| Author | Affiliation |
|---|---|
| Jeffrey Sankoff, MD | University of Colorado School of Medicine, Division of Emergency Medicine, Department of Surgery |
| Arnold Zidulka, MD | Royal Victoria Hospital, Department of Pulmonology |
ABSTRACT
Introduction:
This study describes a means of assessing the external jugular venous pressure (JVP) as an indicator of normal or elevated central venous pressure (CVP).
Methods:
Intensive care unit patients having CVP monitoring were examined. With patients in bed, the external jugular vein (EJV) was occluded at the base of the neck and observed to distend. The occlusion was then removed and the vein observed for collapse. Complete collapse was hypothesized to indicate a non-elevated CVP (≤8cm of water). In those patients whose EJV collapsed incompletely, the vein was then occluded with the finger near the angle of the jaw. With the occlusion maintained, the vein was milked downwards with the other hand to cause its emptying and was then observed for filling from below. Filling from below was hypothesized to indicate an elevated CVP (>8cm of water).
Results:
In 12 of the 40 patients examined, the EJV could not be assessed (EJV not seen at all: 5, and difficult to visualize: 7). For the remaining 28 patients 11 had a CVP > 8 cm, while 17 had a CVP patients, of ≤ 8. EJV assessment was 100% accurate (95% Confidence Interval 88–100) in predicting whether or not a patient’s CVP was greater or less than 8 cm of water.
Conclusion:
EJV assessment, when visible, is accurate to clinically assess a patient’s CVP in the hands of the author. Further studies are needed to see if they are reproducible by other observer.
INTRODUCTION
The rapid and accurate assessment of volume status is an important adjunct in the management of many emergency department (ED) patients. Although ultrasound has been shown to be helpful in this regard, it is not available to all emergency physicians (EP) and takes a degree of skill and time to perform properly.1, 2 The only other technological alternatives available to the EP to make such a determination are invasive.
In 1930 Lewis first described the assessment of central venous pressure, (CVP) by observing the level of distension of the internal jugular veins (IJV).3 Right atrial pressure is translated from the vertical height of the venous column above the sternal angle, (given that the sternal angle itself is, on average, 5 cm above the right atrium).4
Over the subsequent decades, physicians have employed this technique of clinical examination as a rapid, non-invasive means to assess the volume status of patients. Unfortunately, this method has been found to have a low sensitivity and poor inter-observer reliability and as such is ill-suited to ED patients.5–7
A simpler method would be to use the much more visible external jugular vein, (EJV) for measurement. However, such measurements had, until recently, been shown to be even more unreliable than those of the internal jugular.8 This is due to the variability of the anatomy of the vein and in some cases to partial occlusion of the vein by sclerotic valves that may prevent emptying.
In a study that compared EJV pulsation height to CVP readings from a central line,9Vinayak and colleagues9 helped to dispel the notion that the EJV is unreliable. They reported that EJV pulsations were useful to determine if an intensive care unit (ICU) patient’s CVP was low (≤ 5 cm of water), normal (6–9 cm) or high (≥ 10 cm) and that the EJV performed well for both low and high values. However, in a busy ED, this technique may perform less well than in an ICU, as it calls for a careful assessment of the veins to determine the height of venous pulsations. Alternatively, the EJV may be useful to rapidly establish whether a patient’s CVP is elevated or not, rather than an actual value in cm. While this would preclude a diagnosis of hypovolemia, it could simplify the determination of hypervolemia vs. euvolemia or hypovolemia. We describe a method that allows for the anatomical variations of the EJV. Although described in some texts, this method is rarely used and has never been validated prospectively.10
This report describes the technique and details the findings of a prospective trial to validate CVP measurement using the EJV.
METHODS
We conducted a prospective, observational study in a tertiary care hospital ICU in patients with invasive CVP monitoring. ICU, rather than ED, patients were enrolled because of the higher prevalence of CVP catheters and the decreased likelihood of ongoing resuscitation on study subjects. A convenience sample was selected over a three-month period from two hospitals. The local IRB did not require written consent.
Patients were examined by the author (JS, who was not involved in patient management and was blinded to the CVP measurement at the time of the exam) in the following manner: The primary nurse turned the monitor away prior to the investigator approaching the patient. Although CVP lines were not re-zeroed prior to the measurement being recorded, the wave-form was verified.
EJV assessment was done on whichever side of the neck that it could be most easily identified regardless of the presence of a central line. The EJV was identified as it courses medial to lateral in a rostral direction across the sternocleidomastoid muscle (Figure 1). With the patient’s bed at approximately 45°, the vein was occluded (above the clavicle) and observed to distend (Figure 2). At end expiration the occlusion was removed and the vein observed for collapse. Complete collapse was hypothesized to indicate a non-elevated CVP (≤8cm of water).

The surface anatomy of the external jugular vein, (indicated by the large arrows). The clavicle and sternocleidomastoid muscle are indicated by the small arrows.

The external jugular vein is occluded at the clavicle and distends as it fills from above (indicated by the arrows).
