| Author | Affiliation |
|---|---|
| Jeffrey H. Luk, MD, MS | University Hospitals Case Medical Center, Department of Emergency Medicine, Cleveland, Ohio |
| Brian Walsh, MD, MBA | Morristown Memorial Hospital, Department of Emergency Medicine, Morristown, New Jersey |
| Paul Yasbin, BS | Chilton Hospital, Pompton Plains, New Jersey |
Introduction Methods Results Discussion Conclusion
ABSTRACT
Introduction: Very few studies exist on the use of diltiazem in the prehospital setting. Some practitioners believe this medication is prone to causing hypotension in this setting. Our goals were to determine whether the prehospital administration of diltiazem induced hypotension and to evaluate the efficacy of the drug.
Methods: Our two-tiered system is located in a suburban region of New Jersey with advanced life support (ALS) care provided by fly-car units. The ALS units do not transport patients, and all of them are hospital based. The ALS providers are employed by the hospital system. In New Jersey, all ALS care requires online medical control, including the administration of diltiazem. We retrospectively reviewed patient care records for those who were believed to be in rapid atrial fibrillation and were given diltiazem in a suburban emergeny medical services system over a 22-month period. We examined the differences between heart rate (HR) and blood pressure (BP) on the initial evaluation and on arrival to the emergency department (ED). A hypotensive response was defined as a final systolic BP (SBP) less than 90 mmHg and a drop in SBP of at least 10 mmHg. Diltiazem was considered effective if the ED HR was <100 beats per minute (bpm) or if it decreased ≥20%.
Results: During the study period, 26,979 patients were transported. Of these patients, 2,488 had a documented rhythm of atrial fibrillation or atrial flutter. Of the 320 patients who received diltiazem, 42 patient encounters were excluded for incomplete data, yielding 278 patients for analysis. The average initial SBP was 139 mmHg and the average diastolic BP was 84 mmHg. The average diltiazem dosage was 16.7 mg. Two patients became hypotensive. The average initial HR was 154 bpm. On arrival to the ED, 33% of the patients had an HR < 100 bpm and 69% had a drop in HR ≥ 20%. The overall efficacy of prehospital diltiazem was 73%.
Conclusion: In the prehospital setting, diltiazem is associated with a very low rate of hypotension and appears to be effective in decreasing HR adequately. Prospective studies are needed to confirm these findings.
INTRODUCTION
Atrial fibrillation is a common dysrhythmia in the United States. Its prevalence has been reported from 2.3% in persons older than 40 years to 5.9% in persons older than 65 years.1 Uncontrolled rapid atrial fibrillation with an accelerated ventricular response can lead to impaired diastolic filing, loss of atrial kick, decreased ventricular output, and decreased coronary perfusion. The primary treatment goal is to control the ventricular rate. However, there are various methods of treating uncontrolled atrial fibrillation. In an unstable patient, cardioversion is the first-line treatment. If the patient is stable, various pharmacologic agents can be used, including digitalis, beta-blockers, and calcium channel blockers. One such calcium channel blocker is diltiazem.
Diltiazem slows atrioventricular (AV) nodal conduction, thereby prolonging the AV nodal refractory period. This medication is widely used in the emergency department (ED) setting. In the past, its use in the prehospital setting was limited because of various storage issues, particularly the need to store it at 2°C to 8°C. However, with the introduction of lyophilized diltiazem, it has been asserted that this medication can and should be used by prehospital providers in treating tachydysrhythmias.2
Many emergency medical services (EMS) systems have adopted the adult advanced cardiac life support guidelines recommending the use of intravenous (IV) diltiazem as a first-line pharmacotherapy to control the ventricular response in rapid atrial fibrillation.3 However, previous studies have shown that IV administration of diltiazem can lead to a decrease in blood pressure because of its negative inotropic effect and its inhibition of intracellular calcium influx on vascular smooth muscle, leading to a decrease in total peripheral resistance. Several studies totaling more than 450 patients have described up to an 18% prevalence of reported diltiazem-induced hypotension (defined as systolic blood pressure [SBP] < 90 mmHg) with a mean of 9.7%.4
Furthermore, the safety and efficacy of this medication when used in the prehospital setting has not been well studied.5 A Medline reviewof the literature revealed only 1 prior study in which the safety of diltiazem in the prehospital setting was evaluated. This retrospective case-controlled study of 43 patients who were given diltiazem in the prehospital setting demonstrated good efficacy and no adverse effects.1
We sought to determine whether the use of diltiazem is safe in the prehospital setting by determining the prevalence of hypotension in patients who were administered diltiazem. Our secondary objective was to evaluate the efficacy of prehospital administration of diltiazem by determining the percent of patients whose heart rates were controlled after being treated with diltiazem.
