| Author | Affiliation |
|---|---|
| Jody A. Vogel, MD | Denver Health Medical Center, Department of Emergency Medicine, Denver, Colorado |
| Adit A. Ginde, MD, MPH | University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
| Steven R. Lowenstein, MD, MPH | University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
| Marian E. Betz, MD, MPH | University of Colorado School of Medicine, Department of Emergency Medicine, Aurora, Colorado |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction:
To describe the epidemiology and characteristics of emergency department (ED) visits by older adults for motor vehicle collisions (MVC) in the United States (U.S.).
Methods:
We analyzed ED visits for MVCs using data from the 2003–2007 National Hospital Ambulatory Medical Care Survey (NHAMCS). Using U.S. Census data, we calculated annual incidence rates of driver or passenger MVC-related ED visits and examined visit characteristics, including triage acuity, tests performed and hospital admission or discharge. We compared older (65+ years) and younger (18–64 years) MVC patients and calculated odds ratios (OR) and 95% confidence intervals (CIs) to measure the strength of associations between age group and various visit characteristics. Multivariable logistic regression was used to identify independent predictors of admissions for MVC-related injuries among older adults.
Results:
From 2003–2007, there were an average of 237,000 annual ED visits by older adults for MVCs. The annual ED visit rate for MVCs was 6.4 (95% CI 4.6–8.3) visits per 1,000 for older adults and 16.4 (95% CI 14.0–18.8) visits per 1,000 for younger adults. Compared to younger MVC patients, after adjustment for gender, race and ethnicity, older MVC patients were more likely to have at least one imaging study performed (OR 3.69, 95% CI 1.46–9.36). Older MVC patients were not significantly more likely to arrive by ambulance (OR 1.47; 95% CI 0.76–2.86), have a high triage acuity (OR 1.56; 95% CI 0.77–3.14), or to have a diagnosis of a head, spinal cord or torso injury (OR 0.97; 95% CI 0.42–2.23) as compared to younger MVC patients after adjustment for gender, race and ethnicity. Overall, 14.5% (95% CI 9.8–19.2) of older MVC patients and 6.1% (95% CI 4.8–7.5) of younger MVC patients were admitted to the hospital. There was also a non-statistically significant trend toward hospital admission for older versus younger MVC patients (OR 1.78; 95% CI 0.71–4.43), and admission to the ICU if hospitalized (OR 6.9, 95% CI 0.9–51.9), after adjustment for gender, race, ethnicity, and injury acuity. Markers of injury acuity studied included EMS arrival, high triage acuity category, ED imaging, and diagnosis of a head, spinal cord or internal injury.
Conclusion:
Although ED visits after MVC for older adults are less common per capita, older adults are more commonly admitted to the hospital and ICU. Older MVC victims require significant ED resources in terms of diagnostic imaging as compared to younger MVC patients. As the U.S. population ages, and as older adults continue to drive, EDs will have to allocate appropriate resources and develop diagnostic and treatment protocols to care for the increased volume of older adult MVC victims.
INTRODUCTION
Background
Currently, there are approximately 30 million licensed drivers in the United States (U.S.) who are over the age of 65.1 As the older adult population grows, it is anticipated that the number of older drivers will also increase; by the year 2030, an estimated 57 million drivers will be over the age of 65.2,3 Drivers over age 65 have higher rates of motor vehicle crashes (MVCs) per mile driven. On a per-crash basis, older motorists also have higher rates of death4,5 and serious injury, and incur greater costs for acute care and rehabilitation.6 Compared to other types of trauma in older adults, MVCs are responsible for the largest number of intensive care unit days and overall hospital charges.7 In addition, while only 10% of trauma patients are over the age of 65 years, they accrue an estimated 25 percent of total hospital costs for trauma care.7
Among adults aged 65 years and older, MVCs are the second leading cause of injury-related death and the fourth-leading cause of injury-related emergency department (ED) visits.8 As the U.S. population ages, and as older adults continue to drive, EDs will have to allocate appropriate resources and develop diagnostic and treatment protocols to care for the increased volume of older adult MVC victims. Previous research to investigate the care of older adults with MVC-related injuries has focused on the pain management9 and inpatient characteristics of these patients.10–14 However, less is known about how ED visits after MVCs by older patients compare to those by younger patients. Given older adults’ increased propensity for injury from a given mechanism and their decreased physiologic reserve,10–11 we hypothesized that older MVC patients would require more ED resources and would be more likely to be admitted to the hospital after MVC-related injuries when compared to younger MVC patients.
