| Author | Affiliation |
|---|---|
| Eric Bansal, MD | Division of Cardiovascular Medicine, University of Southern California, Los Angeles, California |
| Rahul Dhawan, DO | Division of Cardiovascular Medicine, University of Southern California, Los Angeles, California |
| Brittany Wagman, BS | Office of Biostatistics and Outcomes Assessment, Los Angeles County + University of Southern California Medical Center, Los Angeles, California |
| Garren Low, MS | Office of Biostatistics and Outcomes Assessment, Los Angeles County + University of Southern California Medical Center, Los Angeles, California |
| Ling Zheng, MD, PhD | Department of Neurology, University of Southern California, Los Angeles, California |
| Linda Chan, PhD | Office of Biostatistics and Outcomes Assessment, Los Angeles County + University of Southern California Medical Center, Los Angeles, California |
| Kim Newton, MD | Department of Emergency Medicine, University of Southern California, Los Angeles, California |
| Stuart P. Swadron, MD | Department of Emergency Medicine, University of Southern California, Los Angeles, California |
| Nicholas Testa, MD | Department of Emergency Medicine, University of Southern California, Los Angeles, California |
| David M. Shavelle, MD | Division of Cardiovascular Medicine, University of Southern California, Los Angeles, California |
Introduction
Methods
Results
Limitations
Discussion
Conclusion
ABSTRACT
Introduction
Patients with ST elevation myocardial infarction (STEMI) require rapid identification and triage to initiate reperfusion therapy. Walk-in STEMI patients have longer treatment times compared to emergency medical service (EMS) transported patients. While effective triage of large numbers of critically ill patients in the emergency department is often cited as the reason for treatment delays, additional factors have not been explored. The purpose of this study was to evaluate baseline demographic and clinical differences between walk-in and EMS-transported STEMI patients and identify factors associated with prolonged door to balloon (D2B) time in walk-in STEMI patients.
Methods
We performed a retrospective review of 136 STEMI patients presenting to an urban academic teaching center from January 2009 through December 2010. Baseline demographics, mode of hospital entry (walk-in versus EMS transport), treatment times, angiographic findings, procedures performed and in-hospital clinical events were collected. We compared walk-in and EMS-transported STEMI patients and identified independent factors of prolonged D2B time for walk-in patients using stepwise logistic regression analysis.
Results
Walk-in patients (n=51) were more likely to be Latino and presented with a higher heart rate, higher systolic blood pressure, prior history of diabetes mellitus and were more likely to have an elevated initial troponin value, compared to EMS-transported patients. EMS-transported patients (n=64) were more likely to be white and had a higher prevalence of left main coronary artery disease, compared to walk-in patients. Door to electrocardiogram (ECG), ECG to catheterization laboratory (CL) activation and D2B times were significantly longer for walk-in patients. Walk-in patients were more likely to have D2B time >90 minutes, compared to EMS- transported patients; odds ratio 3.53 (95% CI 1.03, 12.07), p=0.04. Stepwise logistic regression identified hospital entry mode as the only independent predictor for prolonged D2B time.
Conclusion
Baseline differences exist between walk-in and EMS-transported STEMI patients undergoing primary percutaneous coronary intervention (PCI). Hospital entry mode was the most important predictor for prolonged treatment times for primary PCI, independent of age, Latino ethnicity, heart rate, systolic blood pressure and initial troponin value. Prolonged door to ECG and ECG to CL activation times are modifiable factors associated with prolonged treatment times in walk-in STEMI patients. In addition to promoting the use of EMS transport, efforts are needed to rapidly identify and expedite the triage of walk-in STEMI patients.