METHODS
Setting/System
Our system is in a suburban region of New Jersey. Seven advanced life support (ALS) fly-car units in our system bring approximately 90% of their patients to 1 of 3 hospitals. Two of the hospitals in the system are community hospitals, and one is an academic tertiary care center with an emergency medicine residency. The system is two-tiered, and ALS units do not transport patients. All ALS units are hospital based, and ALS providers are employed by the hospital system. Every ALS unit consists of 2 ALS providers. In New Jersey, all ALS care requires online medical control. Thus, for every patient treated by ALS services, the provider must contact a physician by telephone to receive online medical control. The ALS providers can perform and transmit electrocardiograms (ECG) at their discretion, but they cannot administer diltiazem until instructed to do so by the physician as per our system’s protocols. Accordingly, the administration of diltiazem requires online medical control from the base hospital and is not protocol driven. Similarly, ALS units carry lidocaine, amiodarone, and adenosine, which can also be given at the physician’s discretion via medical command and are not standing orders in the protocols for our system.
Population
The ALS providers in our system cover 244 square miles, perform 26,000 dispatches per year, and treat approximately half of the calls to which they are dispatched.
Data/Analysis
Using our prehospital patient care record electronic database, emsCharts Inc (Pittsburgh, Pennsylvania), we retrospectively reviewed charts of all patients treated by our ALS providers over a 22-month period from February 2007 to November 2008. The review was conducted according to applicable criteria previously proposed by Worster et al.6 The people abstracting the data were trained, inclusion and exclusion criteria were established, and variables were defined. The medical record database was also identified. Those patients with missing data were not included in the analysis as described in the Results section. However, sampling did not occur in this study because all patients treated with diltiazem were selected. Abstraction forms were not used because the data were evaluated and analyzed in an electronic database. In addition, the abstractors were aware of the hypothesis and study objectives; their performance was not monitored; and interrater reliability was not discussed, tested, or measured because the data analysis was based on objective data and not on the judgments or opinions of the people abstracting the data. This study was exempt from institutional review board approval.
After unique patient identifiers were removed, we selected those patients with a heart rate (HR) greater than 100 beats per minute (bpm) who were given diltiazem. We then examined the HR and blood pressure (BP) at the initial evaluation and on arrival to the ED. The differences in HR and BP between the initial evaluation and ED arrival were calculated. A priori, a hypotensive response after the administration of diltiazem was defined as a final SBP less than 90 mmHg and a drop in SBP of at least 10 mmHg from the initial reading. Diltiazem was considered effective if the HR on ED arrival was less than 100 bpm or if the HR had decreased at least 20%. The number of administrations of diltiazem and the milligram dose of each administration were also noted for each patient.
RESULTS
During the study period, 26,979 transports were conducted. The average time from arrival on the scene to arrival at the ED was 28 minutes (standard deviation [SD], 20 minutes), and the average transport time (time from leaving the scene to arriving at the ED) was 10 minutes (SD, 6 minutes). Of these patients, 2,488 had a documented rhythm of atrial fibrillation or atrial flutter. We reviewed the charts of 324 patients who were given diltiazem in the prehospital setting.
