| Author | Affiliation |
|---|---|
| Zeynal Karaca, PhD | Social and Scientific Systems, Inc., Silver Spring, MarylandAgency for Healthcare Research and Quality, Rockville, Maryland
George Washington University, Health Policy Department, Washington, DC |
| Herbert S. Wong, PhD | Agency for Healthcare Research and Quality, Rockville, Maryland |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
Abstract
Introduction:
The sources of racial disparity in duration of patients’ visits to emergency departments (EDs) have not been documented well enough for policymakers to distinguish patient-related factors from hospital- or area-related factors. This study explores the racial disparity in duration of routine visits to EDs at teaching and non-teaching hospitals.
Methods:
We performed retrospective data analyses and multivariate regression analyses to investigate the racial disparity in duration of routine ED visits at teaching and non-teaching hospitals. The Healthcare Cost and Utilization Project (HCUP) State Emergency Department Databases (SEDD) were used in the analyses. The data include 4.3 million routine ED visits encountered in Arizona, Massachusetts, and Utah during 2008. We computed duration for each visit by taking the difference between admission and discharge times.
Results:
The mean duration for a routine ED visit was 238 minutes at teaching hospitals and 175 minutes at non-teaching hospitals. There were significant variations in duration of routine ED visits across race groups at teaching and non-teaching hospitals. The risk-adjusted results show that the mean duration of routine ED visits for Black/African American and Asian patients when compared to visits for white patients was shorter by 10.0 and 3.4%, respectively, at teaching hospitals; and longer by 3.6 and 13.8%, respectively, at non-teaching hospitals. Hispanic patients, on average, experienced 8.7% longer ED stays when compared to white patients at non-teaching hospitals.
Conclusion:
There is significant racial disparity in the duration of routine ED visits, especially in non-teaching hospitals where non-White patients experience longer ED stays compared to white patients. The variation in duration of routine ED visits at teaching hospitals when compared to non-teaching hospitals was smaller across race groups.
INTRODUCTION
A number of studies have addressed racial disparities across healthcare settings.1–10 The literature documents that Blacks/African Americans experience reduced access to regular health care due to lower rates of health insurance coverage, poorer access to primary care, and more frequent use of emergency departments (EDs).4 And once they have entered the healthcare system, the quality of care for Blacks has been found to be lower than for Whites.11–12 Several studies concluded that poorer health outcomes could be due to lower-quality hospital care and a lower likelihood of receiving specific indicated interventions.13–17 The sources of racial disparity in EDs have not been documented well enough for policymakers to distinguish patient-related factors from hospital- or area-related factors.
The hospital ED is a primary portal of entry into the healthcare system for many Americans. Length of stay (LOS) is generally perceived as an important indicator of quality of care in EDs.18 Increased LOS at EDs may contribute to systematic problems in the delivery of efficient and high quality medical care in the U.S. Increased LOS may also mean patients wait longer to see ED physicians and to obtain critical treatments and test results. 19,20 Several studies have documented that extended LOS is usually due to evaluation time by a physician for critical testing, treatment, and bed placement.21 Variation in ED LOS provides a good opportunity to study racial disparity because it is affected by a number of complex public health and healthcare facility-related issues. One study showed that disparities in waiting times exist in emergency care and that black patients wait longer to see emergency physicians than white patients.22 A few studies used the National Hospital Ambulatory Medical Care Survey to document racial disparity in ED LOS for admitted patients.23–26 Several studies in the literature found no evidence of racial or ethnic disparity in use of emergency care or in ED LOS.27–29
The objective of this study was to determine whether racial disparities in duration of ED visits exist at teaching and non-teaching hospitals. ED visits for this study are limited to routine visits in which the patients are discharged for home or self care. This study contributes to the existing literature in the following important ways: First, existing studies examining racial disparity in ED LOS and general resource use employ data drawn from a sample of ED visits obtained from a survey or tracked as part of a before-and-after intervention study.30 One of the largest of these data files is a nationally representative sample of 138,569 ED visits over a 5-year period.20 In contrast, our data file includes 4.3 million ED visits in a single year. Healthcare policies designed to provide solutions to increased ED LOS, ED crowding, and related issues may produce better outcomes when they are based on these large data sets. Such large databases may also shed light on the wide variations in use patterns of ED services and the significant differences in patient-related and area-specific factors.31 Second, our findings may inform public and private policymakers on a broad range of issues, including, but not limited to, the variation in duration of routine ED visits by patient race group, age, gender, insurance coverage, and disease category; by hospital bed size, location, system membership, trauma center classification, and ownership status; and by geographic income distribution. Third, our study is also the first, to our knowledge, addressing racial disparity in ED LOS by hospital type. We compare the duration of routine ED visits across race groups in teaching and non-teaching hospitals, as the former generally treat more severe or clinically complex patients compared to the latter. Finally, this study further contributes to the existing literature by addressing several important factors affecting ED LOS,32–41 i.e., hospital ED visit volume and ED admission day of the week.
