred 4-person model (two physicians, one nurse, and one technician) is not realistically or pragmatically achievable in many community EDs. Nonetheless, they “recommend three professionals be present – one to perform the procedure, one to give medications, and one to watch the patient if feasible.”33
What such an assertion lacks is a compelling warrant. There is insufficient evidence demonstrating an outcome advantage (or disadvantage, for that matter) of a dual-physician approach. No randomized trial has compared a two-physician with a one-physician model. The absence of such high quality research supports the agenda advanced by Miner and Krauss13 that asks “whether emergency physicians can perform the procedure and the sedation simultaneously” and in what situations, if any, might separate operators be indicated.
The closest any ED study comes to comparing the safety of a one-physician with a two-physician model is the nationwide ProSCED registry. Fourteen community EDs in the United States prospectively collected detailed data for over 1,000 sedations involving painful procedures in patients of all ages.34,35 In over 80% these cases, one physician both oversaw the nurse-administered sedation and performed the procedure, which was predominantly a dislocation or fracture reduction. As in our study, they found a very low rate of complications, all of which resolved, and none of which required a change in patient disposition. They observed no difference in complication rates between the one-physician and the two-physician model. Outcomes were not affected when one physician tended exclusively to the sedation while a second physician performed the procedure. Why some procedures involved 2 physicians is not explained. Perhaps the two-physician cases were thought to be at some kind of higher respiratory risk or had a more complicated orthopedic injury, as in several of our cases.
The one physician/one nurse approach is commonly employed with procedural sedation in non-ED settings. Propofol, in fact, is widely and safely administered by a registered nurse under the oversight of a physician who is performing concentration-intensive endoscopy.36–41 The abundance of this literature undergirds the conclusion of Miner and Burton in their review of propofol: “[T]here is no current evidence to suggest that propofol is unsafe without a second physician present.”42
Worth noting is the nature of the procedures emergency physicians commonly perform. Emergency physicians undertake brief procedures, such as the reductions of dislocations and fractures that we describe here. These kinds of short procedures are less likely than endoscopy to interfere with the physician’s overall perception of the patient’s cardiorespiratory status. They also are less likely to impede the ability of the emergency physician to respond to the nurse who is carefully monitoring the patient’s ventilatory and cardiovascular parameters so as to alert the physician of any changes. As Sacchetti et al34 observe, “No emergency physicians performed endoscopies or similar procedures, which would have limited entirely the physician’s ability to continually assess the patient.” Although as noted above, endoscopists safely entrust the administration and monitoring of propofol-induced sedation to a trained registered nurse without a demonstrable compromise to patient safety.36–41 If endoscopists are able to engage in their more demanding procedures while simultaneously overseeing nurse-administered, nurse-monitored procedural sedation, then emergency physicians should be capable of doing the same with their orthopedic procedures. The reassuring safety profile of our study supports this hypothesis.
Other studies in community and academic EDs have shown the safety and effectiveness of the one physician/one nurse-equivalent model, including studies in the U.S. and in Canada.43–45Emergency medicine’s leading organizations have made explicit their support of the one physician/one nurse model. The American College of Emergency Physicians (ACEP) and the Emergency Nurses Association (ENA) issued a joint policy in 2005 supporting the administration of propofol, etomidate, and other sedatives by a credentialed emergency nurse under the direct supervision of an emergency physician.46,47
Yet even in 2007 some controversy remained, particularly surrounding ultra-short-acting “deep sedation” agents such as propofol, “whether there should be an emergency physician separate from the procedure who is wholly dedicated to drug administration and patient monitoring.”42 Contrary to the ACEP policy, some felt credentialed, supervised emergency nurses were not equal to the task. The American Society of Anesthesiology (ASA) is among this group. The ASA had proposed in 2004 (and amended in 2009) that a separate professional, “trained in the administration of general anesthesia,” must be dedicated to the deep sedation, one who is “not simultaneously involved in these surgical or diagnostic procedures.”48 This is not a surprising recommendation from the ASA House of Delegates, who assert that deep sedation can be optimally managed only by anesthesia personnel.48
The Centers for Medicare & Medicaid Services (CMS) issued a similarly restrictive regulation in December 2009, stating that deep sedation can be administered only by an anesthesiologist, a certified registered nurse anesthetist, or a trained medical doctor or a doctor of osteopathy not involved in the performance of a medical procedure. This would prohibit non-anesthesia nursing personnel from administering sedatives like propofol.49 Only a two physician model, or a one physician/one nurse anesthetist model, could operate within these regulatory constraints.
