| Author | Affiliation |
|---|---|
| Pamela Yamamoto Swan, BA | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
| Beverly Nighswonger, RN | Emergency Medical Services, Orange County California Health Care Agency, Santa Ana, CA |
| Gregory L. Boswell, RN | Emergency Medical Services, Orange County California Health Care Agency, Santa Ana, CA |
| Samuel J. Stratton, MD, MPH | University of California, Irvine School of Medicine, Department of Emergency Medicine, Orange, CA |
ABSTRACT
Introduction:
In 2005, Orange County California Emergency Medical Services (EMS) initiated a field 12-lead program to minimize time to emergency percutaneous coronary intervention (PCI) for field-identified acute myocardial infarction (MI). As the program matured, “false-positive” (defined as no PCI or coronary artery occlusion upon PCI) field MI activations have been identified as a problem for the program. To identify potentially correctable factors associated with false-positive EMS triage to PCI centers.
Methods:
This was a retrospective, outcome study of EMS 12-lead cases from February 2006 to June 2007. The study system exclusively used cardiac monitor internal interpretation algorithms indicating an acute myocardial infarction as the basis for triage. Indicators and variables were defined prior to the study. Data, including outcome, was from the Orange County EMS database, which included copies of 12-lead ECGs used for field triage. Negative odds ratios (OR) of less than 1.0 for positive PCI were the statistical measure of interest.
Results:
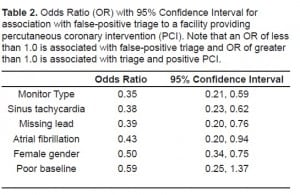
Five hundred forty-eight patients were triaged from the field for PCI. We excluded 19 cases from the study because of death prior to PCI, refusal of PCI, and co-morbid illness (sepsis, altered consciousness) that precluded PCI. Three hundred ninety-three (74.3%) patients had PCI with significant coronary lesions found. False-positive field triages were associated with underlying cardiac rhythm of sinus tachycardia [OR = 0.38 (95% CI 0.23, 0.62)]; atrial fibrillation [OR = 0.43 (95% CI = 0.20, 0.94)]; an ECG lead not recorded [OR = 0.39 (95% CI = 0.20, 0.76)]; poor ECG baseline [OR = 0.59 (95% CI = 0.25, 1.37)]; One of three brands of monitors used in the field [OR = 0.35 (95% CI = 0.21, 0.59)]; and female gender [OR = 0.50 (95% CI = 0.34, 0.75)]. Age was not associated with false-positive triage as determined by ordinal regression (p=1.00).
Conclusion:
For the urban-suburban EMS field 12-lead program studied, age was not associated with false-positive triage. It was unexpected that female gender was associated with false-positive triage. False-positive triage from the field was associated with poor ECG acquisition, underlying rhythms of atrial fibrillation and sinus tachycardia, and one brand of 12-lead monitor.
