| Author | Affiliation |
|---|---|
| T. Paul Tran, MD | University of Nebraska Medical Center |
| Laura M. Robinson, MPA | University of Nebraska Medical Center |
| John R. Keebler, MD | University of Nebraska Medical Center |
| Richard A. Walker, MD | University of Nebraska Medical Center |
| Michael C. Wadman, MD | University of Nebraska Medical Center |
ABSTRACT
Introduction:
Health literacy is an important predictor of healthcare outcomes, but research on this topic has largely been absent from the emergency medicine literature. We measured the prevalence of health literacy in parents or guardians of pediatric patients seen in the emergency department (ED).
Methods:
This was an observational study conducted in a Midwestern urban, university-based, tertiary, Level 1 trauma center ED with 33,000 visits/year. Using convenience sampling during a three-month period, English-speaking parents or guardians of pediatric patients (< 19 yrs.) were asked to complete the short version of the Test of Functional Health Literacy for Adults (s-TOFHLA). Parents/guardians were excluded if they had uncorrected visual impairment, required an interpreter, had altered mental status, or if the patients they accompanied were the subjects of a medical or trauma activation.
Results:
Of the 188 parents or guardians approached, six did not consent or withdrew, one was excluded, leaving 181 (96.3%) in the study. Of these, 19 (10.5%) had either “marginal” or “inadequate” health literacy, while 162 (89.5%, 95% CI: 84.1%, 93.6%) had “adequate” health literacy.
Conclusion:
A large majority (89.5%) of English-speaking parents or guardians of pediatric patients evaluated in the ED have adequate health literacy. This data may prompt ED professionals to adjust their communication styles in the evaluation of children. Future multi-center studies are needed to confirm the findings in this pilot study.
INTRODUCTION
Health literacy is defined as the ability of patients to perform the basic reading and computational tasks required to function effectively in the healthcare environment.1Directly or indirectly through written words, health literacy skills are required in various aspects of doctor-patient dialogue, discussion of diagnostic and therapeutic plans, use of medical tools such as nebulizers or peak flow meters, health information, follow-up instructions, or administration of home medications. Poor health literacy is associated with several adverse health outcomes including increased incidence of chronic illness, poor intermediate disease markers, suboptimal use of preventative resources, and increased rates of hospitalization and use of emergency services.1,2 The potential impact of inadequate health literacy on health outcomes is significant. Almost half of all U.S. adults, approximately 90 million people, were found to have difficulty understanding and acting on health information in a 1992 literacy survey.3 This and the recent reports by the American Medical Association (AMA) and Institute of Medicine (IOM), highlighting the importance of health literacy and its impact on health care outcomes, indicate the increasing focus on this new field of study.1,4
Although significant, the issue of health literacy among patients seen in emergency departments (EDs) has received scant attention in emergency medicine literature. The often-quoted study by Williams et al.5 was performed more than a decade ago, using adult patients recruited from two adult EDs. In this 1995 study, 65% of adults had “adequate” health literacy. We undertook this pilot study to assess health literacy levels in parents or guardians of pediatric patients who presented to our ED for care. Among the patients seen in our nation’s EDs, pediatric patients (< 19 years) constitute one of the most vulnerable populations. Furthermore, pediatric visits are common, accounting for approximately 28% of the 100.4 million annual emergency visits in 2000.6 Anecdotal evidence suggests that ED personnel often presume that recurrent use of the ED by pediatric patients may be linked to socioeconomics, ethnicity, and literacy levels by parents or guardians of these children.7,8
This is an observational study conducted at a Midwestern urban university, tertiary referral, Level1 trauma center ED from May to August 2004. The study was approved by the local Institutional Review Board. The ED serves a greater metropolitan area of approximately three-quarters of a million people and has a census of 33,000 visits/year, with 24.6% pediatric patients (< 19 years of age). A single trained research assistant (RA) approached consecutive English-speaking parents or guardians of pediatric patients in a given eight-hour shift for participation in the study. Potential study subjects were identified using an online log of ED patients and were approached at the end of each patient’s visit to the ED. The timing of the subject solicitation was selected to minimize parent/guardian distraction and to preserve parent/guardian and patient privacy. A balanced rotating shift schedule (morning, evening, night) covering seven days per week was used to achieve a more representative sampling of the ED population. Parents/guardians were excluded if they had uncorrected impaired visual acuity, cognitive impairment (e.g., alcohol, drugs, trauma), required a language interpreter, or the pediatric patients they accompanied were pregnant or were subjects of a medical code or trauma team activation.