METHODS
Study Design and Population
We performed retrospective data analyses and multivariate regression analyses to investigate the racial disparity in the duration of routine ED visits that were discharged for home or self care using the Healthcare Cost and Utilization Project (HCUP)1 State Emergency Department Databases (SEDD) for 2008. HCUP is maintained by the Agency for Healthcare Research and Quality (AHRQ). The SEDD employed in this study include data on 4.3 million routine ED visits in 3 states: Arizona, Massachusetts, and Utah. In general, the SEDD provide detailed diagnoses, procedures, total charges, and patient demographics. Demographics include gender, age, race, and insurance coverage (i.e., Medicare, Medicaid, private insurance, other insurance, and uninsured). However, the SEDD from these 3 states also provide admission and discharge time for each visit, from which duration2 may be calculated.
We obtained information about hospital characteristics (i.e., urban versus rural, ownership status, teaching status, bed size, and system membership) from the 2008 American Hospital Association Annual Survey Database and linked that data to SEDD files using hospital identifiers. In addition, we obtained information about the trauma level of the hospital using the Trauma Information Exchange Program database, collected by the American Trauma Society and the Johns Hopkins Center for Injury Research and Policy. Finally, we used the 2008 Area Resource File3 to obtain county-level income information.
A value for ED LOS is not readily available in our data. We computed the duration for each visit by taking the difference between admission and discharge times, which is the time patients waited in ED rooms plus their treatment time (the time spent with doctors).32 Our measure of duration does not include boarding time because our ED data file includes information for only treat-and-release patients, not admitted ones. Therefore, we do not believe that the lack of separable ED LOS measures (i.e., waiting room time and treatment time) compromises our results because we use the same measures of ED LOS for all race groups within each hospital. More specifically, we assume that ED treatment time for patients with the same clinical conditions, age, and gender are similar regardless of their race groups. However, there might be some variation in ED waiting room time within and across hospitals. Our analytic approach addresses this issue. Hence, if we document that there is racial disparity in duration of ED visits as defined above, we can attribute that disparity mostly to ED waiting room time because our multivariate analysis of ED duration, explained in detail below, controls for the severity of clinical cases and other socio-economic characteristics which are typically responsible for any significant variation in actual treatment times.
Statistical Analyses
We started with extensive secondary data analyses by patient, hospital, and area characteristics to explore racial disparity in the duration of routine ED visits at teaching and non-teaching hospitals separately. ED duration is expressed in minutes, measured as the difference between admission time and discharge time.4 The mean (median) duration for a specific admission hour was measured as the mean (median) value of the durations of all routine ED visits at that specific hour during 2008. We applied a similar approach when reporting the mean duration of ED visits across patient demographics and hospital characteristics. For example, the mean duration of ED visits for female patients was measured as the total duration of routine ED visits by all female patients divided by the total number of routine ED visits by female patients during 2008. We analyzed data with SAS 9.02 and Stata 12.