INTRODUCTION
Studies have shown that percutaneous coronary intervention (PCI) may be preferred over intravenous thrombolytics in achieving reperfusion and reducing mortality for those presenting to an emergency department (ED) with acute myocardial infarction and associated electrocardiographic ST segment elevation (STEMI).1–4 It has also been shown that myocardial reperfusion after onset of a STEMI has greater effectiveness the sooner it is achieved.5 A time period of less than 90 minutes from the time a STEMI victim enters an ED to having PCI with balloon inflation and reperfusion of a blocked coronary artery has become a standard goal in many developed countries.4
In the U.S. it has been found that a majority of adults (75%) live closest to a hospital that does not provide PCI.6 While patients with STEMI can initially be stabilized at a non-PCI provider hospital and transferred by critical care ambulance to a PCI capable facility, studies show that the time for initiation of PCI can be significantly reduced when emergency medical services (EMS) personnel identify STEMI victims in the field and transport them directly to a PCI capable hospital.7–10 To facilitate field triage of potential STEMI patients to PCI centers, many EMS systems have developed prehospital 12-lead electrocardiography (12-lead) protocols that allow EMS personnel at the scene to obtain data and triage a potential STEMI patient directly to a PCI capable facility.11–14 Reducing time in the field before arrival to a PCI center further decreases overall time for reperfusion of occluded coronary arteries.9,10
Three common models are used for EMS field 12-lead identification of potential STEMI. 14 The least expensive model is use of an algorithm interpretation preprogrammed within the cardiac monitor that rapidly generates the field 12-lead. This method for field interpretation requires no wireless or electrical transmission system and allows for 12-lead acquisition and STEMI determination without intensive education of EMS field providers. A second method, using paramedic interpretation, requires training of EMS personnel in the interpretation of the various 12-lead signs of STEMI. While training and maintaining the skill of EMS personnel interpretation may be costly, it has been shown to be effective with paramedic-identified STEMI sensitivity ranging from 71% to 97% and specificity ranging from 91% to 100%.14 A final method is wireless and electronically transmits a field-acquired 12-lead to a physician for interpretation. This method is costly and may add to time a STEMI patient is in the field while 12-lead transmission is accomplished. In addition, some systems may require significant effort or cost to have a physician or other personnel trained in ECG interpretation available at all times to read the transmitted ECG.
While the monitor algorithm STEMI determination method described above is rapid and inexpensive, false-positive field triage to a PCI center is a concern.14 One result of false-positive triage is the unnecessary rapid transport of assumed critical patients beyond a nearby hospital to a more distant PCI facility, placing emergency response crews and the community at increased risk for motor vehicle accidents.15 It can also result in unnecessary redirection of personnel and equipment at the receiving hospital. In addition, when emergency response personnel are assigned to a false-positive incident, fewer available units remain in the area. A decrease in false-positive field STEMI triages could result in better utilization of resources and allow for safer EMS operations. Another adverse effect of excessive false-positive triages could be the decreased willingness of the emergency physician to allow direct transportation to a PCI center without having first personally interpreted the ECG.
Considering the above discussion, minimization of EMS false-positive STEMI transports when using a monitor algorithm exclusive triage system would benefit a healthcare system. To address the issue, this study was designed to identify the rate and variables associated with false-positive triage within an EMS monitor algorithm interpretation triage system.
METHODS
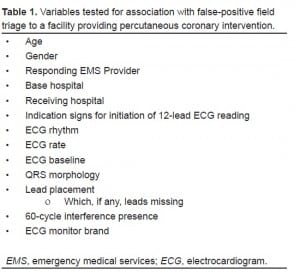
This was a retrospective, sequential, case-control outcome study of EMS responses triaged in the field to designated PCI-capable hospitals. Study variables of interest were those that may have been associated with false-positive field triage for PCI. Potential variables to test for a potential false-positive association were identified in a pre-study (Table 1). Cases considered for the study included all those triaged from the field to a PCI center by exclusive use of a 12-lead monitor algorithm that included the terms “Acute MI Suspected” or “Acute MI.” Indications for obtaining a 12-lead ECG reading were chest pain, shortness of breath, dizziness or syncope. Excluded from the study were cases appropriate for triage to a PCI but for whom cardiac arrest and death prior to PCI occurred or who had co-morbid conditions that precluded PCI. These co-morbid conditions included sepsis, decreased mental capacity that did not allow for PCI consent, diabetic ketoacidosis, acute cerebral vascular accident, concurrent trauma with hemorrhage, and refusal of a competent person to consent for PCI.