INTRODUCTION
Patients with ST elevation myocardial infarction (STEMI) require rapid identification and triage to initiate reperfusion therapy. In the United States, primary percutaneous coronary intervention (PCI) is favored over thrombolytic therapy as the mode of reperfusion.1 However, delay to performing PCI is associated with worse clinical outcome.2 Various factors are associated with prolonged treatment times, and nationwide efforts are underway to address these issues.3–6
In 2008, the Los Angeles County Emergency Medical System (EMS) established a regionalized care system for patients with STEMI. Patients with a pre-hospital electrocardiogram (ECG) showing STEMI are transported to designated STEMI receiving centers for primary PCI.3 Patients with STEMI may also present directly to the emergency department (ED) via self or family transport and are referred to as “walk–in” patients. Prior studies suggest that walk-in STEMI patients have longer treatment times compared to EMS-transported patients.7–9 While effective triage of large numbers of critically ill patients in emergency departments is often cited as the reason for treatment delays, additional factors have not been adequately evaluated.
The goal of this study was to evaluate baseline demographic and clinical differences between walk-in and EMS-transported STEMI patients and identify factors associated with prolonged door to balloon (D2B) time in walk-in STEMI patients.
METHODS
Study Population
Patients were included in this study if they had chest pain (or an angina equivalent), an ECG showing 1 mm of ST segment elevation in 2 contiguous leads consistent with STEMI and were referred for emergency coronary angiography and primary PCI. This study was performed at an urban academic medical center from January, 2009 through December, 2010. Patients were identified for this retrospective, observational study using the Los Angeles County + USC Medical Center Cardiac Catheterization Laboratory STEMI database. Data abstraction was performed by one physician (EB) and all data was reviewed as part of our ongoing institutional quality assessment and quality improvement STEMI program. For EMS-transported patients, the diagnosis of STEMI was made by paramedics when a pre-hospital ECG showed STEMI. For walk-in patients, the diagnosis of STEMI was made by the emergency physician (EP) when the initial or subsequent ECG showed STEMI. The cardiac catheterization laboratory was activated for presumed STEMI patients by EPs using a bundle-paging system. If the pre-hospital ECG or initial ECG was later interpreted by the interventional cardiologist as not showing STEMI and if the patient did not undergo emergent coronary angiography, they were excluded from the study. Patients were also excluded if they did not undergo primary PCI, died in the ED prior to receiving coronary angiography, were transferred-in from another institution for primary PCI or if they were transferred out to another institution during their index hospitalization.
Primary Percutaneous Coronary Intervention
Procedures were performed by 4 experienced interventional cardiologists. Use of mechanical or rheolytic thrombectomy devices prior to stent placement, the decision to place a bare metal or drug eluting stent, the choice of the anticoagulation used for the procedure and the use of vascular closure devices were left to the discretion of the treating interventional cardiologist. Following the procedure, all patients received aspirin (325 mg once daily) and either clopidogrel (300 mg or 600 mg orally followed by 75 mg once daily) or prasugrel (60 mg orally followed by 10 mg once daily). Clopidogrel or prasugel was continued for at least 1 month following placement of a bare metal stent and for 12 months following placement of a drug-eluting stent. Life-long aspirin therapy was recommended. Ejection fraction was assessed prior to hospital discharge by transthoracic echocardiography.
Study Parameters and Outcome Measures
We defined EMS-transport as patients being transported by EMS services. Walk-in patients were defined as those arriving to the hospital by self or private transportation, taxis, public transportation or walking to the hospital. The demographic and clinical parameters of the study population included age, gender, ethnicity, initial complaint and medical history. We defined hypertension as systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg or receiving anti-hypertensive medications. Hyperlipidemia was defined as a total cholesterol level >220 mg/dl or receiving medications for hyperlipidemia. Diabetes mellitus was defined as a hemoglobin A1c level >6.5% or treatment with insulin or an oral hypoglycemic medication. We defined chronic lung disease as the use of medications for chronic obstructive pulmonary disease. Peripheral vascular disease was defined as a claudication, prior history of peripheral angioplasty, stent placement or atherectomy, prior history of lower extremity bypass surgery or prior history of carotid endarterectomy.
