| Author | Affiliation |
|---|---|
| Julie Gorchynski, MD, MSc | Texas A&M, Corpus Christi |
| Worth Everett, MD | University of Pennsylvania |
| Linda Prebil | Pharmaceutical Product of Development Incorporated |
ABSTRACT
Background
Lumbar Puncture (LP) is an invasive procedure frequently used to diagnose meningitis among the pediatric population. Neonates and infants have not routinely received local anesthesia prior to LP.
Study Objective
To determine whether emergency medicine physicians and pediatricians use local analgesics on neonates and infants prior to performing an LP and to identify which local anesthetics, if any, were used.
Methods
Prospective, cohort study of all infants, six months of age or less, that received an LP in the emergency department (ED) or inpatient pediatric units for suspected meningitis during a period of year at a university tertiary care hospital.
Results
A total sample population of 111 infants that received an LP within the study period. A control population of 42 adults received an LP. Only 40.4% (45/111) of the infants received local analgesia prior to LP: either 1% lidocaine, EMLA or a combination of the two. Infants were less likely to receive lidocaine or EMLA prior to LP compared to adult subjects (OR= 0.27; 95% CI0.12 to 0.62). No neonates that were less than one month of age received local procedural anesthesia by emergency medicine or pediatric physicians. ED physicians’ use of local anesthesia prior to LP increased with increasing age of the infant. The pediatricians in this study used local anesthesia prior to LP when the infant was at least five months of age.
Discussion
The data objectively support recent literature regarding the under use or lack of use of analgesia prior to LP among neonates and infants. Local anesthetics should be used routinely without exception prior to performing an LP in the pediatric population.
INTRODUCTION
Lumbar punctures (LP) are performed frequently in emergency departments (EDs) and on hospitalized pediatric patients. It is an invasive but essential procedure, most often used to diagnose meningitis. Local anesthetics, including the common amide and ester anesthetics (lidocaine, mepivicaine, procaine) are commonly used prior to performing LPs as in adults and adolescents. It is felt that infants and neonates should receive local anesthetics, such as lidocaine or a 1:1 mixture of lidocaine and prilocaine also know as eutectic mixture of local anesthetics (EMLA), as standard medical care prior to an LP. Infants are a vulnerable population with regards to assessing pain as they are unable to verbally communicate, therefore presenting a challenge to the medical community. TheInternational Association of the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with the actual or potential tissue damage or described in terms of such damage.”1
Recent studies have linked altered pain responses in infants with cumulative exposures to pain. 5,6 Neonatal and infant nervous systems may be less effective in managing painful stimuli.5,6 Invasive procedures during infancy cause distress, delayed recovery and can lead to developmental issues. 5,6 A paradigm shift has occurred within the medical community in the recognition of pediatric pain resulting in attempts to develop methods for quantifying pain such as behavioral observational scales.
This prospective study is in response to the medical and general community’s awareness of pain control. The aim was to determine if analgesics were administered prior to pediatric LPs in the emergency and pediatric departments.
METHODS
The study occurred at a university-based tertiary referral hospital in southern California. Subjects included children six months of age or less who underwent LP in the ED or any pediatric unit. Pediatric units included the pediatric intensive care unit, the neonatal intensive care unit, and the general pediatric ward. Patients were excluded if they were intubated or developmentally disabled. If multiple LPs were performed, only the first procedure was included. The LP procedural data forms study were distributed to the ED and pediatric units and were collected and reviewed over a one-year period from September 2001 though September 2002. Identification of patients who underwent LPs occurred by weekly collection of LP procedural data forms from the ED and pediatric units. Data was abstracted from the pediatric chart to complete any missing data from the study LP procedural data forms. The hospital laboratory logs were used to cross-reference all received cerebrospinal fluid (CSF) samples, thus enabling capture of all LPs performed in our study age population. Data were abstracted by a trained and patient age, date of LP, type of LA, and other medications administered. To assess the data abstraction methods 10 medical data collection forms were randomly chosen and reviewed by a second reviewer, yielding an assessment of inter-rater reliability (kappa). To control for documentation deficiencies, 42 consecutive data LP forms for adult ED patients who underwent LP were collected and reviewed. The protocol was approved by the institutional review board as an exempt study.
