| Author | Affiliation |
|---|---|
| Nobuaki Inoue, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine, Division of Pediatric Emergency Medicine |
| Tommy Y. Kim, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine, Division of Pediatric Emergency Medicine |
| Anne Marie Birkbeck-Garcia, MD | Kaiser Permanente Southern California, Department of Pediatrics |
| Andrew Givner, MD | Desert Regional Medical Center, Department of Emergency Medicine |
| T. Kent Denmark, MD | Loma Linda University Medical Center and Children’s Hospital, Department of Emergency Medicine, Division of Pediatric Emergency Medicine |
ABSTRACT
Objectives
Premature infants are at higher risk of developing serious bacterial infections (SBI). However, the incidence of SBI in ex-premature infants presenting to the emergency department (ED) remains undetermined. The objective of this study is to examine the incidence of SBI in ex-premature infants with a postconceptional age of less than 48 weeks presenting to a pediatric ED.
Methods
A retrospective medical record review was conducted on 141 ex-premature infants with a postconceptional age of less than 48 weeks who had a full or partial septic work up completed in a pediatric ED between January 1, 1998 and March 31, 2005.
Results
The overall median gestational age at birth was 35 weeks (IQR 33–36 week) and the overall median postconceptional age at ED presentation was 40 weeks (IQR 37–42 weeks). Thirteen (9.2%) infants were found to have a SBI. Five subjects had pneumonia, four with bacteremia, two with pyelonephritis, and two with a concomitant infection of meningitis/pneumonia and bacteremia/pyelonephritis.
Conclusion
The results of this study reveal that the incidence of SBI in ex-premature infants with a postconceptional age of less than 48 weeks is similar to in-term infants (9.2%) and is consistent with previously published incidence rates in-term infants (10%).
INTRODUCTION
Premature infants are considered to be at higher risk of developing serious bacterial infections (SBIs). A younger gestational age at birth is associated with higher incidence of SBIs;1–4 however, there is no literature showing the incidence of SBIs in discharged premature infants presenting to the emergency department (ED) at a postconceptional age of less than 48 weeks. Practice among ED practitioners varies due to the lack of evidence regarding SBIs in ex-premature infants whose postconceptional age is still less than 48 weeks, especially if their chronological age is more than two months. The objective of this study is to examine the incidence of SBIs in ex-premature infants presenting to a pediatric ED up to a postconceptional age of 48 weeks.
METHODS
Data Collection
A retrospective medical record review was conducted on ex-premature infants who presented to a university-based children’s hospital pediatric ED between January 1, 1998 and March 31, 2005. A data collection sheet was completed by the primary study investigator (NI). Study subjects were identified from ED medical records with an ICD-9 code for prematurity. Data extracted from the records included the patient’s gestational age at birth, age during the ED visit, gender, race, reason for ED visit, confounding variables such as underlying medical conditions, results of urine, blood, cerebrospinal fluid (CSF) cultures, follow up for any return visit within one month for a SBI.
Patients
Inclusion criteria included premature infants delivered at less than a gestational age of 37 weeks, who returned to the pediatric ED with a postconceptional age less than 48 weeks at the time of presentation, and had a partial or full septic work up performed by the attending physician on duty. Full septic work up was defined as conducting all of these studies: blood, urine, and CSF cultures as well as chest radiograph; and partial septic work up was defined as conducting any of these studies. Exclusion criteria included those that were not born at our institution, missing/incomplete records, or those that did not have a full or partial septic work up completed in the ED.
A SBI was considered positive with any positive finding on urine, blood, CSF cultures or chest radiograph. Urine cultures were considered positive if a catheterized urine specimen grew greater than 10,000 colony forming units per milliliter of a single organism. Blood cultures were considered positive if a true pathogen was recovered or if skin flora was recovered through a central line. CSF cultures were considered positive if a true pathogen was recovered from the spinal fluid or if skin flora was isolated in the presence of a ventriculoperitoneal shunt. Chest radiograph readings were final interpretations read by a pediatric radiologist, and clinical correlation with the clinical history was used to determine the positive findings on the chest radiograph. Per ED policy during the study period, all patients discharged from the ED with cultures drawn are followed up by a clerical nurse and are often asked to return to the ED for positive culture results. Medical records were reviewed for return visits to the ED or hospitalization within one month of the initial ED visit to ensure that no patient was readmitted for a SBI after the initial ED visit.