Presentation variables included congestive heart failure or cardiogenic shock at the time of hospital admission, admission heart rate and systolic blood pressure and the initial troponin value. We defined congestive heart failure as physical findings consistent with congestive heart failure and radiographic evidence of pulmonary edema. Cardiogenic shock was defined as a systolic blood pressure of less than 90 mmHg for at least 30 minutes following adequate fluid resuscitation of at least 1 liter of normal saline or the need for inotropic agents to maintain a systolic blood pressure of at least 90 mmHg. Clinical signs of hypoperfusion, including decreased urine output, altered mental status and peripheral vasoconstriction were also required to establish the diagnosis of cardiogenic shock. For patients with a swan ganz catheter in place, we defined cardiogenic shock as a pulmonary capillary wedge pressure >18 mmHg and a cardiac index <2.0 liters/minute. Angiographic variables included the number of coronary vessels diseased with luminal diameter stenosis >70% by visual assessment. Left main coronary artery disease was defined as ≥50% luminal diameter stenosis by visual assessment. Procedures performed during the index hospitalization included coronary artery bypass grafting surgery (following 24 hours from coronary angiography) and placement of an intra aortic balloon pump. Ejection fraction was measured by transthoracic echocardiography prior to hospital discharge.
We studied the following time intervals: door to ECG time, ECG to cardiac catheterization (CL) activation time, CL activation to balloon time and D2B time. The primary endpoint of this study was D2B time. In-hospital clinical events included cardiogenic shock, cerebrovascular accident, congestive heart failure, reinfarction, respiratory failure, blood transfusion and in-hospital mortality. We defined reinfarction as subsequent elevation in cardiac biomarkers associated with angina requiring repeat emergent coronary angiography following the initial PCI procedure.
Statistical Analysis
We compared baseline demographic and clinical characteristics, treatment time intervals, in-hospital clinical events and in-hospital mortality between the EMS-transported and walk-in groups. We used chi-square test for comparing proportions, and the Student t-test or the Wilcoxon ranked sum test, wherever appropriate, was used for comparing means. We used non-parametric analysis of covariance to compare the D2B time between the two groups adjusting for significant baseline characteristics found between the two groups. Mean ± standard deviation are reported for continuous variables and number (percentage) are reported for categorical variables. We included significant risk factors identified in the univariate analysis in the stepwise logistic regression analysis from which significant independent factors were derived. Statistical significance was defined as a p-value <0.05. We used the Statistical Analysis System (SAS version 9.1) for all analysis.
RESULTS
Study Population
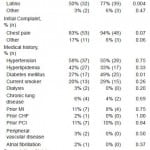
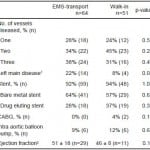
Between January 2009 and December 2010, 136 patients undergoing emergent coronary angiography for STEMI were evaluated. We excluded 21 patients because PCI was not performed (left main and/or multivessel disease requiring surgery n=5, cardiomyopathy n=12, no culprit lesion identified n=4), yielding a study population of 115 patients. Fifty-one patients (44%) arrived as walk-in (Walk-in group) and 64 (56%) were transported by EMS (EMS-transport group). EMS-transported patients were older and more likely to be white compared to walk-in patients (Table 1). Walk-in patients were more likely to be Latino, had a higher prevalence of diabetes mellitus and presented with a higher heart rate and higher systolic blood pressure than EMS-transported patients. A higher proportion of the walk-in patients presented with an elevated troponin value, compared to EMS-transport patients, 88% versus 64%, p=0.005, respectively. The number of diseased coronary vessels was similar between EMS-transport and walk-in patients (Table 2). A higher proportion of EMS-transport patients had significant left main disease compared to walk-in patients, 22% versus 8%, p=0.04, respectively. The use of bare metal stents and drug eluting stents, the need for coronary artery bypass surgery, use of intra aortic balloon pump and ejection fraction prior to hospital discharge were similar between the groups.
Table 1. Baseline demographics and presenting characteristics of emergency medical services (EMS)-transport and walk-in STEMI patients undergoing primary percutaneous coronary intervention.
1Mean ± standard deviation; BMI, body mass index; MI, myocardial infarction; CHF, congestive heart failure; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery; BPM, beats per minute
Table 2. Angiographic findings and procedures performed of emergency medical service (EMS)-transported and walk-in STEMI patients undergoing primary percutaneous coronary
intervention.