Severity of illness is an important factor that can affect the mean duration of ED visits. To further explore the potential relationship between the mean duration of visits and various disease groups, we grouped ED visits into major disease categories based on Clinical Classification Software—a diagnosis and procedure categorization scheme based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). While the HCUP SEDD provide all diagnosis codes for every visit, they do not always clearly differentiate between the primary diagnosis codes and other diagnosis codes. Therefore, we used all diagnosis codes reported for each visit when developing our major disease categories.
Next, we developed a flexible functional linear model that controls for patient demographics and hospital and area characteristics to assess racial disparity in duration of routine ED visits at teaching and non-teaching hospitals. More specifically, we estimated several regression models using the natural log value of the duration5 as the dependent variable to examine factors associated with the duration of patients’ routine ED visits. We estimated a linear regression model that controls for: 1) patient characteristics including race group, age, gender, insurance coverage, and major disease categories; 2) hospital characteristics including bed size, location, membership in a large hospital system, trauma center classification, and ownership status; 3) geographic income distribution measured by median household income in patient’s residence ZIP code; and 4) admission day of the week and average volume at the ED 1 hour before the admission hour.
We tested our flexible linear models for the undesirable presence of multicollinearity (i.e., a linear relationship among predictor variables) and heteroskedasticity (i.e., variance of the error terms correlated with 1 or more explanatory variables). We saw no evidence of multicollinearity in the correlation coefficients of the predictor variables, and we corrected the heteroskedasticity we identified using Huber-White sandwich estimators to obtain robust standard errors and variance estimates.42 We further estimated our linear model using robust regression methods to assess the validity of our results based on the linear model.43–46 More specifically, we ran robust regressions using iteratively reweighted least squares, that is, we assigned a weight to each observation, with higher weights given to better-behaved observations.
RESULTS
Descriptive Results
Patient Characteristics
We began our analysis with a descriptive comparison of duration of routine ED visits across race groups to profile the differences by age, gender, insurance coverage, and disease category. We analyzed patient demographics to explore potential explanations for the racial disparity we observed. Table 1 displays the total number of routine ED visits and mean and median duration of visits for various patient characteristics at both teaching and non-teaching hospitals. As shown in Table 1, the mean duration of visits6 ranged from 223 to 245 minutes at teaching hospitals, and 173 to 189 minutes at non-teaching hospitals across race groups. The mean duration increased with the age of the patient regardless of the teaching status of the hospitals. We also observed longer mean duration of routine ED visits for female patients when compared to male patients across race groups within each hospital setting.
Next, we analyzed the mean duration of routine ED visits by insurance coverage for each race group at both teaching and non-teaching hospitals. We found that Medicare patients’ visits had the longest mean duration (278 minutes at teaching hospitals and 213 minutes at non-teaching hospitals), which could be due to higher severity of illness and presence of multiple diseases among these patients. Table 1 shows that the mean duration of routine ED visits by white, black/African American, Hispanic, and Asian Medicare patients visiting teaching hospitals (non-teaching hospitals) was 280, 268, 280, and 300 (209, 241, 242, and 255) minutes, respectively. Table 1 also shows that the mean duration of routine ED visits by white, black/African American, Hispanic, and Asian patients with Medicaid coverage, at teaching hospitals (non-teaching hospitals) was 228, 201, 214, and 205 (159, 170, 164, and 185) minutes, respectively. For those without insurance coverage, the mean duration of routine ED visits by white, Black/African American, Hispanic, and Asian patients at teaching hospitals (non-teaching hospitals) was 241, 213, 251, and 243 (163, 187, 187, and 191) minutes, respectively. These results suggest that there is no sizable difference in mean duration of ED visits between patients with any insurance coverage and uninsured patients.
Severity of illness is an important factor that can affect the mean duration of ED visits. To further explore the potential relationship between the mean duration of visits and various disease categories, we grouped ED visits into major disease categories based on Clinical Classification Software. We used all diagnosis codes reported for each visit when developing our major disease categories. As presented in Table 1, routine ED visits for neoplasm; endocrine, nutritional, and metabolic diseases and immunity disorders, diseases of blood and blood forming organs, and mental disorders are associated with longer mean duration across all race groups regardless of hospital teaching status; routine ED visits for diseases of the skin and subcutaneous tissue, certain conditions originating in the perinatal period, and injury and poisoning were generally associated with shorter duration of ED visits at both teaching and non-teaching hospitals.