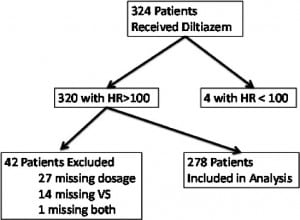
Their demographic and transport information can be found in the Appendix (online only). During the 22-month period, each paramedic in our system administered diltiazem to an average of 3.3 patients (SD, 2.8; 95% confidence interval [CI], 2.9–3.9). Of the 324 patients, 4 were given diltiazem for an HR less than 100 bpm. Of the remaining 320 patients, 27 were excluded because the dose of diltiazem was not recorded on the prehospital chart. An additional 14 patients were excluded because the HR and BP readings were not complete. One patient chart was excluded because it was missing both the diltiazem dose and complete vital signs (Figure 1).
Safety
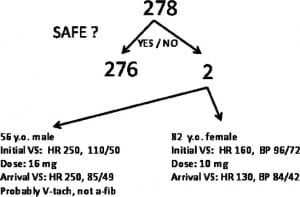
Of the 278 patients included in the analysis, 2 patients became hypotensive after treatment with IV diltiazem. Thus, the prevalence of hypotension was 0.7% (95% CI, 0–2%; Figure 2).
Efficacy
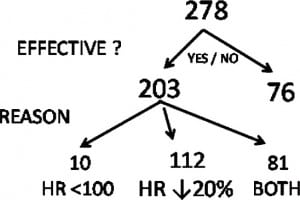
Of the 278 patients in the analysis, 33%(95% CI, 27–38%) had an HR of <100 bpm on arrival at the ED. Sixty-nine percent (95% CI: 64–74%) of patients had a drop in HR ≥ 20%. Accordingly, 73% (95% CI, 68–78%) of patients overall had an effective response in which the HR was <100 bpm or the HR decreased by at least 20%. Neither of the 2 patients who became hypotensive had effective responses (Figure 3).
DISCUSSION
To our knowledge, this is the largest retrospective chart review of diltiazem use in the prehospital setting. Very few studies have evaluated the use of diltiazem in the prehospital setting. In 1999, Wang et al1conducted a retrospective, casecontrolled study of 43 patients with HRs > 150 who were treated with diltiazem and compared these patients to 27 control subjects. The study found that none of the patients given diltiazem required treatment for hypotension, cardiac arrest, or intubation. Except for 1 patient with a low baseline SBP who received diltiazem, Wang et al1 found no instances of SBP reduction below 90 mmHg after treatment with diltiazem. Furthermore, using a similar definition for successful treatment as in the current study, Wang et al1 found that 35 of the 43 patients (81%) receiving diltiazem therapy had an overall therapeutic response.
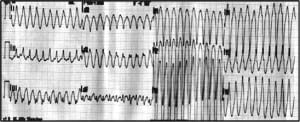
Our study found only 2 patients who had a hypotensive response to diltiazem. One patient was an 82-year-old woman who had an initial HR of 160 bpm and was initially borderline hypotensive with a BP of 96/72 mmHg. After being treated with 10 mg of diltiazem, her HR decreased to 130 bpm and her BP dropped to 84/42 mmHg. The other patient was a 56-year-old man who presented with chest pain and dyspnea that started while he was jogging. He was treated with 16 mg of diltiazem for an initial rhythm that was interpreted as atrial flutter. His initial vital signs included a HR of 250 bpm and a BP of 110/50 mmHg. On arrival in the ED, his HR remained at 250 bpm, but his BP dropped to 85/49 mmHg. On further review of his chart, however, it was determined that his initial rhythm was probably ventricular tachycardia instead of atrial flutter/fibrillation (Figure 4).
In addition, the percentage of patients who experienced a hypotensive response to diltiazem slightly drops if the excluded patients are included in the analysis. Forty-two patients were excluded from the study for incomplete data. Of these patients, 27 were missing only the dose of diltiazem given, and 11 patients were missing only diastolic BPs. None of these patients became hypotensive after the administration of IV diltiazem. Thus, if these patients were included in the analysis, the rate of hypotension would be 0.6% (95% CI, 0–1.5%). In addition, 33 of the 38 patients excluded had an effective response to diltiazem. Accordingly, if these patients were included in the analysis, the efficacy of diltiazem would increase to 75% (95% CI, 70–79%).