1Left main disease defined as >50% diameter stenosis; CABG, coronary artery bypass graft surgery. 2Mean + standard deviation.
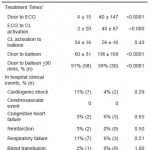
Treatment Times and In-hospital Clinical Events
Door to ECG and ECG to CL activation times were significantly longer in the walk-in compared to EMS-transported patients (Table 3). CL activation to balloon time was similar between both groups. D2B time was significantly longer in the walk-in versus EMS-transported patients, 136±169 versus 60±31 minutes, p<0.0001, respectively. The proportion of patients with D2B time ≤ 90 minutes was significantly higher in the EMS-transport versus the walk-in patients, 91% versus 59%, p<0.0001, respectively. In-hospital clinical events, including cardiogenic shock, cerebrovascular events, congestive heart failure, reinfarction, respiratory failure, blood transfusion and mortality, were similar between both groups.
Table 3. Treatment times and in-hospital clinical events of emergency medical service (EMS)-transported and walk-in STEMI patients undergoing primary percutaneous coronary intervention.
1Mean + standard deviation; ECG, electrocardiogram; CL, catheterization laboratory.
Comparison of D2B time between Walk-in and EMS patients
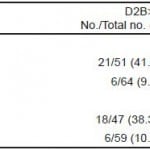
Univariate analysis comparing walk-in and EMS-transport patients identified the following significant risk factors: mode of entry, age, Latino ethnicity, left main disease, initial troponin elevation, admission heart rate, admission systolic blood pressure, and diabetes mellitus. These variables were included in the logistic regression model to derive an adjusted odds ratio for D2B time >90 minutes. Table 4 provides the unadjusted and adjusted odds ratio for D2B time >90 minutes for walk-in as compared to EMS-transport patients.
Table 4. Odds ratios (OR) from logistic regression model for D2B time >90 minutes.
*Adjusted for (variables with p<0.05) age, Latino ethnicity, left main disease, initial troponin elevation, admission heart rate, admission systolic blood pressure, and diabetes mellitus.
**Sample size decreased due to missing values in the covariates.
Identification of independent risk factors for D2B time >90 minutes
Univariate analyses comparing patients with D2B time ≤90 minutes and D2B time >90 minutes identified hospital entry mode, Latino ethnicity and history of diabetes mellitus as significant risk factors. Stepwise regression analysis identified hospital entry mode (walk-in versus EMS-transport) as the only independent factor associated with D2B time >90 minutes (data not shown).
LIMITATIONS
This study has several limitations. The number of patients included is small given that the study period was only 23 months. We excluded 21 patients from the analysis because they did not undergo PCI. Although the primary endpoint of this study was D2B time and therefore required inclusion of patients undergoing PCI, exclusion of 21 patients represents a loss of data and a decrease in the overall sample size. Patients were evaluated by numerous different physicians, nurses and staff in the ED during the study period. While there is a standard triage for patients presenting with non-traumatic chest pain, variations in the triage process may have altered time to ECG acquisition, time for ECG interpretation and time to CL activation. Inherent in the retrospective nature of the study are issues related to the inability to collect information not available in the medical records. The use of a single data abstracter reduces heterogeneity but may also have introduced some bias into data collection. The current study was performed at a large, urban academic teaching hospital with activation of the CL done by EPs using a single bundle-paging system, and as such our results may not be applicable to other hospital systems.
DISCUSSION
In the present study of STEMI patients undergoing primary PCI, 64% arrived via EMS-transport and 44% by walk-in transport. As observed in prior studies, walk-in patients had a significantly longer D2B time compared to EMS-transported patients, 136 ± 169 versus 60 ± 31 minutes, p<0.0001, respectively. Although there were significant baseline differences between walk-in and EMS-transported patients undergoing primary PCI, we found that hospital entry mode was the most important predictor for prolonged D2B time. In evaluating the treatment processes for walk-in STEMI patients, we found that prolonged door to ECG and ECG to CL activation times contributed to the prolonged D2B time.
