| Author | Affiliation |
|---|---|
| Esther K. Choo, MD, MPH | Rhode Island Hospital, Department of Emergency Medicine, Alpert Medical School of Brown University, Providence, RI |
| Craig D. Newgard, MD, MPH | Center for Policy and Research in Emergency Medicine, Department of Emergency Medicine, Oregon Health & Science University, Portland, OR |
| Robert A. Lowe, MD, MPH | Center for Policy and Research in Emergency Medicine, Department of Emergency Medicine, Oregon Health & Science University, Portland, OR |
| Michael K. Hall, MD | University of California, San Francisco, Department of Emergency Medicine, San Francisco, CA |
| K John McConnell, PhD | Center for Policy and Research in Emergency Medicine, Department of Emergency Medicine, Oregon Health & Science University, Portland, OR |
ABSTRACT
Introduction:
Little is known about availability of resources for managing intimate partner violence (IPV) at rural hospitals. We assessed differences in availability of resources for IPV screening and management between rural and urban emergency departments (EDs) in Oregon.
Methods:
We conducted a standardized telephone interview of Oregon ED directors and nurse managers on six IPV-related resources: official screening policies, standardized screening tools, public displays regarding IPV, on-site advocacy, intervention checklists and regular clinician education. We used chi-square analysis to test differences in reported resource availability between urban and rural EDs.
Results:
Of 57 Oregon EDs, 55 (96%) completed the survey. A smaller proportion of rural EDs, compared to urban EDs, reported official screening policies (74% vs. 100%, p=0.01), standardized screening instruments (21% vs. 55%, p=0.01), clinician education (38% vs. 70%, p=0.02) or on-site violence advocacy (44% vs. 95%, p<0.001). Twenty-seven percent of rural EDs had none or one of the studied resources, 50% had two or three, and 24% had four or more (vs. 0%, 35%, and 65% in urban EDs, p=0.003). Small, remote rural hospitals had fewer resources than larger, less remote rural hospitals or urban hospitals.
Conclusion:
Rural EDs have fewer resources for addressing IPV. Further work is needed to identify specific barriers to obtaining resources for IPV management that can be used in all hospital settings.
INTRODUCTION
Intimate partner violence (IPV) includes any pattern of assaultive and coercive behaviors, including physical injury, psychological abuse, sexual assault, social isolation, stalking, deprivation, intimidation or threats perpetrated by someone who was or is in an intimate relationship with the victim.1 It occurs in an estimated two million United States (U.S.) women each year and 26% of U.S. women over their lifetime.2,3 However, partner violence is even more common among individuals visiting the emergency department (ED) for care; estimates range from past-year prevalence of 12 to 19% and lifetime prevalence of 44 to 54%.4–8
The prevalence of IPV in rural settings appears to be similar to that in non-rural settings.9–12However, in rural areas, geographic and economic barriers to seeking healthcare are often greater and alternatives for follow up and referrals may be limited.13,14 Therefore, the ED visit may be particularly important as an opportunity to identify and comprehensively address IPV. The objective of this study was to assess differences in IPV resource availability between urban and rural EDs.
METHODS
Study Design
We conducted the study among ED directors and managers at all of Oregon’s 57 hospitals, using a standardized telephone survey. We targeted ED physician directors and ED nurse managers, reasoning that these individuals would be responsible for and knowledgeable of the protocols and services in use in the ED. We merged survey data with hospital-level variables from the Office for Oregon Health Policy and Research and the Oregon Office of Rural Health. The Institutional Review Board of the study institution approved this protocol.
Study Setting and Population
Oregon has an estimated population of 3.8 million people. Fifteen rural areas in Oregon are defined as geographic areas 10 or more miles from the centroid of a population center of 40,000 or more, while frontier counties are those with less than six people per square mile.16 Approximately 26% of the Oregon population lives in rural or frontier counties and 54% in mixed urban and rural counties; the rest (20%) live in one of six urban areas. Of Oregon’s 57 acute care hospitals, 35 are classified as rural.16
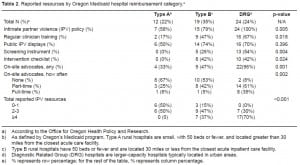
An additional framework for understanding the needs and resources of the acute care hospitals is provided by Oregon’s Medicaid program, which reimburses hospitals according to one of three categories, based on hospital capacity (inpatient bed size) and remoteness (distance from nearest acute inpatient care facility).17 Type A rural hospitals are small, with 50 beds or fewer, and are located greater than 30 miles from the closest acute care facility. Type B rural hospitals also have 50 beds or fewer but are located 30 miles or less from the closest acute inpatient care facility. Diagnostic Related Group (DRG) hospitals, which receive a fixed payment for each patient based on the DRG to which the patient is assigned, are larger-capacity hospitals typically located in urban areas; only three DRG hospitals are classified as rural.