Incomplete emptying was recorded as indeterminate. This finding may be due to three reasons: 1) sclerotic valves prevent emptying in a patient with a normal CVP; 2) occlusion of the vein by a fascial flap at its distal end; or 3) truly elevated CVP. To differentiate between vein obstruction consistent with the first two possibilities and a truly elevated CVP, a second step was performed in patients whose EJV collapsed incompletely or had distension prior to examination.
The vein was occluded with the finger at the angle of the jaw. The vein was milked downwards with the other hand in order to cause its emptying (Figure 3). With the upper occlusion maintained, the lower occlusion was removed and the vein observed for filling from below (Figure 4). Filling from below was hypothesized to indicate an elevated CVP (>8cm of water). Lack of filling would indicate that the patient had a non-elevated CVP and that incomplete emptying observed in the first step of the procedure was due to venous obstruction.

The second step of the technique: milking the vein empty with a lower finger in the direction of the arrow while maintaining the upper occlusion with the other hand.

With the lower occlusion removed and the upper occlusion maintained, the external jugular vein fills from below, (as indicated by the arrows). The subject in the photo employed a Valsalva to stimulate a high CVP.
Patient data included age and sex. Prior to measurement, we noted whether or not the EJV was easily visualized, visualized with difficulty, or not visualized at all. This was a purposely subjective evaluation and not defined in advance. Outcome measures were the result of the examination technique, method of technique used (single or two-step reading), and the CVP reading from the central line.
Data were reported in two-by-two tables to demonstrate sensitivity, specificity and overall diagnostic accuracy.
RESULTS
We examined 40 patients. Twenty five (62.5%) were male. The average age was 40, (range 30–89). Ten patients (25%) had subclavian central lines, while 30 (75%) had IJV central catheters. In five of the 40 patients, the EJV could not be visualized at all. In the remaining 35 patients, 19 had a CVP ≤8 while 16 had a CVP > 8.
In the 35 patients whose EJV could be assessed, the sensitivity and specificity for elevated CVP was 91.7% (95% confidence interval (CI) 62–100) and 78.3% (95% CI 56–93) respectively. The overall accuracy of the test in determining whether or not CVP was < or ≥ 8 cm of water was 83 % (95% CI 66–93) (Table 1). Eliminating those seven patients in whom the EJV was not easily visible resulted in a diagnostic accuracy of 100% (95% CI 88–100)(Table 2).
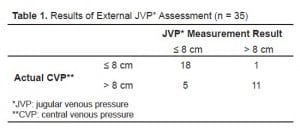
Results of External JVP* Assessment (n = 35)
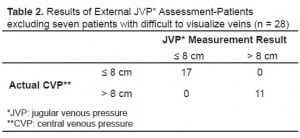
Results of External JVP* Assessment-Patients excluding seven patients with difficult to visualize veins (n = 28)
The reason for the inability to visualize the vein at all was obesity in three and anasarca in two. In an additional seven patients the EJV could be visualized only with difficulty, resulting in one false positive and five false negatives.
Table 3 shows the findings in all 35 patients by whether they had a one-step technique or two.
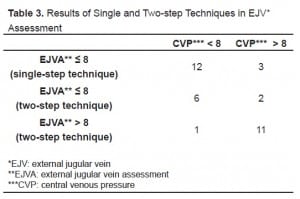
Results of Single and Two-step Techniques in EJV* Assessment
DISCUSSION
The rapid and accurate assessment of a patient’s volume status is important for treating a wide range of ED patients. The determination of hypovolemia is critical in early goal-directed therapy of sepsis and in diagnosing shock ascribed to volume loss.11 It is also helpful to be able to easily identify those patients who have adequate or elevated intravascular volume, as these patients are less likely to respond to further volume challenges in the case of shock, or may require diuresis for congestive heart failure.12
It has become common practice for EPs and intensivists to use CVP as a surrogate marker for intravascular volume. However, others have questioned the veracity of this and have advocated that other measures such as continuous right ventricular end-diastolic volume index, pulmonary capillary wedge pressure, or transesophageal echocardiographically-derived left ventricular end-diastolic area be used instead.13
While this important question has yet to be resolved, none of the alternatives to CVP are currently widely available to the EP. As such, the determination of CVP remains important.
While ultrasound provides a reliable and reproducible means of making this determination, it requires special equipment and skills. While physical examination of the IJV has been used for over 70 years, it is a skill performed inconsistently by cardiologists and non-cardiologists alike.14, 15 A recent report on the validity of EJV assessment made this a plausible alternative for this purpose, although it too may have limited value in the ED. The assessment of the EJV as described in this paper may make the determination of elevated volume status more practical.
In the hands of the author, EJV assessment via a single- or two-step technique when indicated, proved accurate in all patients in whom the EJV could easily be visualized. This limitation is important as false results were obtained in six of the seven patients in whom the vein was not easily seen. The subjective ability to visualize the EJV was not defined a-priori. We felt this was important as it would make this technique more applicable. We acknowledge that different observers may have varying abilities to visualize the EJV and this could result in inappropriate use of the technique. For our subjects, the EJV was easily identifiable in nearly 70% of the patients.