Hospital and Area Characteristics
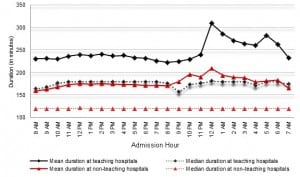
Next, we analyzed hospital and area characteristics to explore other potential factors associated with longer ED visits for each race group. Figure 1 shows that mean duration of ED visits at teaching hospitals is consistently longer when compared to non-teaching hospitals. Table 2 further shows that hospitals with large bed size7 were associated with the longest duration of visits (279 minutes at teaching and 191 minutes at non-teaching hospitals) when compared to hospitals with small bed size (207 minutes at teaching and 161 minutes at non-teaching hospitals) or medium bed size (173 minutes at teaching and 161 minutes at non-teaching hospitals). White patients had longer ED stays when compared to black/African American, Hispanic, and Asian patients at teaching hospitals regardless of hospital bed size. In contrast to the pattern at teaching hospitals, white patients generally experienced shorter ED stays at non-teaching hospitals regardless of bed size. Table 2also shows that the mean duration of routine ED visits at urban teaching hospitals was 67 minutes longer than at their urban non-teaching counterparts. The mean duration of routine ED visits encountered by white patients was longer by 22, 10, and 10 minutes (shorter by 13,14, and 16 minutes), respectively, when compared to the mean duration of routine ED visits encountered by black/African American, Hispanic, and Asian patients at urban teaching hospitals (urban non-teaching hospitals). We found that non-teaching hospitals generally serve rural areas and the mean ED duration of all routine visits at these hospitals was 164 minutes, with some variation across race groups. Recognizing the differences in income levels across geographic regions, we compared the mean duration based on income distribution. In general, we did not find significant differences in mean duration of routine ED visits between relatively richer or poorer counties. Akin to previous results, white patients generally had longer ED stays at teaching hospitals and had slightly shorter ED stays at non-teaching hospitals when compared to other race groups regardless of geographic income distribution. We also observed that the mean duration of routine ED visits at teaching hospitals (non-teaching hospitals) that were members of a hospital system was 40 (25) minutes longer when compared to non-system-member teaching hospitals (non-teaching hospitals). Similarly, the mean duration of visits at Level 1 trauma centers was 269 minutes and substantially longer than those at Level 2 or Level 3 trauma centers, or at non-trauma centers at teaching hospitals. We also found that the mean duration of routine ED visits at Level 1 trauma centers when compared to Level 2 and Level 3 trauma centers or to non-trauma centers at non-teaching hospitals was longer by 81, 85, and 38 minutes, respectively.8 Finally, we found that the mean duration of visits at public, non-profit, and for-profit teaching hospitals was 194, 248, and 217 minutes, respectively, showing significant differences between for-profit and non-profit hospitals. We observed similar but smaller variation between public, non-profit, and for-profit non-teaching hospitals possibly due to differing financial incentives.
Risk-adjusted Results
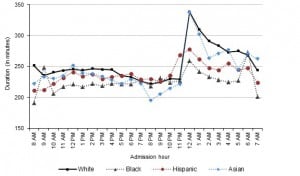
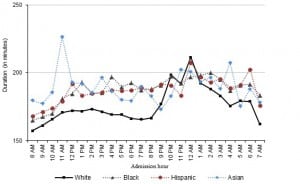
Table 3 presents the regression coefficients9 of our linear model estimated separately for teaching and non-teaching hospitals. The empirical estimates show that the mean duration of routine ED visits encountered by black/African American and Asian patients at teaching hospitals (non-teaching hospitals) were, respectively, 10.0 and 3.4% lower (3.6 and 13.8% higher) than the mean duration of routine ED visits encountered by white patients. The difference in mean duration of routine ED visits at teaching hospitals between Hispanic and white patients were not statistically significant. However, Hispanic patients, on average, experienced an 8.7% longer duration of ED visit when compared to white patients at non-teaching hospitals. These risk-adjusted results parallel our descriptive results, indicating that white patients, when compared to non-white patients, generally have longer ED stays at teaching hospitals (Figure 2) but shorter ED stays at non-teaching hospitals (Figure 3). Our results also support the findings of a previously published study19 that found longer ED LOS for Black/African American non-Hispanic patients (10.6% longer) and Hispanic patients (13.9% longer) when compared to non-Hispanic white patients.