Measurements
To measure availability of IPV resources, we adapted survey questions from the “Delphi Instrument for Hospital-Based Domestic Violence Programs” developed by the Agency for Healthcare Research and Quality (AHRQ).18 To optimize participation, we limited our survey to six questions addressing policies and procedures relevant to the ED setting (Figure 1). The survey was pilot tested among ED staff unaffiliated with the study and revised based on their feedback prior to administration elsewhere.
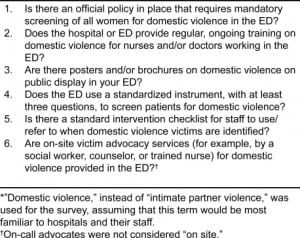
The survey was administered by telephone to ED directors and nurse managers over a one-month period from September to October 2008. A single individual was interviewed at each site. Respondents were asked to answer “Yes” or “No” to the availability of each of the resources. The full survey included three additional questions about ED resources for the management of child abuse; these results were reported separately.19 The survey took approximately five minutes to complete.
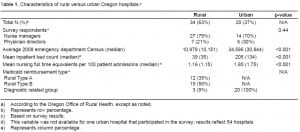
We obtained hospital-level variables, including urban/rural designation, annual ED census, bed size, trauma capabilities and a nurse staffing score, from the Office for Oregon Health Policy and Research.20,21 The nurse staffing score represents the number of nursing full time equivalents (FTE) for every 100 hospital admissions and was included to reflect available hospital human resources. The distribution of these characteristics between urban and rural locations is shown in Table 1.
Statistical Analysis
We used frequencies and proportions to characterize the reported availability of IPV resources among the surveyed EDs. Differences in the proportion of rural and urban EDs reporting individual resources were evaluated using univariate (Pearson’s chi-square) analysis. We examined the advocacy variable both as a dichotomous variable (present or not present) and as a categorical variable (not present, part-time, or full-time). We also examined differences between rural and urban EDs with respect to total number of IPV resources (0–1, 2–3, ≥4) using chi-square analysis.
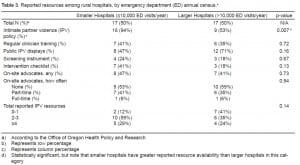
To see if resource availability was related not just to rural / urban designation but also to factors such as hospital capacity and remoteness, we repeated analyses using the Medicaid reimbursement categories (DRG hospitals versus Type A and Type B hospitals). Finally, to address whether resource availability was related to higher ED volume – with presumably higher numbers of IPV cases – among rural hospitals, we compared resources reported and between larger (>10,000 vists/year) and smaller (<10,000/year) ED census.
We defined statistical significance as a probability of a type I error of less than 5% (2-tailed). Analyses were conducted using Stata, version 10.1 (StataCorp LP, College Station, TX).
RESULTS
Fifty-five of 57 EDs (96%) participated in the survey, with 13 physician directors and 42 nurse managers responding. The director and nurse manager of one hospital could not be reached, and one ED declined participation. Table 1 compares characteristics of rural and urban hospitals. Thirty-four (63%) of the participating hospitals are classified as rural.
Figure 2 shows reported resource availability by practice setting. In univariate analysis, a smaller proportion of rural hospitals reported official IPV screening policies (p=0.01), standardized screening instruments (p=0.01), regular clinician training (p=0.02), and on-site IPV advocates (<0.001). Urban EDs more often reported availability of full-time on-site advocates than rural EDs (38% vs 6%, p<0.001). Use of public displays regarding IPV and standardized intervention checklists was greater in urban settings, although these differences were not statistically significant.
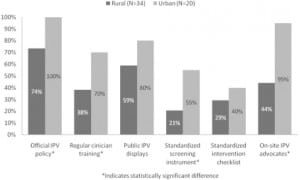
The total number of available IPV services differed significantly between urban and rural EDs (Figure 3) as well. Twenty-seven percent of rural services reported none of the six resources examined, while all urban hospitals reported two or more IPV resources and 65% had four or more (p=0.003).