Statistical Analysis
Data were analyzed using STATA (version 7.0, Stata Corp., College Station, Texas). Proportions with 95% confidence intervals (CI) were calculated for local anesthetic use, defined as lidocaine or EMLA for pediatric and adult patients. In order to estimate the effect of missing documentation on the magnitude of the proportion of local anesthetic used, a sensitivity analysis was performed in which three different proportions of the missing data were estimated. The situations in which all, one half, and none of the procedures with missing documentation would have demonstrated local anesthetic use was estimated. This demonstrates the maximum and minimum proportions possible. Finally, the odds ratio of infants six months of age or less receiving local anesthetic in conjunction with lumbar puncture compared to adult patients was calculated.
RESULTS
The age of the study subjects was based on a prior retrospective cross-sectional study conducted the year before at the same institution. Data was collected and statistically analyzed on a total of 82 infants, 12 months of age or less, who had an LP performed for suspected meningitis in the ED and inpatient pediatric units.
A total of 194 LP procedural data forms were collected and reviewed including 42 adult and 111 pediatric subjects (Figure 1). Twelve pediatric charts were excluded due to intubation or conscious sedation and 29 subjects had incomplete data collection forms. The ED physicians and pediatric physicians preferentially used 1% lidocaine and EMLA, respectively, for local analgesic prior to infant LP. The Table shows that the use of local anesthetics was more common among adult subjects. Narcotics, benzodiapepines, and conscious sedation use were also more common among adults. Ketamine was not used in this series. Infants were less likely to receive lidocaine or EMLA before an LP compared to adult subjects (OR= 0.33; 95% CI 0.13 to 0.79).
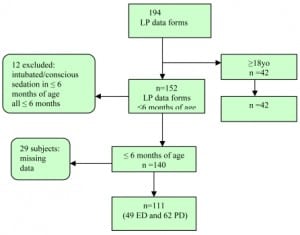
Flow diagram of sample population. LP = lumbar puncture, ED = emergency department, PD = pediatric department
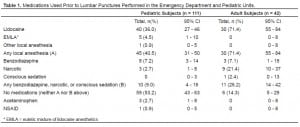
Medications Used Prior to Lumbar Punctures Performed in the Emergency Department and Pediatric Units.
Of all the subjects that received either EMLA or 1% lidocaine, only one infant received Tylenol as an adjunct for analgesia and three subjects that had EMLA applied, two had received Tylenol and only one had received a NSAID agent. Narcotics and Benzodiapzepines were not administered as an adjunct agent in those infants that had received either EMLA or lidocaine.
There were more LPs performed in the pediatric units than in the ED since our institution is a referral center with a PICU transport service that provides direct admissions to the pediatric units bypassing the ED for their initial evaluation.
A sensitivity analysis was conducted to account for the missing data from 29 subjects. The minimum ranges from 33.3 (95% CI 24.7 to 42.9) of infants receiving lidocaine or EMLA. The minimum assumes none of the 29 subjects were administered lidocaine or EMLA prior to the LP. Forty-seven (95% CI 37 to 56.6) signifies half of the 29 subjects received lidocaine or EMLA. Finally, if all 29 subjects received lidocaine or EMLA a maximum 59.5 (95% CI 49.7 to 68.7) subjects received appropriate local analgesic prior to an LP.
DISCUSSION
Anatomic, physiologic and biochemical prerequisites for nocioreception are developed by the neonatal period.2 Standard medical practice dictates lidocaine or EMLA should be used to minimize the pain of an LP.4 Local anesthetics can be safely used in neonates and children although excessive plasma concentrations can result in seizures and cardiac depression. The maximal recommended dose of lidocaine is 4mg per kilogram without epinephrine and 5mg per kilogram with epinephrine in neonates.3 Orthotoludine is a metabolite of prilocaine, an oxidant that can lead to methemoglobinemia in neonates. EMLA, therefore should be limited in neonates. A single application of EMLA for procedures, such as LP, has been shown to be safe and effective.1
Infants are easily held in the appropriate LP position and cannot verbalize their perception of pain or be observed for visual pain assessment. “Perception reflects the effect of the nocioreceptive information on the existing psychological framework. Perception is the emotional and physical experience of pain. That experience then changes the framework thereby affecting subsequent painful experiences altering subsequent pain pathway development resulting in decreased pain tolerance.”2,6 Several short-term observational studies have been conducted illustrating neonates and infants without adequate anesthesia during a painful procedure showed more distress in subsequent procedures.7,8
The odds ratio of receiving anesthetic prior to LP if you are a neonate or infant is low in the emergency and pediatric departments at our institution. We can speculate if all 29 data collection forms were positive for analgesic then the pediatric population would be 10% lower than the adult group, increasing the odds ratio dramatically.