After verbal consent had been obtained and documented on the chart, the RA administered the English version of the abbreviated Test of Functional Health Literacy for Adults (s-TOFHLA) using standard instructions provided by the test maker. One of the authors (TPT) was licensed to use s-TOFHLA instrument (license #112/03) for research. Details on abbreviated s-TOFHLA are available elsewhere.9 Briefly, the abbreviated s-TOFHLA is a 36-item timed-reading comprehension test that measures health literacy skills of a patient in a realistic health care environment. Parents/guardians were asked to read two passages with every fifth or seventh word in the passages omitted, and to fill in the blanks from a list of four word choices. The first passage is a set of instructions for a patient in preparation for an upper gastrointestinal series. The second passage is taken from an applicant’s “Rights and Responsibilities” portion of a theoretical Medicaid application. The patient’s health literacy score reflects the number of correct answers and ranges from 0–36. Parents/guardians are considered to have “inadequate” health literacy if his/her abbreviated s-TOFHLA score is 0–16, “marginal” health literacy if score is 17–22, and “adequate” health literacy if score is 23–36.9
Along with the s-TOFHLA scores, demographic data, social, and medical information for the patients were abstracted from electronic medical records. Data were entered into an Excel® spreadsheet (Microsoft, Seattle, WA) and categorical variables were analyzed using Fisher’s exact (SigmaStat™, Point Richmond, CA). Data are reported with 95% exactconfidence interval (95% CI).
RESULTS
During the study period, 2,209 pediatric patients presented to the ED, out of 8,649 total patients (25.5%). Of these, 188 consecutive parents/guardians were approached, six did not consent or withdrew, and one had incomplete data, leaving 181 (96.28%) in the study. Of the 181 subjects, 162 (89.5%, 95% CI: 84.1%, 93.6%) scored in the “adequate” range (23–36), and 19 (10.5%) scored in the “marginal” or “inadequate” range [six participants (3.3%) scored in 0–12 range, 13 (7.2%) in 13–22 range]. The mean age for the pediatric patients was five years (interquartile range 2–11 years). Table 1summarizes the study results. Table 2 illustrates the clinical characteristics of our ED during the study period. There were no differences in health literacy levels by ethnicity, insurance status, age, gender, or medical disposition.
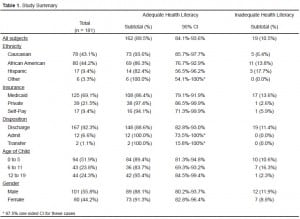
Study Summary
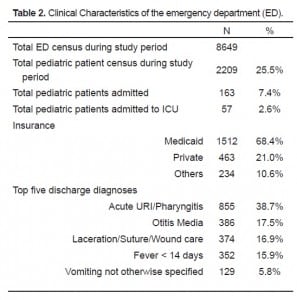
Clinical Characteristics of the emergency department (ED).
DISCUSSION
In this pilot study, almost nine out of 10 parents or guardians of pediatric patients had “adequate” health literacy, as measured by s-TOFHLA. Our findings, if validated in future multi-center studies, may have a significant impact on the way healthcare professionals interact and communicate with parents or guardians of children in the ED. In the subsequent discussion, we will briefly review health literacy and its impact on healthcare outcomes.