We also obtained valuable information associated with patients’ ED stays in general. The regression results show that the mean duration of routine ED visits for female patients was 5.4 and 4.9% longer than for male patients at teaching and non-teaching hospitals, respectively. The regression results also show that the mean duration of ED visits increases with patient age both at teaching and non-teaching hospitals. Our risk-adjusted results also suggest that uninsured patients generally have shorter ED stays when compared to Medicare enrollees. We also found significant variation in mean duration of routine ED visits across disease categories. Our risk-adjusted results were mostly parallel to our descriptive results (Table 1) indicating that patients diagnosed with neoplasm, endocrine, nutritional, and metabolic diseases and immunity disorders, diseases of blood and blood forming organs, and mental disorders generally experienced longer ED stays when compared to patients diagnosed with other conditions both at teaching and non-teaching hospitals.
Table 3 also presents the estimated effects of hospital characteristics on mean duration of routine ED visits. The results suggest that the mean duration of routine ED visits was higher at for-profit teaching hospitals and lower at for-profit non-teaching hospitals when compared to their respective cohorts of teaching and non-teaching public hospitals. Patients at teaching hospitals with large bed size have ED stays about twice as long as patients at teaching hospitals with small bed size. The mean duration of ED stays at non-teaching hospitals with large bed size was only 7.5% longer than the mean duration of ED stays at non-teaching hospitals with small bed size. We also found that the mean duration of routine ED visits at Level 1 trauma centers was significantly longer than those at non-trauma centers regardless of the hospital teaching status. Additionally, we obtained crucial information regarding how admission day of the week and hospital volume affect the mean duration of routine ED visits. Our risk-adjusted results in Table 3 show that the mean duration of ED visits at teaching hospitals (non-teaching hospitals) was 4.1% (3.7%) longer on Mondays and 5.9% (4.1%) shorter on other weekdays when compared to the mean duration of ED visits on weekends. We also found a positive correlation between longer ED stays and the number of patients present at the ED prior to admission time both at teaching and non-teaching hospitals.
DISCUSSION
This analysis, based on a very large data set, reveals considerable variation in duration of routine ED visits across race groups at teaching and non-teaching hospitals. We computed the duration of each visit by taking the difference between admission and discharge times, which is the total time patients waited in ED rooms plus their treatment time. We documented racial disparity in duration of ED stays both at teaching and non-teaching hospitals. We found that white patients generally have shorter ED stays at teaching hospitals and longer ED stays at non-teaching hospitals when compared to non-white patients. These findings provide robust evidence of racial disparity, especially in non-teaching hospitals, that may be used by decision makers in both public and private healthcare arenas to improve the timeliness of the care provided in the ED and to understand the factors causing the racial disparity.
Some of our results are consistent with the characterization in the literature of care provided in the ED and are expected.22,23 Level 1 trauma centers, for example, have comprehensive resources and are able to care for the most severely injured patients. One plausible explanation for longer ED stays is that Level 1 trauma centers provide the highest level of surgical care to seriously injured patients who may use more resources and whose treatments last longer. It is also plausible to assume that most Level 1 trauma centers provide leadership in education and research. We found that the mean duration of routine ED visits at non-trauma centers are longer than at Level 2 or Level 3 trauma centers, but it is not clear why.
Another important finding of our study is pertinent to uninsured patients. We found that the duration of routine ED visits encountered by uninsured patients are about the same as the mean duration of routine ED visits by all patients. More precisely, the mean duration of all routine ED visits was 238 and 175 minutes, respectively, at teaching and non-teaching hospitals, whereas the mean duration of ED stays encountered by uninsured patients was 239 and 171 minutes at their respective hospitals. We further found that the difference in mean duration of ED visits between uninsured patients and others is not sizable across race groups at either teaching or non-teaching hospitals. It is plausible to assume that both uninsured and insured patients receive similar quality of care once they are admitted to the ED and that both cohorts could face similar barriers to healthcare access at hospital EDs.