A code book defining study variables was developed before conducting the study. We validated the code book by first collecting data for 20 patients who met criteria for inclusion. We clarified inconsistent terms and variables to ensure that study definitions were standardized. Data was collected on a collection form that used field and receiving hospital records with a copy of the original field 12-lead attached. We developed a database using Microsoft Excel 2003 (Microsoft Corp, Redmond, WA, USA), and used a double data entry method to enter data. We corrected errors when conflicting data were entered. If a conflict in interpretation still existed, the senior investigator’s entry took precedence for consistency. Prior to the study we determined that for interpretation of odds ratios (OR), a confidence interval precision of 10% or less was necessary for the findings to be clinically significant. Using this assumption, the number of cases needed for adequate sample size was determined to be at least 500, based on a desired power of 80%. We conducted this power calculation using Statistics with Confidence v2.0 software (CIA Software, Bristol, UK).
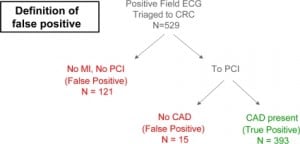
For this study, false-positive triage was the outcome of interest. Because there is potential for variability in the definition for false-positive, we used a conservative definition indicating no acute coronary artery occlusion (disease). False-positive was defined as a patient who had no significant coronary artery occlusion by PCI or was determined after evaluation by receiving PCI-center physicians to lack need for PCI (Figure 1). We used SPSS v13.0 software (SPSS Inc, Chicago, Il, USA) to calculate OR for association of each study variable and positive PCI outcome. Therefore, a reported OR of less than 1.0 was associated with false-positive triage. Confidence intervals (95%) were calculated for each OR to determine precision of the statistical estimate. For age as a variable, we used ordinal regression for statistical analysis, with a p-value of less than 0.05 considered significant.
The study setting was Orange County, California with a population of 3.02 million persons living in an urban-suburban environment. EMS units were 911 computer-aided-dispatched with a two-tiered basic life support (BLS)-advanced life support (ALS) response. Thirteen fire departments with 880 paramedics provided ALS resources and transported to 25 receiving hospitals of which 12 were designated PCI centers. Field medical control was provided by blended off-line protocols and on-line base hospital radio contact.
This study received Institutional Review Board approval by a committee recognized by Federal-wide Assurance submitted to the U.S. Department of Health and Human Services.
RESULTS
Paramedics triaged 548 sequential patients from the field for PCI during the study period. Nineteen cases were excluded because of cardiac arrest prior to PCI or co-morbid conditions that precluded PCI. During the study, three types of field 12-lead cardiac monitors were used: the Zoll M Series (Zoll Medical Corp., Chelmsford, MA, USA); LifePAK 12 (Physio-Control, Inc., Redmond, WA, USA); and the Philips HeartStart Rx (Philips Electronics, Amsterdam, Netherlands). The average age for those entered into the study was 64.7 years with 60.0% male. Of the 529 cases included, 393 (74.3%) patients had PCI with coronary lesions treated by balloon angioplasty or coronary artery bypass graft. The remaining 136 (25.7%) were considered false-positives, defined as a patient who was determined after evaluation by receiving PCI-center physicians to lack need for PCI (121; 22.9%) or had no coronary artery occlusion by PCI (15; 2.8%) (Figure 1). False-positive cases were associated with the following variables: a specific brand of one of three monitors used in the system (OR = 0.35, 95% CI = 0.21, 0.59); sinus tachycardia (OR = 0.38, 95% CI = 0.23, 0.62); missing lead recording on 12-lead printout (0.39, 95% CI = 0.20, 0.76); atrial fibrillation (OR = 0.43, 95% CI = 0.20, 0.94); female gender (OR = 0.50, 95% CI = 0.34, 0.75); and poor ECG baseline (OR = 0.59, 95% CI = 0.25, 1.37) (Table 2). Age was not associated with false-positive triage for PCI as determined by Ordinal Regression (p = 1.00).
DISCUSSION
This study showed a substantial number (25.7%) of false-positive triages to specialty centers for PCI based on field 12-lead monitor algorithms. We found multiple variables associated with false-positive triage within the EMS system studied.