The primary objective of this study was to use a national, population-based data set to examine the demographic and visit-related characteristics of older adults presenting to EDs after motor vehicle crashes. Specifically, we sought to: (1) compare the characteristics of MVC-related ED visits by older (65+ years) and younger (18–64 years) adults in terms of emergency medical services (EMS) arrival, visit acuity, use of imaging studies, and injury diagnoses; and (2) compare the likelihood of hospitalization of older and younger MVC patients, after adjustment for injury severity.
METHODS
Study Design and Setting
We conducted a cross-sectional analysis of visits to EDs for MVCs in the United States using 2003–2007 data from the National Hospital Ambulatory Medical Care Survey (NHAMCS). These surveys are conducted annually by the National Center for Health Statistics and use multi-stage probability sampling to derive national estimates of patient visits. The NHAMCS design is based on: primary sampling units within geographic areas; nonfederal, acute care general hospitals within those primary sampling units; EDs within those hospitals; and patients within those EDs. The NHAMCS data files include a patient-weighting variable for generating national estimates based on sampling designs and response rates adjusted for non-response. Detailed descriptions of the survey methodologies are available in the technical documentation that accompanies the data set.15
Between 2003 and 2007, an annual average sample of 438 EDs was included in NHAMCS, which represents approximately 10 percent of all U.S. EDs (based on American Hospital Association ED Counts).16 Hospital staff in the sampled EDs completed patient record forms for a systematic random sample of visits during a randomly assigned 4-week period. The overall annual average sampling response rate between 2003 and 2007 was 89.4% across all EDs.
We defined visits in the NHAMCS data files as MVC-related using the cited external causes of injury, which are the activities from which the injury resulted. Each visit has up to 3 external causes cited; we clustered these using the Centers for Disease Control and Prevention’s (CDC) groupings of ICD-9 CM External Causes of Injury and Poisoning codes.17 Specifically, we included ED visits with at least 1 external cause from a traffic-related MVC (E810-E816; E818-E819; E823). We excluded an estimated 1.58 million motor vehicle injury visits (n = 469 observations) that resulted from off-road motor vehicle crashes (e.g., dirt bikes or snowmobiles) or injuries resulting from a stationary vehicle (e.g., slammed finger in car door or fall from vehicle); these accounted for 9% of all motor vehicle injury visits for adults aged 18 and older. The NHAMCS files also contain questions concerning the episode of care (“initial visit”; “follow-up visit”; “unknown”) and the duration of the injury problem (“acute problem, <3 months onset”; “routine chronic problem”; “flare-up of chronic problem”; “pre-/post-surgery”; “preventive care”). For this analysis, we were interested in the total burden of MVC-related ED visits, so we included all episodes of care and all durations of injuries.
For this analysis, we categorized patients into 2 age groups: younger adults (aged 18–64 years) and older adults (≥65 years). The surveys included separate variables for race (white, black, Asian, Native Hawaiian/other Pacific Islander, Native Alaskan/American Indian, and ≥2 races reported) and ethnicity (Hispanic, non-Hispanic and unknown/blank). Because of the high proportion of missing ethnicity data in all of the surveys (range 15.1%–21.9%), we used the imputed ethnicity variable (Hispanic and non-Hispanic).
We further categorized the MVC-related injuries reported using the CDC’s Barrell Injury Diagnosis Matrix, which classifies injuries based upon body region and nature of injury; we defined a “significant injury diagnosis” as an ICD-9 diagnosis of a traumatic brain, spinal cord or internal torso injury.18 Metropolitan statistical areas were classified in the survey data using definitions from the U.S. Census Bureau.16 As proxies for injury severity, variables of interest included significant injury diagnoses; EMS arrival (yes or no); high triage acuity (level 1 or 2, versus levels 3 to 5); and ED imaging (at least radiography, computed tomography or magnetic resonance image study) as identified in the NHAMCS database.
This study was deemed exempt from review by the local institutional review board.