Some of these findings are worthy of further exploration. For example, we believe that since elderly patients frequently present to the ED with multiple complications, they require more ED resources during their visits, which causes them to have longer duration of visits. Similarly, we found that race is correlated with increase in duration of ED visits. When this race correlation is associated with a lower socio-economic status, some policymakers may choose to use interpreters, or perhaps social workers, to work with patients to increase their access to primary care and thereby decrease their use of the ED for non-emergency complaints.
LIMITATIONS
We computed the duration of each visit by taking the difference between admission and discharge times, which yields the total time patients waited in ED rooms plus their treatment time. Our measure of duration, unfortunately, does not separate waiting time and treatment time.
The data in the HCUP SEDD are based on ED encounters as the unit of analysis. Therefore, a given patient may have many visits represented in the data. As a result, the summary information reported under patient characteristics might overestimate or underestimate demographics for individual patients. This study also does not address the impact of financial incentives and other confounding factors across hospitals types on duration of ED visits.
Our analysis is confined to the routine ED visits presented in the HCUP SEDD. ED encounters that result in subsequent admission to the same hospital are not included in the analysis. Therefore, the relative number of patients admitted at the individual EDs may compromise this analysis as their presence may limit the resources available to patients on routine ED visits.
CONCLUSION
Our results show that the mean duration for a routine ED visit was 238 minutes at teaching hospitals and 173 minutes at non-teaching hospitals. When documenting the mean duration, we uncovered a significant racial disparity in mean duration of ED visits at non-teaching hospitals. Based on patient demographics and hospital characteristics, we identified several important factors that are associated with increased ED stays. We identified a direct relationship between increased duration of ED visits and patient race, age, gender, and severity of illness; and hospital location and ownership status. We observed substantial variation in mean duration of ED visits by race group between teaching and non-teaching hospitals. The mean duration of ED visits at teaching hospitals (non-teaching hospitals) for White, Black/African American, Hispanic, and Asian patients was 245, 223, 234, and 235 (173, 187, 186, and 189) minutes respectively. Our risk-adjusted findings show that the mean duration of ED visits for Black/ African American and Asian patients was 10.0 and 3.4% lower (3.6 and 13.8% higher), respectively, than the mean duration of routine ED visits encountered by white patients at teaching hospitals (non-teaching hospitals). The mean duration of ED visits for Hispanic patients was 8.7% longer at non-teaching hospitals when compared to white patients. We did not find any disparity in duration of ED visits at teaching hospitals between white and Hispanic patients. We also found that female patients generally experienced longer ED stays than male patients. Elderly patients and patients diagnosed with neoplasm, endocrine, nutritional, and metabolic diseases and immunity disorders, diseases of blood and blood forming organs, and mental disorders generally experienced longer ED stays than did other patients. Consistent with the existing literature, our results suggest that, in the aggregate, lack of health insurance did not have a significant direct association with longer mean duration of ED visits. The mean duration of ED visits was substantially longer at non-profit hospitals when compared to for-profit hospitals, and at Level 1 trauma centers when compared to other trauma centers or non-trauma centers. Our findings may also inform public and private policymakers on a broad range of issues including, but not limited to, admission day of the week, hospital volume, and the impact of hospital bed size on the mean duration of ED visits.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Further details about HCUP databases are available at http://hcup-us.ahrq.gov/.
Some data elements, such as admission times and discharge times, are considered too sensitive by HCUP data organizations for general release to public. However, we received special permission to have access to these more sensitive data for analysis. In this study, the Arizona Department of Health Services, the Massachusetts Division of Health Care Finance and Policy, and the Utah Department of Health granted permission for the admission hour and discharge hour data elements.
The Area Resource File (ARF) provides county-level data. Further details are available at http://arf.hrsa.gov/.