The accuracy of the test was consistent in both single-step and two-step techniques and was not affected by whether or not the patient’s true CVP was elevated. The test was performed on whichever side of the neck the EJV was visualized most easily, regardless of the presence of a central line. This was on the right in most patients but the left side proved no less accurate.
The time to conduct the test was very brief for all patients. For the single-step technique 10–15 seconds were required, while 20–25 seconds were required for the two-step test. Furthermore, in the setting of the ED the test can be performed without interrupting other patient evaluation and management. No patient reported any discomfort during the performance of the test.
In the current clinical environment, emphasizing all manner of technology to diagnose ED patients, there has been a gradual erosion in EPs’ physical exam skills. This study, although limited, offers a return to traditional physical examination that provides useful information quickly.
LIMITATIONS
These results reflect the experience of only one examiner and therefore lack external validity. However, in our experience, this test is easily taught. A study to determine inter-observer reliability as well as validating accuracy in the hands of others is planned.
Many of the patients were post-operative or on mechanical ventilation and these are not the same patients as in the ED.
Unlike the technique described by Vinayak, the one described here does not distinguish between euvolemia and hypovolemia. Instead, it discriminates between those who have hypervolemia and those without. Other means must be used to stratify patients in the latter category.
A final limitation of the EJV assessment is an extension of the limitations of assessment of the IJV. Neither of these methods will be useful to assess CVP in patients with tricuspid regurgitation or stenosis, atrial septal defect or superior vena cava syndrome,-all of which will result in falsely elevated readings.
CONCLUSION
EJV assessment in the hands of the author is highly accurate to grossly determine a patient’s CVP when the EJV is clearly visible. Both the single- and two-step techniques can be employed with confidence. The test can be performed during other important aspects of therapy. When the EJV is not clearly seen, other methods should be used to determine patient volume status.
Footnotes
We are indebted to Dr. Saundra M Kay who graciously offered her EJV for photography for the purpose of publication, and for reviewing this manuscript.
Supervising Section Editor: H. Bryant Nguyen, MD, MS
Submission history: Submitted October 15, 2008; Revision Received July 4, 2008; Accepted July 14, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Jeffrey Sankoff MD. Division of Emergency Medicine, Department of Surgery, University of Colorado School of Medicine, Leprino Office Building, 7th Floor, 12401 E. 17th Avenue, B-215, Aurora, CO 80045
Email: Jeffrey.sankoff@uchsc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Lipton B. Estimation of central venous pressure by ultrasound of the internal jugular vein. Am J Emerg Med. 2000;18:432–4. [PubMed]
2. Lipton BM. Determination of elevated jugular venous pressure by real-time ultrasound.Ann Emerg Med. 1999;34:115. [PubMed]
3. Lewis T. Early Signs of Cardiac Failure of the Congestive Type. The British Medical Journal. 1930;1:849–52.
4. O’Rourke R, Braunwald E. Harrison’s Principles of Internal Medicine. 13th ed. New York: McGraw-Hill; 1994.
5. Butman S, Ewy G, Standen J, et al. Bedside Cardiovascular Examination in Patients With Severe Chronic Heart Failure: Importance of Rest or Inducible Jugular Venous Distension. JACC. 1993;22:968–974. [PubMed]
6. Chakko S, Woska D, Martinez H, et al. Clinical, radiographic, and hemodynamic correlations in chronic congestive heart failure: conflicting results may lead to inappropriate care. Am J Med. 1991;90:353–359. [PubMed]
7. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989;261:884–8. [PubMed]
8. Davison R, Cannon R. Estimation of Central Venous Pressure by Examination of Jugular Veins. Amer Heart Jour. 1974;87:279–82. [PubMed]
9. Vinayak AG, Levitt J, Gehlbach B, Pohlman AS, Hall JB, Kress JP. Usefulness of the external jugular vein examination in detecting abnormal central venous pressure in critically ill patients. Archives of Internal Medicine. 2006;166:2132–2137. [PubMed]
10. Sapira J. The Art & Science of Bedside Diagnosis. Baltimore: Williams & Wilkins; 1990.
11. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M. Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. [PubMed]
12. Magder S, Bafaqeeh F. The clinical role of central venous pressure measurements.Journal of Intensive Care Medicine. 2007;22:44–51. [PubMed]
13. Wiesenack C, Fiegl C, Keyser A, Laule S, Prasser C, Keyl C. Continuously assessed right ventricular end-diastolic volume as a marker of cardiac preload and fluid responsiveness in mechanically ventilated cardiac surgical patients. Critical Care. 2005;9:R226–R233.(London, England) [PMC free article] [PubMed]
14. Ajuluchukwu JN, Inem VA. The examination of the jugular venous pressure (JVP): variation of technique amongst Nigerian resident doctors. Niger Postgrad Med J.2000;7:124–128. [PubMed]
15. Cook DJ. Clinical assessment of central venous pressure in the critically ill. Am J Med Sci. 1990;299:175–178. [PubMed]