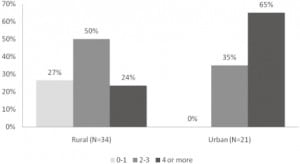
Results based on reimbursement category are shown in Table 2. For every resource except use of public displays, a smaller proportion of Type A hospitals reported resource availability than Type B hospitals, and a smaller proportion of Type B hospitals reported resource availability than DRG hospitals. Fifty percent of Type A hospitals reported none of the examined resources, while all DRG hospitals reported at least two resources and 70% had four or more (p= <0.001).
In the comparison of hospitals by annual ED census, the only resource with a statistically significant difference was a written IPV policy, which was reported more frequently among hospitals with an annual ED census less than 10,000.
DISCUSSION
We describe differences in the reported availability of IPV resources between urban and rural EDs. Overall, rural EDs seem to have fewer resources to address partner violence, with less reported availability of all six types of studied IPV resources and fewer total number of IPV resources. Comparison of reported resource availability based on hospital reimbursement categories suggests that resource limitations were exacerbated by factors such as small size and remoteness. However, we did not find a correlation between ED volume and number of resources reported. It seems unlikely, therefore that need (i.e., number of IPV cases encountered) is what dictates availability of services.
In 1992, the Joint Commission (formerly known as the Joint Commission on the Accreditation of Healthcare Organizations, or JCAHO) defined basic standards for hospital policies and procedures to increase the identification of IPV within EDs and hospital-based ambulatory care centers.22 Updated in 2004, the standards include maintenance of specific criteria for identifying victims of IPV, identification of victims upon entry into the healthcare system (e.g., at ED triage), education of staff about the management of IPV, and appropriate assessment and referrals by staff. These recommendations are uniform for all hospitals and do not acknowledge potential resource differences between rural and urban hospitals, or hospitals of varying sizes.
There are a number of potential solutions to resource limitation in rural areas. Resources such as IPV management guidelines or patient educational posters and pamphlets are relatively inexpensive to develop and use, particularly with the increasing availability of free or low-cost materials from non-profit domestic violence groups and medical societies.23,24 Existing leadership and continual medical education activities may be modified to include material on IPV and to emphasize skills that will allow individuals to train others within their institution. Statewide or county-wide collaborations may allow rural institutions to benefit from a variety of educational, research and community initiatives related to the management of IPV.25 State and national hotlines are available 24/7 for counseling patients experiencing IPV. Telemedicine is providing intriguing new possibilities for counseling victims of IPV in rural locations.26
LIMITATIONS
Resource availability was determined by the responses of surveyed ED staff. The studied resources may have been mistakenly reported as present when absent or reported as absent when actually present. Further, a resource may be technically present but not provided to patients meaningfully; for example, a written policy may exist but would have little effect on patient care if it was rarely referred to or if there was no quality assurance process to make sure it was adhered to rigorously. On the other hand, it may be that an ED does not have a formal policy in place yet in practice still delivers a service well. Our study was not able to measure actual ED practices.
Our findings may also be limited by recall bias. ED representatives may have been more likely to report having resources when unsure, particularly if they were aware that specific IPV resources are mandated for hospitals by the Joint Commission. Further, as a non-anonymous survey, respondents may not have felt free to answer honestly. However, there is no reason over-reporting or under-reporting of resources should have occurred differentially between rural and urban sites, so this bias, if present, would not explain our findings.
Because our study was limited to the state of Oregon, the findings may not be generalizable to the entire U.S. Oregon does not require reporting of IPV unless a weapon was used to inflict an injury. States without reporting requirements may have different resource utilization than those with these requirements. The hospitals surveyed did represent a broad range of practice settings, with varying bed and staff sizes and trauma capabilities, so are likely to be relevant to a broad range of practice types.
CONCLUSION
Rural EDs in our study reported limited resources for IPV management compared to urban EDs. Further research is needed to identify specific barriers to obtaining IPV resources. At the same time, further cost-effective means of improving the initial assessment and care of IPV victims in the ED should be identified and developed.
Footnotes
Supervising Section Editor: Michael Menchine, MD, MPH
Submission history: Submitted January 14, 2010; Revision received May 7, 2010; Accepted July 26, 2010
Reprint available through open access at http://scholarship.org/uc/uciem_westjem.
Address for Correspondence: Esther K. Choo, MD, MPH, Rhode Island Hospital, Warren Alpert Medical School of Brown University, 593 Eddy Street, Claverick 2, Providence, RI 02903.