Such a policy struck many as overreaching, cost ineffective, and out of step with the evidence of the safety of deep sedation medication use in the hands of specially trained nurses under direct contemporaneous physician oversight.50–53 In 2010 ACEP, ENA, and the American Academy of Emergency Medicine collectively appealed to CMS.53,54 CMS regulators then met with these leading representatives of the emergency medicine community and subsequently issued an updated bulletin that reflected a more flexible and evidence-based approach.
The revised CMS interpretive guidelines of January 2011 sought to appropriately balance patient safety “with avoidance of undue burdens on facilities or reductions in access to care”.55 These modified regulations transcended the confines of the ASA proscriptions, allowing hospitals to base their policies on a variety of nationally recognized guidelines. Among those now endorsed by the CMS are the ACEP/ENA guidelines that advocate a one physician/one nurse model in which sedation medications are delivered by credentialed emergency nurses working side-by-side with supervising emergency physicians, whom the CMS recognizes as being “uniquely qualified to provide all levels of analgesia/sedation and anesthesia (moderate to deep to general)”.55 ACEP’s 2011 recommendations for physician credentialing, privileging, and practice in procedural sedation and analgesia reflect the revised CMS regulations and further undergird the one physician/one nurse model.56
The growing literature demonstrating the safety of non-anesthesia nurse-administered propofol sedation undercuts the justifiability of the restrictions by the ASA. The results of our study add to the accumulating evidence that most brief orthopedic reductions in emergency medicine can be safely and effectively performed using the one physician/one nurse model. There may be indications for a second physician operator, but further research is needed to spell out under what conditions a dual-physician approach is preferred.
LIMITATIONS
Our results need to be interpreted in the context of several limitations. The major limitation in using electronic health records as a primary data source for a descriptive study is missing, inconsistent, or erroneous documentation. We think this risk is lessened in this study because our EDs require the use of templated electronic documentation for all cases of procedural sedation. These templates call for the nurses to report all adverse events and their interventions. Moreover, all procedural sedation cases undergo monthly quality improvement review, which also tends to improve the quality of documentation. We supplemented the nurses’ records by reviewing the notes of the emergency physicians and the notes of the consultants when present. Although we believe the data regarding the number of participating physicians, intervention-requiring complications, and radiographic outcomes are complete and accurate, we cannot ensure the absence of error to which such studies are liable.
Also, this is simply a descriptive study. Patient allocation to the one physician/one nurse group and the two physician/one nurse group was not randomized. The lack of equivalency between the 2 groups tempers the comparison of adverse events between them. Additionally, our study is underpowered to estimate accurately the incidence of rare events. We also had an insufficient number of patients to stratify outcomes by types of sedative, dosing, and route of administration. Lastly, these results are specific to our practice setting and may not be generalizable to other EDs or healthcare delivery systems.
CONCLUSION
This multicenter descriptive study suggests that sedation-assisted closed reduction of major joint dislocations and forearm fractures can be performed effectively and safely in the ED using a one physician/one nurse model. Requiring a second physician (or nurse anesthetist) to adminster medications for all sedation-assisted ED procedures is unncessarily cautious and would fail to match healthcare resources to patient needs. Further research is needed to determine which specific clinical scenarios might benefit from a dual-physician approach.
Footnotes
We would like to thank Lynde Rammelsberg, Consulting Data Analyst, for her generous assistance with identifying our patient cohort. We are grateful, as well, to Mary E. Reed, DrPH, Staff Scientist, Kaiser Permanente Division of Research, for her data analysis, and to Steve Green, MD, Professor of Emergency Medicine & Pediatrics, Loma Linda University Medical Center & Children’s Hospital, for his review of a section of our discussion. The leadership of our emergency department deserves acknowledgment for longASA.Theresultsofour supporting our department’s research division and its research internship program. Thanks are due as well to the Kaiser Permanente Northern California Community Benefit Programs for their financial support.