Poor ECG baseline and failure to record all 12 leads for machine algorithm interpretation are false-positive associated variables that can be addressed by improved quality in field acquisition of 12-leads. Variables more difficult to address are sinus tachycardia and atrial fibrillation, which had a tendency to be wrongly interpreted by machine algorithm as acute MI. EMS system adjustments to disregard readings of acute MI in the setting of sinus tachycardia and atrial fibrillation could result in missing true MI patients and would require further study to insure the rate of missed true positives is not unacceptable. An unexpected finding was the association of one type of 12-lead machine with false-positive triage. Once this was re-validated by repeat data analysis, we advised the device manufacturer of the findings. Adjustments and changes to the algorithm for the device have been made and follow-up study is in progress. The type of monitor associated with false-positive 12-leads is not identified in this paper because the oversight Institutional Review Committee for the study requires that a written release from the manufacturer be obtained and such a release was declined.
Another interesting finding was an association of false-positive triage with female gender. We collected demographic data with the intent to show that the study population was homogenous with no difference in gender outcomes. The association of female gender with false-positive triage was unexpected and deserves further study for confirmation and explanation.
Field EMS determination of STEMI has been shown to be beneficial in rapid identification, transport, treatment, and decreased mortality.7,11,16 To maximize this benefit and decrease the problems earlier described for false-positive triage, this study suggests that in addition to the mechanics of attaining a field ECG, additional paramedic education may be required to help recognize ST elevation MI in field ECG recordings.
In a 2008 article Ting et al.14 noted that current knowledge of false-positive and false-negative rates for EMS triage of STEMI patients to PCI centers is poorly characterized, supporting the findings of this paper. Their study describes poor field ECG acquisition as a factor associated with false-positive triage, and finds that movement artifact, lead misplacement, and poor skin contact can cause the poor-quality tracings that can be misinterpreted by ECG monitor software or EMS personnel.
Decreasing false-positive system activation could inadvertently increase false-negatives. To mitigate this adverse effect, it has been suggested that electronic transmission of 12-lead ECG to a receiving hospital for over-read may be effective.17
LIMITATIONS
One limitation of this study is the retrospective method used for data acquisition. The retrospective method increases risk for loss of original data, erroneous recording of data elements on original records, selection bias, and confounding due to lack of control of study variables. A more subtle limitation is that our definition of false-positive triage does not take into account patients who were determined by the receiving physicians to lack evidence for an acute STEMI MI, when in fact such an MI was present and PCI could have been a benefit. Studies show there is a background risk that approximately 3% of MI patients requiring PCI will be misdiagnosed and discharged by cardiologists without appropriate coronary intervention, and approximately 6–10% by emergency physicians.18,19
While left bundle branch block was analyzed within the study population 12-leads, there was not an association of this finding with false-positive triage; on the other hand the study was limited in that we did not test for false-positive association with left ventricular hypertrophy, pericarditis, left ventricular aneurysm, and early repolarization.
Another limitation is the focus on false-positive triage and lack of data for false-negative cases. This study does not consider patients who were false-negatives. Knowing the false-negatives would have allowed for better system description and calculation of field 12-lead sensitivity and specificity.
And because we conducted this study in an urban-suburban setting with multiple hospital options within a few minutes transport time, the findings may lack external validity. Additionally, selection bias by paramedics could have occurred in that some cases eligible for 12-lead application may not have had an ECG. Finally, outcomes were obtained from hospital billing and discharge databases and not independently confirmed.
CONCLUSION
For the EMS field 12-lead program studied, there was a false-positive triage rate of 25.7%. False-positive field triage was associated with one brand of 12-lead ECG monitor, poor ECG acquisition, and underlying rhythms of sinus tachycardia and atrial fibrillation. Unexpectedly, female gender was also associated with false-positive triage. Age was not associated with false-positive field triage for PCI.
Footnotes
This paper is dedicated to Beverly Nighswonger, RN, who passed away October 29, 2008. She was a dedicated professional of highest ethics. In her shortened lifetime, she accomplished more than most and was generous to all.