Ideally, ED waiting time would be deconstructed into waiting room, treatment, and boarding times experienced by ED patients. However, in our data, we can only observe the total length of stay in the ED for each visit.
Because the distribution of duration of ED visits was skewed, the natural logarithm of ED duration was used as the dependent variables for the analysis.
We focus mainly on the mean value of duration in our analysis. However, we have provided both mean and median values for each measure separately throughout all tables and figures to set the stage for further research and to provide additional detail to key policymakers and interested researchers.
Further details about hospital bed sizes are available at: http://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp.
Trauma level designation was based on American College of Surgeons or state-specific designation. We found most of the trauma Level 1 centers within teaching hospitals. Less than 2 percent of them were located within non-teaching hospitals. While we were expecting all of them to be located within teaching hospitals, we still report the results assuming the possibility of having Level 1 trauma centers located within non-teaching hospitals.
Address for Correspondence: Zeynal Karaca, PhD. Agency for Healthcare Research and Quality, 540 Gaither Road, Room 5002, Rockville, MD 20850. Email: zeynal.karaca@ahrq.hhs.gov.
Submission history: Revision received May 21, 2012; Submitted November 30, 2012; Accepted March 25, 2013
We presented the empirical results of the linear regression model here. The estimates obtained from the robust linear regression model were parallel to our estimates of the linear regression model.
REFERENCES
1 . National Healthcare Disparities Report. 2004;
2 . Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. 2003;
3 Brown ER, Ojeda VD, Wyn R . Racial and Ethnic Disparities in Access to Health Insurance and Health Care. 2000;
4 Collins K, Hughes D, Doty M Diverse Communities, Common Concerns: Assessing Health Care Quality for Minority Americans. Findings from the Commonwealth Fund 2001 Health Care Quality Survey. 2002;
5 Bazarian JJ, Pope C, McClung J Ethnic and racial disparities in emergency department care for mild traumatic brain injury. Acad Emerg Med. 2003; 10:1209-1217
6 Pletcher MJ, Kertesz SG, Kohn MA Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008; 299:70-78
7 Todd KH, Samaroo N, Hoffman JR Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993; 269:1537-1539
8 Heins JK, Heins A, Grammas M Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs. 2006; 32:219-224
9 Yen K, Kim M, Stremski ES Effect of ethnicity and race on the use of pain medications in children with long bone fractures in the emergency department. Ann Emerg Med. 2003; 42:41-47
10 Bradley EH, Herrin J, Wang Y Racial and ethnic differences in time to acute reperfusion therapy for patients hospitalized with myocardial infarction. JAMA. 2004; 292:1563-1572
11 Kressin NR, Petersen LA Racial variations in cardiac procedures: a review of the literature and prescription for future research. Ann Intern Med. 2001; 135:352-366
12 Lillie-Blanton M, Rushing O, Ruiz S . Racial/Ethnic Differences in Cardiac Care: The Weight of the Evidence. 2002;
13 Peterson ED, Shaw LK, DeLong ER Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter?. N Engl J Med. 1997; 336:480-486
14 Kaul P, Lytle B, Spertus M Influence of racial disparities in procedure use on functional status outcomes among patients with coronary artery disease. Circulation. 2005; 111:1284-1290
15 Kressin NR, Petersen LA Racial differences in the use of invasive cardiovascular procedures: review of the literature and prescription for future research. Ann Intern Med. 2001; 135:352-366
16 Chen J, Rathore SS, Radford MJ Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001; 344:1443-1449
17 Schneider EC, Leape LL, Weissman JS Racial differences in cardiac revascularization rates: does “overuse” explain higher rates among white patients?. Ann Intern Med. 2001; 135:328-337