Primary Data Analysis
The data analysis proceeded in 3 steps. First, we estimated the number (reported as a weighted estimate and proportion) and population-based incidence rates of driver or passenger MVC-related ED visits for younger and older adults. Rates were calculated per 1000 population using annual denominators based on the civilian, non-institutionalized U.S. population for 2003–2007, as estimated by the U.S. Census Bureau.18
Second, we used logistic regression to test for associations between age and each of the ED visit characteristics of interest (EMS arrival, triage level, ED imaging, and significant injury diagnosis). We decided a priori to simultaneously adjust for potential confounders including gender, race (white versus other) and Hispanic ethnicity, since these demographic characteristics could impact the age distribution of MVC patients, arrival by EMS, and the decision to assign a high triage acuity or order an imaging study. To measure the strength of these relationships, we calculated adjusted odds ratios (OR) with 95% confidence intervals (CIs).
Third, to examine the association between age and hospital admission, we conducted an additional multivariable logistic regression. Hospital admission was the dependent variable, and age group, gender, race, ethnicity, and markers of injury severity (EMS arrival, high triage acuity, imaging studies performed, and injury diagnosis) were identified a priori to be included simultaneously as factors that could be related to hospitalization after injury. We performed all data analysis using Stata 11.0 (Stata Corporation, College Station, TX), using the program commands designed for analysis of weighted survey data.
RESULTS
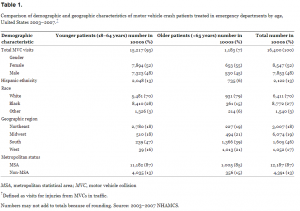
From 2003–2007, there were an average of 237,000 annual ED visits by older adults for MVCs (Table 1). MVC-related visits accounted for 1.4% (95% CI 1.2–1.6) of ED visits by older adults, as compared with 4.3% (95% CI 4.1–4.6) of ED visits for younger adults. The annual ED visit rate for MVCs was 6.4 (95% CI 4.6–8.3) visits per 1,000 for older adults and 16.4 (95% CI 14.0–18.8) visits per 1,000 for younger adults. The proportion of MVC-related visits among older and younger adults did not differ significantly by gender, geographic region or metropolitan status. Although blacks accounted for a greater proportion of younger MVC patients (27.6%; 95% CI 24.3–30.9) than older MVC patients (15.3%; 95% CI 10.7–19.9), they also accounted for a larger proportion of all ED presentations by younger patients (24.4%, 95% CI 21.8–26.9) than by older patients (14.0%, 95% CI 12.2–15.8).
Approximately half of MVC patients were transported by ambulance or had a high triage acuity (Level 1 or 2; Table 2). There was a non-statistically significant trend for older MVC patients as compared to younger MVC patients to be transported by ambulance (OR 1.47, 95% CI 0.76–2.86) or to have a high triage acuity (OR 1.56, 95% CI 0.77–3.14) after adjustment for gender, race and ethnicity. However, after adjusting for other variables, older MVC patients were significantly more likely than younger MVC patients to have at least 1 imaging study performed in the ED (OR 3.69, 95% CI 1.46–9.36). Approximately 15% (95% CI 13.5–16.4) of ED visits for MVCs—or 2.5 million visits by adults aged 18 and older—resulted in a diagnosis of a head, spinal cord or torso injury, without significant differences between older and younger patients after adjustment for gender, race and ethnicity (OR 0.97, 95% CI 0.42–2.23).
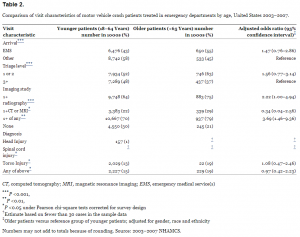
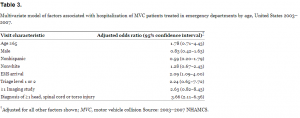
Overall, 14.5% (95% CI 9.8–19.2) of older MVC patients and 6.1% (95% CI 4.8–7.5) of younger MVC patients were admitted to the hospital. After controlling for gender, race, ethnicity, and injury severity (EMS arrival, high triage acuity, ED imaging, and diagnosis of a head, spinal cord or internal injury), there was a trend for older MVC patients to be admitted to the hospital as compared to younger MVC patients (OR 1.78, 95% CI 0.71–4.43) (Table 3). Of MVC patients hospitalized, 2.3% of older patients and 1.2% of younger patients were admitted to an intensive care unit (ICU). Older MVC patients had a higher odds than younger MVC patients to be admitted to the ICU if hospitalized (OR 6.86, 95% CI 0.91–51.90) after adjustment for gender, race, ethnicity, and markers for injury severity, although this also was not statistically significant and younger patients accounted for a much larger absolute volume of total estimated MVC-related ICU admissions (189,000) compared with older patients (28,000).