Supervising Section Editor: Eric Snoey, MD
Submission history: Submitted February 2, 2012; Revisions recieved April 9, 2012; Accepted April 30, 2012
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2012.4.12455
Address for Correspondence: David R. Vinson, MD, Kaiser Permanente Roseville Medical Center, Department of Emergency Medicine, 1600 Eureka Road, Roseville, CA 95661
Email: drvinson@ucdavis.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Kuypers MI, Mencl F, Verhagen MF, et al. Safety and efficacy procedural sedation with propofol in a country with a young emergency medicine training program. Eur J Emerg Med. 2011;18:162–7.[PubMed]
2. Andolfatto G, Willman E. A prospective case series of single-syringe ketamine-propofol (Ketofol) for emergency department procedural sedation and analgesia in adults. Acad Emerg Med.2011;18:237–45. [PubMed]
3. David H, Shipp J. A randomized controlled trial of ketamine/propofol versus propofol alone for emergency department procedural sedation. Ann Emerg Med. 2011;57:435–41. [PubMed]
4. Shah A, Mosdossy G, McLeod S, et al. A blinded, randomized controlled trial to evaluate ketamine/propofol versus ketamine alone for procedural sedation in children. Ann Emerg Med.2011;57:425–33.e2. [PubMed]
5. Miner JR, Danahy M, Moch A, et al. Randomized clinical trial of etomidate versus propofol for procedural sedation in the emergency department. Ann Emerg Med. 2007;49:15–22. Epub 2006 Sep 25. [PubMed]
6. Burton JH, Miner JR, Shipley ER, et al. Propofol for emergency department procedural sedation and analgesia: a tale of three centers. Acad Emerg Med. 2006;13:24–30. [PubMed]
7. Dunn MJ, Mitchell R, Souza CD, et al. Evaluation of propofol and remifentanil for intravenous sedation for reducing shoulder dislocations in the emergency department. Emerg Med J.2006;23:57–8. [PMC free article] [PubMed]
8. Miner JR, Biros M, Krieg S, et al. Randomized clinical trial of propofol versus methohexital for procedural sedation during fracture and dislocation reduction in the emergency department. Acad Emerg Med. 2003;10:931–7. [PubMed]
9. Godambe SA, Eliot V, Matheny D, et al. Comparison of propofol/fentanyl versus ketamine/midazolam for brief orthopedic procedural sedation in a pediatric emergency department.Pediatrics. 2003;112:116–23. [PubMed]
10. Coll-Vincent B, Sala X, Fernández C, et al. Sedation for cardioversion in the emergency department: analysis of effectiveness in four protocols. Ann Emerg Med. 2003;42:767–72.[PubMed]
11. Bassett KE, Anderson JL, Pribble CG, et al. Propofol for procedural sedation in children in the emergency department. Ann Emerg Med. 2003;42:773–82. [PubMed]
12. Guenther E, Pribble CG, Junkins EP, Jr, et al. Propofol sedation by emergency physicians for elective pediatric outpatient procedures. Ann Emerg Med. 2003;42:783–91. [PubMed]
13. Miner JR, Krauss B. Procedural sedation and analgesia research: state of the art. Acad Emerg Med. 2007;14:170–8. [PubMed]
14. Vinson DR, Bradbury DR. Etomidate for procedural sedation in emergency medicine. Ann Emerg Med. 2002;39:592–8. [PubMed]
15. Burton JH, Vinson DR, Drummond K, et al. Electrical cardioversion of emergency department patients with atrial fibrillation. Ann Emerg Med. 2004;44:20–30. [PubMed]
16. Bhatt M, Kennedy RM, Osmond MH, et al. Consensus-based recommendations for standardizing terminology and reporting adverse events for emergency department procedural sedation and analgesia in children. Ann Emerg Med. 2009;53:426–35.e4. [PubMed]
17. Green SM, Yealy DM. Procedural sedation goes Utstein: the Quebec guidelines. Ann Emerg Med.2009;53:436–8. [PubMed]
18. White PF, Song D. New criteria for fast-tracking after outpatient anesthesia: a comparison with the modified Aldrete’s scoring system. Anesth Analg. 1999;88:1069–72. [PubMed]
19. Hendey GW, Avila A. The Captain Morgan technique for the reduction of the dislocated hip. Ann Emerg Med. 2011;58:536–40. [PubMed]
20. Jacques KG, Dewar A, Gray A, et al. Procedural sedation and analgesia in a large UK Emergency Department: factors associated with complications. Emerg Med J. 2011;28:1036–40. [PubMed]