Statistical Analysis
Data were analyzed to generate descriptive statistics using Statistical Package for the Social Sciences version 10. (SPSS Inc., Chicago, Illinois) Given that our data are not normally distributed, we present our results as medians with interquartile (IQR) ranges. Chi-square and Mann-Whitney test were used to evaluate the differences between groups. This study was approved by the local institutional review board.
RESULTS
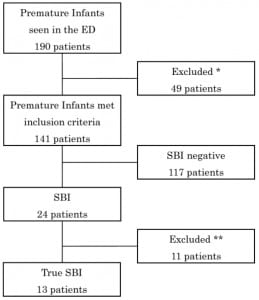
There were 190 medical records identified as premature infants seen in the ED during the study period requiring a work up for a possible SBI. Forty nine subjects were excluded due to non-infectious ED visits (17), greater than 48 weeks postconceptional age at time of ED visit (31), and incomplete medical record (1). The remaining 141 subjects (64 females) were included into the analysis. (Figure 1)
The overall median gestational age at birth was 35 weeks (IQR 33–36 week) with no significant difference between the SBI and non-SBI group (p=0.60). The overall median postconceptional age at ED presentation was 40 weeks (IQR 37–42 weeks) with no significant difference between the SBI and non-SBI group (p=0.57). Gender and race were not found to be significant predictors of a SBI (p = 0.17 and p = 0.58, respectively). The common presenting symptoms that prompted a work up included apnea (29), fever (26), respiratory distress (24), irritability (6), and lethargy (4). Forty infants (28.4%) had a full septic work up completed in the ED.
Twenty-four subjects were found to have positive culture results or radiographic findings suggestive of a SBI. Eleven subjects were excluded due to urine with mixed flora (3), urine with <10,000 colony forming units per milliliter of a single organism (2), blood with contaminant (5), CSF with contaminant (1) (Figure 1). The remaining 13 (9.2%) infants were found to have a SBI and admitted. Five subjects were diagnosed as pneumonia (38.4%), four had bacteremia (30.8%), two had pyelonephritis (15.4%), and one each for meningitis/pneumonia and bacteremia/pyelonephritis (7.7%) (Table 1).

The only confounding factor found to be clinically significant was a patient with a vertriculoperitoneal shunt who had a positive CSF culture and a positive chest radiograph four weeks after shunt placement (subject 11). Of the infants discharged home from the ED after septic work up, no patient was found to have a SBI within one month of discharge.
DISCUSSION
Prematurity is a common risk factor for SBIs in infants.1–4 The premature infant has a less developed immune system than the in-term infant as more maternal immunoglobulin G (IgG) is transferred to the fetus through the placenta later in the pregnancy.5 Serum level of IgG is lower among preterm infants,6 and a lower level of serum IgG is also a risk factor for SBIs among the premature infants.7 There is also a higher incidence of neutropenia observed in premature infants8, 9 and this is associated with higher mortality due to infection in these infants.9
Approximately 12 to 28% (n = 250 – 372) of neonates who present to the pediatric ED with fever have SBIs,10–12 and up to 10% (n = 1298) of febrile young infants up to three months of age with low risk criteria have SBIs.13, 14 There is no report identified to dateshowing the incidence of SBIs among ex-premature infants who present to the ED. The incidence of SBI found in this study was similar to the previous studies.
No statistical difference was found between the groups with SBIs and without SBIs in the median gestational birth age and the median postconceptional age at ED presentation. Confounding factors, such as indwelling devices, immunocompromised conditions, or any other underlying medical conditions were also assessed and revealed that none of subjects developed SBIs except one patient with a vertriculoperitoneal shunt. Further investigation is necessary to conclude their association with developing a SBI.
There are several limitations to this study. Above all, this is a retrospective study. Study subjects may have been missed due to miscoding. Conducting a full septic work up was determined by the attending physician on-duty. Although no infant returned to the ED or inpatient unit for a SBI within one month of discharge from the ED, they may have presented to another facility. However, all these concerns of “missing cases” would increase our incidence. Secondly, this study only evaluated 141 subjects, a relatively small sample size. We did not conduct a sample-size calculation because of the retrospective nature of this descriptive study.