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Preventing Domestic Violence: Clinical Guidelines on Routine Screening. Family Violence Prevention Fund; San Francisco, CA: 1999.
2. Black M, Breiding M. Adverse Health Conditions and Health Risk Behaviors Associated with Intimate Partner Violence — United States, 2005. MMWR, National Center for Injury Prevention and Control, Centers for Disease Control; [February 6, 2008. Accessed March 1, 2010.
3. Errata: Vol 57, No 5. MMWR, National Center for Injury Prevention and Control, Centers for Disease Control March 5, 2008. Accessed March 1, 2010.
4. El-Bassel N, Gilbert L, Krishnan S, et al. Partner violence and sexual HIV-risk behaviors among women in an inner-city emergency department. Violence Vict. 1998;13(4):377–93. [PubMed]
5. Dearwater SR, Coben JH, Campbell JC, et al. Prevalence of intimate partner abuse in women treated at community hospital emergency departments. JAMA. 1998;280(5):433–38. [PubMed]
6. Abbott J, Johnson R, Koziol-McLain J, Lowenstein SR. Domestic violence against women: Incidence and prevalence in an emergency department population. JAMA. 1995;273(22):1763–67.[PubMed]
7. Ernst AA, Nick TG, Weiss SJ, et al. Domestic violence in an inner-city ED. Ann Emerg Med.1997;30(2):190–97. [PubMed]
8. Brokaw J, Fullerton-Gleason L, Olson L, et al. Health status and intimate partner violence: a cross-sectional study. Ann Emerg Med. 2002;39(1):31–38. [PubMed]
9. Coker AL, Flerx VC, Smith PH, et al. Intimate partner violence incidence and continuation in a primary care screening program. Am J Epidemiol. 2007;165(7):821–7. [PubMed]
10. Van Hightower NR, Gorton J. Domestic violence among patients at two rural health care clinics: prevalence and social correlates. Public Health Nurs. 1998;15(5):355–62. [PubMed]
11. Breiding MJ, Ziembroski JS, Black MC. Prevalence of rural intimate partner violence in 16 US states, 2005. J Rural Health. 2009;25(3):240–6. [PubMed]
12. Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Womens Health Issues. 2004;14(1):19–29. [PubMed]
13. Bushy A. Health issues of women in rural environments: an overview. J Am Med Womens Assoc.1998;53(2):53–56. [PubMed]
14. Iyengar R, Sabik L. The dangerous shortage of domestic violence services. Health Aff (Millwood)2009;28(6):w1052–65. [PubMed]
15. Proehl RS. Oregon Population Report. Portland, OR: Population Research Center, Portland State University; 2008. 2009.
16. Oregon Office of Rural Health Rural Hospitals. http://www.ohsu.edu/xd/outreach/oregon-rural-health/data/rural-definitions/index.cfm. Accessed December 7, 2009.
17. Oregon Office of Rural Health http://www.ohsu.edu/xd/outreach/oregon-rural-health/hospitals/index.cfm. Accessed January 5, 2010.
18. Evaluating Domestic Violence Programs http://www.ahrq.gov/research/domesticviol/. Accessed August 1, 2008.
19. Choo EK, Spiro D, Newgard CD, et al. Urban Disparities in Child Abuse Management Resources in the Emergency Department. J of Rural Health. In press.
20. DataBank 2008. http://www.oregon.gov/OHPPR/RSCH/databank.shtml. Accessed March 1, 2010.
21. 2009. Oregon’s Acute Care Hospitals: Capacity, Utilization and Financial Trends: Office for Oregon Health Policy and Research.
22. Flitcraft A. Physicians and domestic violence: challenges for prevention. Health Aff.1993;12(4):154–61.
23. American Congress of Obstetricians and Gynecologists: Screening Tools–Domestic Violence.http://www.acog.org/departments/dept_notice.cfm?recno=17&bulletin=585. Accessed January 11, 2009.
24. Family Violence Prevention Fund: Health Practitioner Toolshttp://fvpfstore.stores.yahoo.net/healpractool.html. Accessed January 11, 2009.
25. Illinois Family Violence Coordinating Councils http://www.ifvcc.org/. Accessed November 25, 2009.
26. Thomas CR, Miller G, Hartshorn JC, Speck NC, Walker G. Telepsychiatry program for rural victims of domestic violence. Telemed J E Health. 2005;11(5):567–73. [PubMed]