From humble beginnings, the last two decades have witnessed the maturity of what is now a legitimate field of study known officially as “health literacy.” Up to 1,000 papers link health literacy to general health, healthcare, and health outcomes.10 Limited health literacy skills have been associated with disparity in access to care, adverse health outcomes, increased hospitalization, higher healthcare costs, increased use of emergency services, ineffective communication, inability to understand informed consent, and inability to understand verbal and written medical advice.2,7,11,12 In the ED and clinic settings, low health literacy adversely impacts patient-physician dynamics, communication, patient satisfaction, and resource utilization.7,11–13 One approach healthcare professionals have taken to counter the effects of low health literacy is to tailor health-related communications to patients’ literacy and comprehension levels.14
Health literacy is commonly defined as “the degree to which individuals have the capacity to obtain, process, and understand basic information and services needed to make appropriate decisions regarding their health.”1 In the first U. S. government study of its kind, the 1992 National Adult Literacy Survey found that upward of 44 million Americans out of 191 million (23%) were functionally illiterate and 53.5 million (28%) had marginal reading skills.3 Although the term health literacy is closely related toliteracy – English-language reading skills – they are not the same. Health literacy is a potpourri of reading, comprehension, and computational skills that patients must possess to navigate effectively in a healthcare environment. Not only do patients need to know how to read, they need to know how to interpret their own health issues in the context of their healthcare environment to be health literate. Subsequent to the 1992 National Adult Literacy Survey, the U.S. Department of Education conducted the first national survey on health literacy. In this 2005 study, 35% of Americans were found to have “basic” or “below basic” health literacy.15
The two instruments most commonly used to approximate health literacy skills in the clinical setting include the Rapid Estimate of Adult Literacy in Medicine (REALM)16 and the Test of Functional Health Literacy in Adults (TOFHLA).17 While the REALM can be administered quickly (< 3 minutes), it does not measure comprehension. The TOFHLA, is more comprehensive but more time-consuming (> 20 minutes) to administer. In this study, we elected to use the shortened version of the TOFHLA (s-TOFHLA) because it is a good approximation of the full TOFHLA yet more practical (< 8 minutes) in the ED setting.9
Research has gained momentum in the last decade with the selection of health literacy as one of the 20 Healthy People 2010 objectives by the U.S. Department of Health and Human Services18 and 20 Priority Areas for National Action by the IOM;19 however, similar advances have not been observed in emergency medicine literature.2 To our knowledge, ours is one of the first two studies in the last decade that examined health literacy among parents or guardians who accompanied pediatric patients to the ED. Compared to Williams’s well known study,5 results from our study and those by Sanders et al.13suggest that parents or guardians of children seen in the ED tend to have higher health literacy skills–77.2% in Sanders’ and 89.5% in our study vs 65% in Williams’. One possible explanation for the differences is that health literacy declines with age. Since parents of pediatric patients tend to be younger, both studies that involve parents and guardians of children (Sanders and ours) report higher health literacy. Future studies are required to confirm our findings as well as the conclusions by Sanders.
Data in this study suggest two potentially important implications. First, if parents of pediatric patients seen in the ED are in fact more health literate, ED professionals may need to adjust the patient-doctor communications accordingly. Second, fresh health literacy data are needed in the current debates regarding access to emergency care. For example, some arguments for limited access to emergency care are fueled in part by the assumption that poor health literacy may cause over-utilization of emergency services.8New data may thus impact policy-making decisions regarding ED access in the future.
When the “adequate” group was compared to the “marginal/inadequate” group for any predictors of poor health literacy, no evidence emerged that ethnicity, insurance status, medical disposition, age, or gender predicted or predisposed any particular group of patients to inadequate health literacy (Table 1). In our study, pediatric patients accounted for approximately a quarter of our ED visits, with a payer mix that included 68% Medicaid patients (Table 2).
LIMITATIONS
This was a pilot study using convenience sampling of English-speaking subjects at a single site in the Midwest. Results should not be generalized to regional or national ED populations. Although a rolling enrollment design was employed, the study sample was only a small fraction of eligible patients seen in the ED during the study period. The possibility of a non-representative population could not be excluded. We did not include the Spanish version of s-TOFHLA because of the required training in cultural competency and interpreter quality. This exclusion of Spanish-speaking subjects may also have skewed the results. During the study period, however, the Spanish-speaking pediatric patients (requiring a Spanish interpreter) made up a small fraction (5.78%) of our ED’s pediatric patient census.