Four of the excluded patients were missing HR or SBP measurements on initial presentation or on arrival at the ED. Even if it is assumed that all of these patients became hypotensive after receiving diltiazem, the prevalence of hypotension would only increase to 1.9% (95% CI, 0.4–3.4%). Furthermore, if these 4 patients had ineffective responses to diltiazem, the efficacy of diltiazem would drop only 1% to 74% (95% CI, 69–79%).
Nevertheless, the concern that diltiazem has adverse side effects is still prevalent. Vinson et al7 reported a patient who developed tetany with sudden respiratory arrest after receiving a standard dosage of diltiazem (ie, 0.24 mg/kg IV) over 2 to 3 minutes for narrow complex atrial fibrillation with a rapid ventricular response. Vinson et al7 reported that within 1 minute of receiving the diltiazem, the patient developed severe, generalized muscle spasm associated with rapidly decreasing oxygen saturation to below 60%. The patient ultimately became unconscious and was about to undergo rapid sequence intubation. Before the patient was intubated, he was given 10 mL of 10% calcium chloride, and his tetanic contractions immediately resolved. Vinson et al7 reported that spontaneous chest excursions then returned, followed by a steady recovery in oxygenation and ventilatory function.
Hypotension is another major adverse effect of diltiazem, and it is believed that 2 main mechanisms of action are responsible for this adverse effect: (1) its effect on vascular smooth muscle as an inhibitor of intracellular calcium influx, thereby decreasing total peripheral resistance, and (2) its negative inotropic effect. Accordingly, it would be reasonable to believe that pretreatment with calcium chloride may prevent this hypotensive response. Oshida et al8 studied the effects of calcium chloride on the cardiac effects of verapamil and diltiazem in rat hearts. The study found that calcium significantly counteracted the negative inotropic effects of diltiazem and verapamil but potentiated the negative chronotropic effects of these medications.
Kolkebeck et al4 studied this issue in humans and performed a prospective, randomized, double-blinded, placebo-controlled study to determine if pretreatment with calcium chloride would blunt an SBP drop after the administration of IV diltiazem. Seventy-eight patients with atrial fibrillation/flutter and a ventricular rate of at least 120 bpm were enrolled. Half of these patients received IV calcium chloride as a pretreatment and the other received a placebo. All patients received IV diltiazem in a standard, weight-based dose, and the pretreatment solution was given again if a second dose of diltiazem was required. Kolkebeck et al4 found no statistically significant blunting of a drop in SBP with calcium chloride pretreatment. Furthermore, both groups had an equal decrease in HR that was statistically significant. In addition, there were no adverse events in those patients that were pretreated with calcium chloride.
Given that the use of diltiazem in the prehospital setting is controversial, some have found that using IV diltiazem and electrical cardioversion for the treatment of rapid atrial fibrillation may be unnecessary. Abarbanell et al3 retrospectively reviewed cases of rapid atrial fibrillation over a 12-month period from October 1998 through September 1999 in the low-volume urban EMS system of Evanston, Illinois. They found 33 persons who presented with rapid atrial fibrillation, representing 0.69% of their total prehospital volume, and none of them received IV diltiazem or electrical cardioversion. Nine patients received prehospital treatment consisting of nitroglycerin, furosemide, aspirin, morphine, or IV fluid bolus therapy. The remainder of the patients were treated only with symptomatic/supportive care consisting of observation. All of the patients reported symptomatic improvement after care was provided, regardless of the use of prehospital interventions. In addition, severe hemodynamic instability, cardiac dysrhythmias, iatrogenic complications, or conditions requiring endotracheal intubation were not noted in any of the patients. Accordingly, the authors found that prehospital rapid atrial fibrillation is infrequently encountered, predominantly hemodynamically stable, and readily treatable with symptomatic/supportive care and cautious observation. Consequently, the authors suggest that the use of IV diltiazem and electrical cardioversion in the treatment of prehospital rapid atrial fibrillation may be unnecessary.