21. Wakai A, O’Sullivan R, McCabe A. Intra-articular lignocaine versus intravenous analgesia with or without sedation for manual reduction of acute anterior shoulder dislocation in adults. Cochrane Database Syst Rev. 2011;4:CD004919. [PubMed]
22. Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl. 2009;91:2–7.[PMC free article] [PubMed]
23. Mathieu N, Jones L, Harris A, et al. Is propofol a safe and effective sedative for relocating hip prostheses? Emerg Med J. 2009;26:37–8. [PubMed]
24. Gagg J, Jones L, Shingler G, et al. Door to relocation time for dislocated hip prosthesis: multicentre comparison of emergency department procedural sedation versus theatre-based general anaesthesia. Emerg Med J. 2009;26:39–40. [PubMed]
25. Fitch RW, Kuhn JE. Intraarticular lidocaine versus intravenous procedural sedation with narcotics and benzodiazepines for reduction of the dislocated shoulder: a systematic review. Acad Emerg Med. 2008;15:703–8. [PubMed]
26. Frymann SJ, Cumberbatch GL, Stearman AS. Reduction of dislocated hip prosthesis in the emergency department using conscious sedation: a prospective study. Emerg Med J. 2005;22:807–9. [PMC free article] [PubMed]
27. Germann CA, Geyer DA, Perron AD. Closed reduction of prosthetic hip dislocation by emergency physicians. Am J Emerg Med. 2005;23:800–5. [PubMed]
28. Austin T, Vilke GM, Nyheim E, et al. Safety and effectiveness of methohexital for procedural sedation in the emergency department. J Emerg Med. 2003;24:315–8. [PubMed]
29. Betham C, Harvey M, Cave G. Manipulation of simple pediatric forearm fractures: a time-based comparison of emergency department sedation with theatre-based anaesthesia. N Z Med J.2011;124:46–53. [PubMed]
30. Khan S, Sawyer J, Pershad J. Closed reduction of distal forearm fractures by pediatric emergency physicians. Acad Emerg Med. 2010;17:1169–74. [PubMed]
31. Pershad J, Williams S, Wan J, et al. Pediatric distal radial fractures treated by emergency physicians. J Emerg Med. 2009;37:341–4. [PubMed]
32. Sharieff GQ, Trocinski DR, Kanegaye JT, et al. Ketamine-propofol combination sedation for fracture reduction in the pediatric emergency department. Pediatr Emerg Care. 2007;23:881–4.[PubMed]
33. Smally AJ, Nowicki TA, Simelton BH. Procedural sedation and analgesia in the emergency department. Curr Opin Crit Care. 2011;17:317–22. [PubMed]
34. Sacchetti A, Senula G, Strickland J, et al. Procedural sedation in the community emergency department: initial results of the ProSCED registry. Acad Emerg Med. 2007;14:41–6. [PubMed]
35. Hogan K, Sacchetti A, Aman L, Opiela D. The safety of single-physician procedural sedation in the emergency department. Emerg Med J. 2006;23:922–3. [PMC free article] [PubMed]
36. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr. 2012;54:171–85. [PubMed]
37. Bosslet GT, Devito ML, Lahm T, Sheski FD, Mathur PN. Nurse-administered propofol sedation: feasibility and safety in bronchoscopy. Respiration. 2010;79:315–21. [PubMed]
38. Horiuchi A, Nakayama Y, Hidaka N, Ichise Y, Kajiyama M, Tanaka N. Low-dose propofol sedation for diagnostic esophagogastroduodenoscopy: results in 10,662 adults. Am J Gastroenterol.2009;104:1650–5. [PubMed]
39. Tohda G, Higashi S, Wakahara S, Morikawa M, Sakumoto H, Kane T. Propofol sedation during endoscopic procedures: safe and effective administration by registered nurses supervised by endoscopists. Endoscopy. 2006;38:360–7. [PubMed]
40. Rex DK, Heuss LT, Walker JA, Qi R. Trained registered nurses/endoscopy teams can administer propofol safely for endoscopy. Gastroenterology. 2005;129:1384–91. [PubMed]
41. Walker JA, McIntyre RD, Schleinitz PF, et al. Nurse-administered propofol sedation without anesthesia specialists in 9152 endoscopic cases in an ambulatory surgery center. Am J Gastroenterol. 2003;98:1744–50. [PubMed]
42. Miner JR, Burton JH. Clinical practice advisory: Emergency department procedural sedation with propofol. Ann Emerg Med. 2007;50:182–7. 7.e1. [PubMed]
43. Charles M, McGinnis HD, Wehner P. Propofol for procedural sedation: one versus two physicians.Ann Emerg Med. 2005;46:S73–4. 261. abstract.