DISCUSSION
Between 2003 and 2007, there were 1.2 million MVC-related ED visits by older adults. As the number of older adult drivers continues to rise, it is anticipated that the annual ED visit volume for older MVC victims will also increase. As such, understanding the healthcare resources used by these patients will be increasingly important to inform diagnostic and treatment protocols for older MVC patients. In this analysis of 5 years of data, we found that older MVC patients were more likely than younger ones to have imaging studies performed but were equally likely to have a final ED diagnosis of a head, spinal cord or torso injury or to be admitted to the hospital.
In general, older adults have an increased propensity for injury and decreased physiologic reserve to respond to injury.10–14,19 As individuals age, physical changes in bone density, muscle mass and tissue pliability lead to decreased ability to tolerate forces experienced in an MVC with a consequential increased susceptibility to injury.20 These same physical changes can also lower an older adult’s physiologic reserve to compensate and heal from injury. In this study, however, no trend was identified to suggest that older MVC patients were more likely than younger ones to have a head, spinal cord or torso injury based on their final ED diagnoses. It is possible that this somewhat surprising finding may be a result of the small subgroup sample sizes (which did not allow for stable estimate generation) or from the age categories we used, but it does merit further investigation in the future.
Older adults’ generally increased propensity for injury and decreased physiologic reserve may be important to consider in the determination of triage criteria and decision rules for imaging in the older adult population. Indeed, we found a trend toward ED visits by older MVC patients to have a higher triage acuity level as compared to younger MVC patients, which may reflect triage consideration of age, although the difference was not statistically significant. Previous research suggests that the emergency severity index is a valid tool to predict hospitalization, length of stay, and 1-year survival in older adult trauma patients.21
Over three-fourths of ED visits for older MVC patients included imaging studies, and older patients were more likely than younger ones to have at least 1 imaging study performed, after adjustment for gender, race and ethnicity. The high rate of imaging may also be related to ED provider consideration of age, although this database does not include information about why a particular study was ordered. These data also do not allow determination of whether imaging was necessary, and in future work it will be useful to examine how age affects the sensitivity and specificity of clinical decision rules for imaging in order to optimize older adult care.
A greater proportion of ED visits by older MVC patients than by younger MVC patients resulted in hospitalization, and there was a trend toward increased odds of admission in older patients after adjustment for other factors. Compared with younger cohorts, older trauma patients have been previously shown to have higher admission rates, longer stays and higher morbidity and mortality,12–14 although this is the first study to describe the patterns of ED care for older MVC patients. We believe it is possible that issues such as co-morbidities, perceived safety of the living situation, limited physiologic reserve, and diagnostic uncertainties in older adults may have influenced the admission decisions for these patients. We were unable to adjust for these factors in the present analysis, an additional investigation into this topic is warranted to better identify the factors that impact the decision by the clinician to admit older adult MVC patients. It is also important to recognize that the majority (85%) of older MVC patients were discharged home, and previous work has suggested that many of these patients may have significant pain.16 Finding ways to optimize pain control (and functional outcomes) while minimizing adverse events, including falls, from narcotic medications will be critical in the coming years.
LIMITATIONS
The NHAMCS database provides reliable, census-weighted estimates of ED use across the U.S., but it does not include some information, such as injury severity score and driver versus passenger status, that may vary by age or may affect admission Other variables, such as imaging, are limited by their classification categories in NHAMCS. We included initial and follow-up MVC-related visits in our study to estimate the total volume of visits. The episode of care was unknown for almost half of MVC-related older (46%) and younger (44%) patients, and there were also no significant differences in the proportions of older and younger MVC patients presenting for initial (53% each) or follow-up (1.7% vs. 2.6%, respectively) visits (p=0.55 under Chi Square). Sampling and non-sampling errors, including coding inaccuracies, misclassification of injuries, and non-response, are also potential limitations to the use of this kind of survey data in research. However, the NHAMCS is a well-established survey tool that uses multiple standardized procedures to minimize these problems, such as pretesting, quality control, and adjustment of weights for non-response items.