Given these various issues and the lack of clear guidance regarding the use of diltiazem in the prehospital setting, it remains a continual challenge to train paramedics on the proper use of the drug. As demonstrated in this study, diltiazem was inappropriately administered in 1 patient who was in ventricular tachycardia instead of atrial fibrillation. Although this instance was the first recorded time that the paramedic administered the drug, we cannot easily determine whether it was his very first administration of the drug because the electronic database was instituted only 1 month before the start date of this study. Nevertheless, this particular medic had been working for approximately 5 years at the time of this incident. Although this study shows that diltiazem is very safe and effective in the prehospital setting, this case of incorrect administration of diltiazem reinforces the need for continuing medical education on rhythm strips, ECGs, and appropriate use of the medication.
LIMITATIONS
The current study has several limitations. First, the ECGs and rhythm strips were not reviewed to ensure that patients treated with diltiazem were in atrial fibrillation. It is possible that some of the patients in the study were in sinus tachycardia, supraventricular tachycardia, or even ventricular tachycardia (as was the case with one of the patients who became hypotensive). Despite this limitation, the study shows how safe and efficacious diltiazem will be in real practice where similar mistakes could be made. Another limitation of the study is that the prehospital system in New Jersey is unique in that all patients treated by prehospital ALS providers need online medical control. Because physicians are directly involved in every decision to give diltiazem, it is possible diltiazem would be given to a different set of patients in other systems. Finally, this study has the same limitations of all retrospective studies, such as reporting errors.
CONCLUSION
Although the use of diltiazem for the treatment of rapid atrial fibrillation in the prehospital setting remains controversial, we found that diltiazem is associated with a very low rate of hypotension and appears to be effective in decreasing HR adequately. We strongly support and advocate for prospective studies to further examine this issue.
Footnotes
Supervising Section Editor: David E. Slattery, MD
Submission history: Submitted December 23, 2010; Revision received May 7, 2011; Accepted August 29, 2011
Full text available through open access at http://escholarship.org/uc/uciem_westjem
DOI: 10.5811/westjem.2011.8.6692
Address for Correspondence: Jeffrey H. Luk, MD, MS, University Hospitals Case Medical Center, Department of Emergency Medicine, 11100 Euclid Ave, BHC 5064, Cleveland, OH 44106. Email: jhlukmd@gmail.com.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Wang HE, O’Connor RE, Megargel RE. The use of diltiazem for treating atrial fibrillation in the out-of-hospital setting. Ann Emerg Med. 2001;37:38–45. et al. [PubMed]
2. Abarbanell NR, Marcotte MA. Prehospital use of intravenous diltiazem (Cardizem Lyo-Ject) in the treatment of rapid atrial fibrillation. Am J Emerg Med. 1997;15:618–619. [PubMed]
3. Abarbanell NR, Marcotte MA, Schaible BA. Prehospital management of rapid atrial fibrillation: recommendations for treatment protocols. Am J Emerg Med. 2001;19:6–9. et al. [PubMed]
4. Kolkebeck T, Abbrescia K, Pfaff J. Calcium chloride before I.V. diltiazem in the management of atrial fibrillation. J Emerg Med. 2003;26:395–400. et al. [PubMed]
5. Zachar B, Graham K, Jaslow D. Prehospital pharmacology: diltiazem. Emerg Med Serv. 2006;35:53–57. [PubMed]
6. Worster A, Bledsoe RD, Cleve P. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45:448–451. et al. [PubMed]
7. Vinson DR, Burke TF, Sung HM. Rapid reversal of life-threatening diltiazem-induced tetany with calcium chloride. Ann Emerg Med. 1999;34:676–678. [PubMed]
8. Oshida J, Goto H, Benson KT. Effect of calcium chloride on verapamil- and diltiazem-pretreated isolated rat hearts. J Cardiothorac Vasc Anesth. 1993;7:717–720. et al. [PubMed]