Current guidelines suggest that febrile infants less than one month of age have a high risk of SBI and recommend conducting a full septic work up and hospitalization.15, 16 Well-appearing febrile infants with low risk criteria between 28 to 90 days old can be treated outpatient with full or partial work up. However, being “full-term” is one criterion for “low risk.” Therefore, all febrile ex-premature infants in this age range should have a full septic work up completed along with hospitalization based on these guidelines.15 Clinical dilemma exists when considering chronological age vs postconceptional age. Based on our results, the postconceptional age for most of the subjects with SBI was less than 44 weeks, except one (subject 13). Further investigations are required to resolve this dilemma. Our results show that the incidence of SBI in ex-premature infants <48 weeks post-conceptual age is similar to that of in-term infants as reported in prior studies.
Footnotes
Supervising Section Editor: Judith R. Klein, MD
Submission history: Submitted July 29, 2008; Revision Received October 15, 2008; Accepted October 21, 2008.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Nobuaki Inoue, MD. 11234, Anderson Street, Suite A 108, Loma Linda, California 92354
Email: ninoue@llu.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Tessin I, Trollfors B, Thiringer K. Incidence and etiology of neonatal septicemia and meningitis in Western Sweden 1975–1986. Acta Paediatr Scand. 1990;79:1023–1030.[PubMed]
2. Stoll BJ, Gordon T, Korones SB, et al. Late-onset sepsis in very low birth weight neonates: a report from the National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1996;129:63–71. [PubMed]
3. Stoll BJ, Gordon T, Korones SB, et al. Early-onset sepsis in very low birth weight neonates: a report from the National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr. 1996;129:72–80. [PubMed]
4. Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics.2002;110(Pt 1):285–291. [PubMed]
5. Hobbs JR, Davis JA. Serum gammaG-globulin levels and gestational age in premature babies. Lancet. 1967;1:757–759. [PubMed]
6. Ballow M, Cates KL, Rowe JC, Goetz C, Desbonnet C. Development of the immune system in very low birth weight (less than 1500 g) premature infants: concentrations of plasma immunoglobulins and patterns of infections. Pediatr Res. 1986;20:899–904. [PubMed]
7. Sandberg K, Fasth A, Berger A, et al. Preterm infants with low immunoglobulin G levels have increased risk of neonatal sepsis but do not benefit from prophylactic immunoglobulin G. J Pediatr. 2000;137:623–628. [PubMed]
8. Gessler P, Luders R, Konig S, Haas N, Lasch P, Kachel W. Neonatal neutropenia in low birth weight premature infants. Am J Perinatol. 1995;12:34–38. [PubMed]
9. Funke A, Berner R, Traichel B, Schemeisser D, Leititis JU, Niemeyer CM. Frequency, natural course, and outcome of neonatal neutropenia. Pediatrics. 2000;106:45–51.[PubMed]
10. Chiu CH, Lin TY, Bullard MJ. Identification of febrile neonates unlikely to have bacterial infections. Pediatr Infect Dis J. 1997;16:59–63. [PubMed]
11. Baker MD, Bell LM. Unpredictability of serious bacterial illness in febrile infants from birth to 1 month of age. Arch Pediatr Adolesc Med. 1999;153:508–511. [PubMed]
12. Kadish HA, Loveridge B, Tobey J, et al. Applying outpatient protocols in febrile infants 1–28 days of age: can the threshold be lowered? . Clin Pediatr. 2000;39:81–88.
13. Baker MD, Bell LM, Avner JR. The efficacy of routine outpatient management without antibiotics of fever in selected infants. Pediatrics. 1999;103:627–631. [PubMed]
14. Byington CL, Rittichier KK, Bassett KE, et al. Serious bacterial infections in febrile infants younger than 90 days of age: the importance of ampicillin-resistant pathogens.Pediatrics. 2003;111(5 Pt 1):964–968. [PubMed]
15. Baraff LJ. Management of fever without source in infants and children. Ann Emerg Med. 2000;36:602–614. [PubMed]
16. American College of Emergency Physicians Clinical Policies Subcommittee on Pediatric Fever. Clinical policy for children younger than three years presenting to the emergency department with fever. Ann Emerg Med. 2003;42:530–545. [PubMed]