One common deficiency among physicians is the lack of proper training in current concepts, methods and use of procedural pain management in the pediatric population. Additionally, the preconceived notion that the physician will obtain the CSF with one attempt at LP and therefore rationalizing that prior subcutaneous injection of lidocaine may cause more pain and discomfort is not supported by the literature.8,9 In the majority of cases several attempts are usually required before a successful LP. EMLA requires approximately 60 minutes for adequate analgesia and in the ED it is not routinely used because of the urgency to obtain CSF and initiate antibiotics.8,9 Another common generalization that local injection of an anesthetic may obscure the landmarks for LP is unsubstantiated by the medical literature.8,9
LIMITATIONS
The data collection tool should have included the CSF sample results or a diagnosis of whether viral or bacterial meningitis was present and the physical assessment of the subject. The diagnosis of meningitis and some key features of the physical assessment could have been used as an indicator of time signifying if the LP needed to be performed emergently disallowing the use of topical anesthetics, particularly EMLA. This study was centered in one institution and may not be representative of the entire medical community.
A multi-center prospective study should be considered in the future that utilizes video recordings of lumbar punctures in infants and the elderly. Trained observers could quantify the pain using a visual pain assessment scale and the use of anesthetic prior to lumbar punctures would be recorded.
CONCLUSIONS
The data demonstrates the underutilization of local anesthesia prior to LP in infants six months of age or less by both emergency medicine and pediatric physicians. The data supports prior generalized statements in the literature regarding under use or lack of use of procedural analgesics among the pediatric population.
It is the authors’ opinion that local anesthetics should be used prior to performing pediatric lumbar punctures. ED physicians and pediatricians must proactively educate and practice maximal procedural pain management in the pediatric population.
Footnotes
Submission history: Submitted May 8, 2007; Accepted November 2, 2007.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Julie Gorchynski, MD, MSc, FACEP, FAAEM Department of Emergency Medicine, Texas A&M, Corpus Christi, CHRISTUS-Spohn, 2606 Hospital Blvd. 3W, Department of Emergency Medicine, Corpus Christi, TX 78405
Email: jgorchyn@msn.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Golianu B, Krane EJ, Galloway KS, Yaster M. Pediatric acute pain management. Ped Clin N Amer. 2000;47:559–588.
2. Greenburg CS, Franck LS, Stevens B. Pain Assesment in infants and children. Ped Clin N Amer. 2000;47:487–512.
3. Berde CB, Sethna NF. Analgesics for the treatment of pain in children. N Engld J Med.2002;347:1094–1103.
4. Brent AS. The management of pain in the emergency department. Ped Clinics N Amer.2000;47:651–679.
5. Klein ER. Premedicating children for painful invasive procedures. J Pediatr Oncol Nors.1992;4:170–179.
6. Fitzgerald M, Beggs S. The neurobiology of pain: developmental aspects. Nueroscientist.2001;3:246–247.
7. Weisman SJ, Bernstein B, Schechter NL. Consequences of inadequate analgesia during procedures in children. Arch Pediatr Adolesc Med. 1998;152:147–149. [PubMed]
8. Pinheiro JM, Furdon S, Ochoa LF. Role of local anesthesia during lumbar punctures in neonates. Pediatrics. 1993;91:379–82. [PubMed]
9. Baxter AL, Fisher RG, Burke BL, Goldblatt SS, Isaacman DJ, Lawson MO. Local Anesthsetic Stylet and Styles: Factors associated with resident lumbar puncture success.Pediatrics. 2006;117:876–881. [PubMed]