A common limitation in survey research is missing data; some variables may not have been assessed by the surveys, and others may have had high proportions of missing or blank responses. In our analysis, data were missing for a high proportion (17%) of the external cause of injury (e-code). It is difficult to determine how the total injury estimates reported for this study would change if these data were available for analysis. It is also possible that the acuity level of the patient impacted those patients with missing or blank responses, which may have affected the findings of this study. Finally, some of the response subgroups had small numbers, limiting our ability to generate reliable estimates for national trends.
CONCLUSION
Although population-based MVC-related ED visit rates for older adults are lower than for younger adults, older MVC victims appear to require significant ED resources in terms of increased use of diagnostic imaging. In addition, a greater proportion of older than younger MVC patients were admitted to the hospital and ICU. As the U.S. population ages and adults continue to drive into old age, EDs will have to allocate appropriate resources and develop diagnostic and treatment protocols to care for the increased volume of older adult MVC victims.
Footnotes
Address for Correspondence: Jody A. Vogel, MD, MSc. Department of Emergency Medicine, Denver Health Health Medical Center, 777 Bannock Street, Mail Code 0108, Denver, CO 80204., Email: jody.vogel@dhha.org. 11 / 2013; 14:576 – 581
Submission history: Revision received March 27, 2012; Submitted October 29, 2012; Accepted February 22, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. United States Census Bureau QuickFacts. Available athttp://quickfacts.census.gov/qfd/states/00000.html. Accessed April 8, 2011.
2. National Transportation and Safety Board, Safety, Mobility, and Aging Drivers Symposium Available at http://www3.ntsb.gov/speeches/hersman/daph101109.html. Accessed April 8, 2011.
3. US Government Accountability Office Available at http://www.gao.gov/new.items/d07413.pdf/. Accessed April 8, 2011.
4. Eberhard J Older drivers’ “high per-mile crash involvement”: The implications for licensing authorities. Traffic Inj Prev. 2008; 9:284-290
5. Spaite DW, Criss EA, Valenzuela TD Geriatric injury: an analysis of prehospital demographics, mechanisms, and patterns. Ann Emerg Med. 1990; 19:1418-1421
6. Scheetz LJ Differences in survival, length of stay, and discharge disposition of older trauma patients admitted to trauma centers and nontrauma center hospitals. J Nurs Schol. 2005; 37:361-366
7. MacKenzie EJ, Morris JA, Smith GS Acute hospital costs of trauma in the United States: Implications for regionalized systems of care. J Trauma. 1990; 30:1096-1101
8. Ten Leading Causes of Death and Injury. . 2012;
9. Platts-Mills TF, Hunold KM, Esserman DA Motor vehicle collision-related emergency department visits by older adults in the United States. Acad Emerg Med. 2012; 19:821-827
10. Scheetz LJ Life-threatening injuries in older adults. AACN Adv Crit Care. 2011; 22:128-139
11. McMahon DJ, Shapiro MB, Kauder DR The injured elderly in the trauma intensive care unit. Surg Clin Nort Am. 2000; 80:1005-1019
12. Finelli FC, Jonsson J, Champion HR A case control study for major trauma in geriatric patients. J Trauma. 1989; 29:541-548
13. Champion HR, Copes WS, Buyer D Major trauma in geriatric patients. Am J Public Health. 1989; 79:1278-1282
14. Tornetta P, Mostafavi H, Riina J Morbidity and mortality in elderly trauma patients. J Trauma. 1999; 46:702-706
15. 2003–2007 microdata file documentation [National Center for Health Statistics Web site]. . ;
16. Metropolitan and Micropolitan Statistical Areas. . ;
17. Recommended framework for presenting injury mortality data. . ;
18. Barell V, Aharonson-Daniel L, Fingerhut LA An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev. 2002; 8:91-96
19. Callaway DW, Wolfe R Geriatric trauma. Emerg Med Clin North Am. 2007; 25:837-860
20. Newgard CD Defining the “older” crash victim: the relationship between age and serious injury in motor vehicle crashes. Accid Anal Prev. 2008; 40:1498-1505
21. Baumann MR, Strout TD Triage of geriatric patients in the emergency department: validity and survival with the emergency severity index. Ann Emerg Med. 2007; 49:234-240