The evaluation of walk-in patients with chest pain in the ED is multifaceted and requires a complex number of decisions at multiple levels throughout the triage process.10–12 Patients arriving via walk-in transport to ED fail to receive a number of components that EMS-transported patients routinely receive. The most essential of these is a pre-hospital ECG that allows rapid identification of a STEMI, thus mandating rapid triage on arrival. Use of a pre-hospital ECG reduces door to needle time in those receiving thrombolytic therapy and reduces D2B time in those undergoing primary PCI.13,14 Current American College of Cardiology/American Heart Association Guidelines indicate that an ECG should be obtained within 10 minutes of hospital arrival for patients with chest pain or an anginal equivalent or other symptoms suggestive of STEMI.15 The ability to identify walk-in patients with chest pain who require an ECG at the time of initial triage is critical. Several recent studies have explored various methods in an attempt to reduce this arrival or door to ECG time.16–19 Takakuwa et al16 found that use of registration clerks to screen patients for chest pain followed by expedited orders for an ECG improved the percentage of patients receiving an ECG within 10 minutes of arrival from 16% to 64%. Zarich et al17 performed routine ECGs on all males >35 years of age or women >40 years of age with nontraumatic chest pain and reduced the door to ECG time from 15 to 7.6 minutes, p<0.001. Caputo et al18 reduced door to ECG time from 8.4 to 3.7 minutes by obtaining a “more rapid ECG assessment of patients presenting with a complaint consistent with angina;” additional details on how these patients were identified at the time of triage were not described. Purim-Shem-Tov et al19 used a dedicated ED greeter stationed in the triage area who screened all patients for chest pain, shortness of breath, acute mental status change in nursing home patients and dizziness and nausea in diabetic patients. Use of this protocol reduced the door to ECG time to 8.8 minutes. In addition to obtaining an ECG within 10 minutes of hospital arrival, rapid and accurate interpretation of the ECG and prompt activation of the STEMI team by EPs using a bundle paging system are additional essential components.20,21
Given the documented benefits of EMS-transport for STEMI patients, few studies have specifically evaluated walk-in STEMI patients undergoing primary PCI.7–9 Canto et al8 evaluated over 300,000 patients enrolled in the National Registry of Myocardial Infarction (NRMI) database and compared baseline characteristics and management between EMS and self-transport (walk-in) patients. While use of EMS was associated with shorter treatment times, only 10% of the study cohort underwent primary PCI, and factors associated with prolonged treatment times in the walk-in cohort were not explored. So et al7 evaluated STEMI patients arriving via EMS versus self-transport to 2 hospitals in Canada. Three hundred twenty- three of the 356 patients (91%) received thrombolytic therapy and 33 of the 356 patients (9%) received primary PCI; the reasons for prolonged treatment times in the self-transport (walk-in) primary PCI cohort were not explored. Despite nationwide efforts to promote the use of EMS-transport, walk-in patients constitute approximately 40% of STEMI patients.7,9 A recent study from the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network Registry – Get With the Guidelines (ACTION Registry-GWTG) found that older patients, those living farther from the hospital and those with hemodynamic compromise were more likely to use EMS-transport.9
CONCLUSION
In addition to promoting the use of EMS-transport for STEMI patients, efforts are needed to rapidly identify and expedite the triage of walk-in STEMI patients. Prolonged door to ECG and ECG to CL activation times contribute to treatment delays in walk-in STEMI patients and should continue to be a focus of the quality improvement process.