18 Asplin BR Measuring crowding: time for a paradigm shift. Acad Emerg Med. 2006; 13:459-461
19 Herring A, Wilper A, Himmelstein DU Increasing length of stay among adult visits to U.S. emergency departments, 2001–2005. Acad Emerg Med. 2009; 16:609-616
20 Chalfin DB, Trzeciak S, Likourezos A Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007; 35:1477-1483
21 Andrulis DP, Kellermann A, Hintz EA Emergency departments and crowding in United States teaching hospitals. Ann Emerg Med. 1991; 20:980-986
22 Wilper AP, Woolhandler S, Lasser KE Waits to see an emergency department physician: U.S. trends and predictors, 1997– 2004. Health Aff (Millwood). 2008; 27:w84-w95
23 Pines JM, Localio AR, Hollander JE Racial Disparities in Emergency Department Length of Stay for Admitted Patients in the United States. Acad Emerg Med. 2009; 16:403-410
24 Karve SJ, Balkrishnan R, Mohammad YM Racial/ethnic disparities in emergency department waiting time for stroke patients in the United States. J Stroke Cerebrovasc Dis. 2011; 20:30-40
25 Wu BU, Banks PA, Conwell DL Disparities in emergency department wait times for acute gastrointestinal illnesses: results from the National Hospital Ambulatory Medical Care Survey, 1997–2006. Am J Gastroenterol. 2009; 104:1668-1673
26 Tamayo-Sarver JH, Hinze SW, Cydulka RK Racial and Ethnic Disparities in Emergency Department Analgesic Prescription. Am J Public Health. 2003; 93:2067-2073
27 Shafi S, Gentilello LM Ethnic disparities in initial management of trauma patients in a nationwide sample of emergency department visits. Arch Surg. 2008; 143:1057-1061
28 Tsai CL, Camargo CA Racial and ethnic differences in emergency care for acute exacerbation of chronic obstructive pulmonary disease. Acad Emerg Med. 2009; 16:108-115
29 Baker DW, Stevens CD, Brook RH Determinants of emergency department use: are race and ethnicity important?. Ann Emerg Med. 1996; 28:677-682
30 Hoot NR, Aronsky D Systematic review of emergency department crowding: Causes, effects, and solutions. Ann Emerg Med. 2008; 52:126-136
31 Shortridge EF, Moore JR Use of emergency departments for conditions related to poor oral healthcare: implications for rural and low-resource urban areas for three states. J Public Health Manag Pract. 2009; 15:238-245
32 Karaca Z, Wong HS, Mutter RL Duration of patients’ visits to the hospital emergency department. BMC Emergency Medicine. 2012; 12:15
33 Pines JM, Hollander JE Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008; 51:1-5
34 Rathlev NK, Chessare J, Olshaker J Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med. 2007; 49:265-271
35 Asaro PV, Lewis LM, Boxerman SB The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007; 14:235-242
36 Schull MJ, Kiss A, Szalai JP The effect of low-complexity patients on emergency department waiting times. Ann Emerg Med. 2007; 49:257-264
37 Lucas R, Farley H, Twanmoh J Emergency department patient flow: The influence of hospital census variables on emergency department length of stay. Acad Emerg Med. 2009; 16:597-602
38 Handel DA, Hilton JA, Ward MJ Emergency department throughput, crowding, and financial outcomes for hospitals. Acad Emerg Med. 2010; 17:840-847
39 Agrawal S Emergency department crowding: an ethical perspective. Acad Emerg Med. 2007; 14:750-751
40 Kelen GD, Scheulen JJ Commentary: emergency department crowding as an ethical issue. Acad Emerg Med. 2007; 14:751-754
41 Hoot NR, Aronsky D Systematic review of emergency department crowding: Causes, effects, and solutions. Ann Emerg Med. 2008; 52:126-136
42 Greene WH . Econometric analysis. 2000;
43 Baldauf M On the use of robust regression in econometrics. Economics Letters. 2012; 114:124-127
44 Zaman A, Rousseeuw PJ, Orhan R Econometric applications of high-breakdown robust regression techniques. Economics Letters. 2001; 71:1-8
45 Rousseeuw PJ, Wagner J Robust regression with a distributed intercept using least median of squares. Computational Statistics and Data Analysis. 1994; 17:65-76
46 Hubert M, Rousseeuw PJ Robust regression with both continuous and binary regressors. Journal of Statistical Planning and Inference. 1997; 57:153-163