CONCLUSION
A large majority (89.5%) of English-speaking parents or guardians of pediatric patients evaluated in the ED have adequate health literacy. This high prevalence of health literacy may prompt ED professionals to adjust their communication styles in the evaluation of children seen in the ED. While the data from this study may prompt ED professionals to adjust their communication styles in the evaluation of children, future multi-center studies are needed to confirm these findings.
Footnotes
The authors would like to thank Jane Meza, Ph.D., Department of Preventative and Societal Medicine, University of Nebraska Medical Center, for her statistical assistance.
Supervising Section Editor: Paul Walsh, MD, MSc
Submission history: Submitted October 16, 2007; Revision Received March 31, 2008; Accepted April 5, 2008
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Paul Tran, MD, Department of Emergency Medicine, University of Nebraska Medical Center, 981150 Nebraska Medical Center, Omaha, NE 68198-1150
Email: trtran@unmc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Nielsen-Bohlman L. Health literacy:A Prescription To End Confusion. Washington, DC: National Academies Press; 2004. Institute of Medicine & Committee on Health Literacy.
2. Berkman ND, et al. Literacy and health outcomes. Evid Rep Technol Assess (Summ)2004;87:1–8. [PubMed]
3. Kirsch IS. Adult literacy in America: A first look at the results of the National Adult Literacy Survey. Washington, DC: Office of Educational Research and Improvement, U.S. Dept. of Education; 1993. Educational Testing Service & National Center for Education Statistics.
4. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health Literacy: Report of the Council on Scientific Affairs. JAMA.1999;281:552–557. [PubMed]
5. Williams MV, et al. Inadequate functional health literacy among patients at two public hospitals. JAMA. 1995;274:1677–1682. [PubMed]
6. McCaig LF. National Hospital Ambulatory Medical Care Survey: 1998 emergency department summary. Adv Data. 2000:1–23.
7. Halfon N, Newacheck PW, Wood DL, St Peter RF. Routine emergency department use for sick care by children in the United States. Pediatrics. 1996;98:28–34. [PubMed]
8. Vastag B. Low Health Literacy Called a Major Problem. JAMA. 2004;291:2181–2182.[PubMed]
9. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 199;38:33–42. [PubMed]
10. Rudd RE. Health literacy skills of U.S. adults. Am J Health Behav. 2007;31:S8–S18.[PubMed]
11. Baker DW, et al. Health literacy and use of outpatient physician services by Medicare managed care enrollees. J Gen Intern Med. 2004;19:215–220. [PMC free article][PubMed]
12. Davis TC, Wolf MS. Health literacy: implications for family medicine. Fam Med.2004;36:595–598. [PubMed]
13. Sanders LM, Thompson VT, Wilkinson JD. Caregiver health literacy and the use of child health services. Pediatrics. 2007;119:e86–e92. [PubMed]
14. Williams MV, Davis T, Parker RM, Weiss BD. The role of health literacy in patient-physician communication. Fam Med. 2002;34:383–389. [PubMed]
15. Kutner MA. National Center for Education Statistics. The health literacy of America’s adults results from the 2003 National Assessment of Adult Literacy. Washington, DC: U.S. Dept of Education, National Center for Education Statistics; 2006.
16. Davis TC, et al. Rapid assessment of literacy levels of adult primary care patients.Fam Med. 1991;23:433–435. [PubMed]
17. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med.1995;10:537–541. [PubMed]
18. U.S. Department of Health and Human Services. Prevention and Health Promotion. Healthy People 2010. Nasnewsletter. 2000;15:3. [PubMed]
19. Adams K, Corrigan J. Institute of Medicine, Committee on Identifying Priority Areas for Quality Improvement. Priority areas for national action transforming health care quality. Washington, DC: National Acad. Press; 2003.