Footnotes
Address for Correspondence: David M. Shavelle, MD. Division of Cardiovascular Medicine, University of Southern California, 1510 San Pablo Street, Suite 300, Los Angeles, CA 90033. Email: shavelle@usc.edu 2 / 2014; 15:81 – 87
Submission history: Revision received April 1, 2013; Submitted July 9, 2013; Accepted September 4, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20. [PubMed]
2. Terkelsen CJ, Sorensen JT, Maeng M, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7):763–771. [PubMed]
3. Rokos IC, Larson DM, Henry TD, et al. Rationale for establishing regional ST-elevation myocardial infarction receiving center (SRC) networks. Am Heart J. 2006;152(4):661–667. [PubMed]
4. Mehta RH, Bufalino VJ, Pan W, et al. Achieving rapid reperfusion with primary percutaneous coronary intervention remains a challenge: insights from American Heart Association’s Get With the Guidelines program. Am Heart J. 2008;155(6):1059–1067. [PubMed]
5. Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes.2009;2(5):491–499. [PubMed]
6. Krumholz HM, Bradley EH, Nallamothu BK, et al. A campaign to improve the timeliness of primary percutaneous coronary intervention: Door-to-Balloon: An Alliance for Quality. JACC Cardiovasc Interv. 2008;1(1):97–104. [PubMed]
7. So DY, Ha AC, Turek MA, et al. Comparison of mortality patterns in patients with ST-elevation myocardial infarction arriving by emergency medical services versus self-transport (from the prospective Ottawa Hospital STEMI Registry). Am J Cardiol. 2006;97(4):458–461. [PubMed]
8. Canto JG, Zalenski RJ, Ornato JP, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106(24):3018–3023. [PubMed]
9. Mathews R, Peterson ED, Li S, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124(2):154–163. [PubMed]
10. Jesse RL, Kontos MC. Evaluation of chest pain in the emergency department. Curr Probl Cardiol. 1997;22(4):149–236. [PubMed]
11. Mair J, Smidt J, Lechleitner P, et al. Rapid accurate diagnosis of acute myocardial infarction in patients with non-traumatic chest pain within 1 h of admission. Coron Artery Dis. 1995;6(7):539–545.[PubMed]
12. Ting HH, Lee TH, Soukup JR, et al. Impact of physician experience on triage of emergency room patients with acute chest pain at three teaching hospitals. Am J Med. 1991;91(4):401–408. [PubMed]
13. Hutchison AW, Malaiapan Y, Jarvie I, et al. Prehospital 12-lead ECG to triage ST-elevation myocardial infarction and emergency department activation of the infarct team significantly improves door-to-balloon times: ambulance Victoria and MonashHEART Acute Myocardial Infarction (MonAMI) 12-lead ECG project. Circ Cardiovasc Interv. 2009;2(6):528–534. [PubMed]
14. Morrison LJ, Brooks S, Sawadsky B, et al. Prehospital 12-lead electrocardiography impact on acute myocardial infarction treatment times and mortality: a systematic review. Acad Emerg Med. 2006;13(1):84–89. [PubMed]
15. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51(2):210–247. [PubMed]
16. Takakuwa KM, Burek GA, Estepa AT, et al. A method for improving arrival-to-electrocardiogram time in emergency department chest pain patients and the effect on door-to-balloon time for ST-segment elevation myocardial infarction. Acad Emerg Med. 2009;16(10):921–927. [PubMed]
17. Zarich SW, Sachdeva R, Fishman R, et al. Effectiveness of a multidisciplinary quality improvement initiative in reducing door-to-balloon times in primary angioplasty. J Interv Cardiol. 2004;17(4):191–195. [PubMed]
18. Caputo RP, Kosinski R, Walford G, et al. Effect of continuous quality improvement analysis on the delivery of primary percutaneous revascularization for acute myocardial infarction: a community hospital experience. Catheter Cardiovasc Interv. 2005;64(4):428–433. [PubMed]
19. Purim-Shem-Tov YA, Rumoro DP, Veloso J, et al. Emergency Department greeters reduce door-to-ECG time. Crit Pathw Cardiol. 2007;6(4):165–168. [PubMed]
20. Kim SH, Oh SH, Choi SP, et al. The appropriateness of single page of activation of the cardiac catheterization laboratory by emergency physician for patients with suspected ST-segment elevation myocardial infarction: a cohort study. Scand J Trauma Resusc Emerg Med. 2011;19:50.[PMC free article] [PubMed]
21. Kraft PL, Newman S, Hanson D, et al. Emergency physician discretion to activate the cardiac catheterization team decreases door-to-balloon time for acute ST-elevation myocardial infarction. Ann Emerg Med. 2007;50(5):520–526. [PubMed]