44. Campbell SG, Magee KD, Kovacs GJ, et al. Procedural sedation and analgesia in a Canadian adult tertiary care emergency department: a case series. CJEM. 2006;8:85–93. [PubMed]
45. Mensour M, Pineau R, Sahai V, et al. Emergency department procedural sedation and analgesia: A Canadian Community Effectiveness and Safety Study (ACCESS) CJEM. 2006;8:94–9. [PubMed]
46. Emergency Nurses Association; American College of Emergency Physicians Delivery of agents for procedural sedation and analgesia by emergency nurses. Ann Emerg Med. 2005;46:368. [PubMed]
47. Godwin SA, Caro DA, Wolf SJ, et al. American College of Emergency Physicians Clinical policy: procedural sedation and analgesiain the emergency department. Ann Emerg Med. 2005;45:177–96.[PubMed]
48. American Society of Anesthesiologists. Statement on safe use of propofol. (Approved October 27, 2004, and amended on October 21, 2009). Available at:http://www.asahq.org/~/media/for%20members/documents/standards%20guidelines%20stmts/safe%20use%20of%20propofol.ashx. Accessed July 20, 2012.
49. Centers for Medicare & Medicaid Services (CMS). Clarificationsf the Interpretive Guidelines for the Anesthesia Services Condition of Participation, and Revised Hospital Anesthesia Services Interpretive Guidelines State Operations Manual (SOM) Appendix A, S&C-10-09-Hospital. CMS publication no. 100-07. December 11, 2009.
50. Rex DK. Effect of the Centers for Medicare & Medicaid Services policy about deep sedation on use of propofol. Ann Intern Med. 2011;154:622–6. [PubMed]
51. Hannenberg AA. Effect of the Centers for Medicare & Medicaid Services policy about deep sedation on use of propofol. Ann Intern Med. 2011;155:405. author reply. [PubMed]
52. Vargo JJ. A SEER snapshot of anesthesiologist-assisted procedural sedation: in or out of focus?Clin Gastroenterol Hepatol. 2012;10:7–8. [PubMed]
53. Clinical Practice Statement: Propofol and other sedating agents can be safely used by emergency physicians without an anesthesiologist present. (2/17/2012) Available at:http://www.aaem.org/UserFiles/file/propofol_references.pdf. Accessed July 20, 2012.
54. Gardner AF, Blumstein H, Gurney D. Appeal letter [re: Revised Hospital Anesthesia Services Interpretive Guidelines Ref S&C 10-09 (revised 2/5/10) 42 CFR48252] to Thomas Hamilton, Director, Survey and Certification Group, Centers for Medicare and Medicaid Services, Baltimore, MD (sent on behalf of the American College of Emergency Physicians, the American Academy of Emergency Medicine, and the Emergency Nurses Association by the Presidents of these three organizations). March 22, 2010.
55. American Academy of Emergency Medicine. Centers for Medicare & Medicaid Services (CMS). State Operations Provider Certification. Revised Appendix A, Interpretive Guidelines for Hospitals. CMS publication no. 100-07. January 14, 2011. Available at:https://www.cms.gov/SurveyCertificationgeninfo/downloads/SCLetter11_10.pdf. Accessed July 20, 2012.
56. O’Connor RE, Sama A, Burton JH, et al. American College of Emergency Physicians. Procedural sedation and analgesia in the emergency department: recommendations for physician credentialing, privileging, and practice. Ann Emerg Med. 2011;58:365–70. [PubMed]