Supervising Section Editor: Christopher Kahn, MD, MPH
Submission history: Submitted April 15, 2009; Revision Received May 28, 2009; Accepted June 1, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Samuel J. Stratton, MD, MPH Health Disaster Management/Emergency Medical Services, Orange County Health Care Agency, 405 W. Fifth Street, Suite 301A, Santa Ana, CA 92701
Email sstratton@att.net
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Grines CL, Browne KF, Marco J, et al. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med. 1993;328:673–9. [PubMed]
2. Weaver WD, Simes RJ, Betriu A, et al. Comparison of primary coronary angiography and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA.1997;278:2093–8. [PubMed]
3. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet. 2003;361:13–20.[PubMed]
4. Pollack CV, Antman EM, Hollander JE. 2007 focused update to the ACC/AHA Guidelines for the management of patients with ST-segment elevation myocardial infarction: implications for emergency department practice. Ann Emerg Med. 2008;52:344–55. [PubMed]
5. McNamara RL, Wang Y, Herrin J, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–96. [PubMed]
6. Nallamothu BK, Bates ER, Wang Y, et al. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113:1189–95. [PubMed]
7. van’t Hof AW, Rasoul S, van de Wetering H, et al. Feasibility and benefit of prehospital diagnosis, triage, and therapy by paramedics only in patients who are candidates for primary angioplasty for acute myocardial infarction. Am Heart J. 2006;151:1255.e1–5. [PubMed]
8. Afolabi BA, Novaro GM, Pinski SL, et al. Use of the prehospital ECG improves door-to-balloon times in ST segment elevation myocardial infarction irrespective of time of day or day of week.Emerg Med J. 2007;24:588–91. [PMC free article] [PubMed]
9. Brown JP, Mahmud E, Dunford JV, et al. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-balloon time in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2008;101:158–161. [PubMed]
10. Le May MR, So DY, Dionne R, et al. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2008;358:231–40. [PubMed]
11. Le May MR, Davies RF, Dionne R, et al. Comparison of early mortality of paramedic-diagnosed ST-segment elevation myocardial infarction with immediate transport to a designated primary percutaneous coronary intervention center to that of similar patients transported to the nearest hospital. Am J Cardiol. 2006;98:1329–33. [PubMed]
12. Johnston S, Brightwell R, Ziman M. Paramedics and pre-hospital management of acute myocardial infarction: diagnosis and reperfusion. Emerg Med J. 2006;23:331–334. [PMC free article][PubMed]
13. Dhruva VN, Abdelhadi SI, Anis A, et al. ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction (STAT-MI) trial. J Am Coll Cardiol. 2007;50:509–13. [PubMed]
14. Ting HH, Krumholz HM, Bradley EH, et al. Implementation and integration of prehospital ECGs into systems of care for acute coronary syndrome: a scientific statement from the American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research, Emergency Cardiovascular Care Committee, Council on Cardiovascular Nursing, and Council on Clinical Cardiology. Circulation. 2008;118:1066–79. [PubMed]
15. Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehosp Emerg Care. 2001;5:261–269. [PubMed]
16. Feldman JA, Brinsfield K, Bernard S, et al. Real-time paramedic compared with blinded physician identification of ST-segment elevation myocardial infarction: results of an observational study. Am J Emerg Med. 2005;23:443–448. [PubMed]
17. Davis DP, Graydon C, Stein R, et al. The positive predictive value of paramedic versus emergency physician interpretation of the prehospital 12-lead electrocardiogram. Prehosp Emerg Care.2007;11:399–402. [PubMed]
18. Turnipseed SD, Bair AE, Kirk JD, et al. Electrocardiogram differentiation of benign early repolarization versus acute myocardial infarction by emergency physicians and cardiologists. Acad Emerg Med. 2006;13:961–966. [PubMed]
19. Brady WJ, Perron A, Ullman E. Errors in emergency physician interpretation of ST-segment elevation in emergency department chest pain patients. Acad Emerg Med. 2000;7:1256–60.[PubMed]


