| Author | Affiliation |
|---|---|
| James F. Holmes, MD, MPH | University of California, Davis, School of Medicine, Sacramento, California |
| Ryan Caltagirone, MD | University of California, Davis, School of Medicine, Sacramento, California |
| Maureen Murphy, RN | University of California, Davis, School of Medicine, Sacramento, California |
| Lisa Abramson, MD | University of California, Davis, School of Medicine, Sacramento, California |
Introduction
Methods
Results
Discussion
Limitations
Conclusion
ABSTRACT
Introduction:
To determine if increased trauma team response results in alterations in resource use in a population of children <6 years, especially in those least injured.
Methods:
We conducted a retrospective before and after study of children <6 years sustaining blunt trauma and meeting defined prehospital criteria. We compared hospitalization rates and missed injuries (injuries identified after discharge from the emergency department/hospital) among patients with and without an upgraded trauma team response. We compared the computed tomography (CT) rate and laboratory testing rate among minimally injured patients (Injury Severity Score [ISS] 6).
Results:
We enrolled 352 patients with 180 (mean age 2.7 ± 1.5 years) in the upgrade cohort and 172 (mean age 2.6 ± 1.5 years) in the no-upgrade cohort. Independent predictors of hospital admission in a regression analysis included: Glasgow Coma Scale <14 (odds ratio [OR]=11.4, 95% confidence interval [CI] 2.3, 56), ISS (OR=1.55, 95% CI 1.33, 1.81), and evaluation by the upgrade trauma team (OR=5.66, 95% CI 3.14, 10.2). In the 275 patients with ISS <6, CT (relative risk=1.34, 95% CI 1.09, 1.64) and laboratory tests (relative risk=1.71, 95% CI 1.39, 2.11) were more likely to be obtained in the upgrade cohort as compared to the no-upgrade cohort. We identified no cases of a missed diagnosis.
Conclusion:
Increasing the trauma team response based upon young age results in increased resource use without altering the rate of missed injuries. In hospitals with emergency department physicians capable of evaluating and treating injured children, increasing ED trauma team resources solely for young age of the patient is not recommended.
INTRODUCTION
Trauma is the leading cause of morbidity and mortality in children age 1 to 18 years.1,2 To care for these injured patients, designated trauma centers provide immediate, specialized treatment. Within these trauma centers, predefined trauma teams respond to the emergency department (ED) to provide such expert care.
The composition of these teams may include surgeons, emergency physicians (EP), anesthesiologists, ED nurses, respiratory therapists, and radiology technicians. In centers with resident training programs, resident physicians frequently compose a substantial membership. The members of these teams, however, vary by hospital, and many centers modify the composition of the trauma team by the severity of the patient’s injuries, known as a tiered response.
Trauma team activation is dependent on the prehospital provider report. The prehospital report is used to determine the extent of the trauma team activation with the most severely injured met in the ED by the entire trauma team and the less severely injured met by a subset of the trauma team. This practice is designed to appropriately match and conserve limited resources and is often referred to as “secondary trauma triage.” “Primary trauma triage” is the initial determination to transport an injured patient to a trauma or non-trauma center.
Criteria for internal trauma team activation and degree of response vary by hospital.3,4 Limited data exist for determining appropriate internal trauma team response.5–12 Due to the limited physiologic reserve and poor response to injury in the elderly, many centers upgrade trauma team response solely for patient age, although this practice is controversial.7,13 Similarly, some centers increase trauma team response solely for young age as the evaluation of these patients may be difficult. However, no data supporting or refuting this practice currently exist.
The study objective was to determine if increased trauma team response results in alterations in resource utilization in this population, especially in those least injured. We hypothesized that an upgraded trauma team response would result in increased resource utilization (hospitalization rates, radiologic and laboratory testing) without decreasing the rate of missed injuries.
METHODS
Study Design
This is a retrospective before-and-after cohort study of children less than 6 years of age with blunt trauma. The study was approved by the study site’s institutional review board.
Study Setting
The study was performed at a single center with both adult Level 1 and pediatric Level 1 trauma center designations. The annual ED census is approximately 65,000 patients/year, including 12,000 children/year. The pediatric ED is staffed at all times by board certified/prepared EPs or pediatric EPs and supports training programs in emergency medicine, pediatrics, and surgery.
Selection of Participants
Eligible patients included those younger than 6 years of age sustaining a blunt trauma mechanism and meeting defined prehospital criteria. This included patients transported by prehospital providers and those arriving by private vehicle. Patients transferred from another facility were excluded. We identified patients from the study site’s trauma registry, which collects data on all patients meeting defined prehospital criteria resulting in trauma team activation. We then searched the pediatric ED patient logs to identify any additional patients with trauma activations who were not included in the trauma registry.
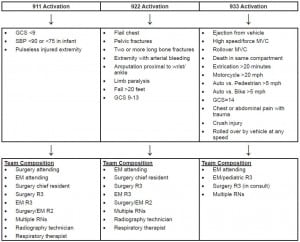
Interventions
The study site has a 3-tiered trauma team response (Figure). Prior to December 2006, patients younger than six years of age were upgraded one level of trauma team response solely because of their age (i.e. patients meeting “933” activation criteria were upgraded to “922” activation response and patients meeting “922” activation criteria were upgraded to “911” activation response). In December 2006, the protocol for trauma team response to the ED was changed such that children younger than 6 years of age did not have the upgraded trauma team response (i.e. patients meeting “933” activation criteria were treated as “933” activations).
We compared patients who had upgraded trauma team response (May to December 2006) with those who did not have upgraded trauma team response (May to December 2007). This time period was chosen to capture the same months, such that the mechanisms of injuries would be similar between 2 groups (avoid bias by including different months and potentially different mechanisms between the 2 cohorts).
The “933” trauma team was composed of the following personnel: emergency medicine (EM) faculty, a second- or third-year pediatric/EM resident, ED nurses, and trauma surgery team consultation by the third-year trauma surgery resident. The third-year trauma surgery resident consultation is mandatory on all “933” patients and occurred at any time prior to patient discharge. This consultation was performed so that the trauma team would be aware of all trauma patients in the ED in case of the need for admission. The “922” trauma team added the following physicians present on patient arrival to the ED: surgery chief resident, third-year surgery resident, second-year surgery/EM resident, and a third-year EM resident. A “911” trauma activation simply added the attending trauma surgeon. Additionally, the “911” and “922” trauma response teams added additional nurses, a respiratory therapist, and a radiology technician, all present in the ED at the time of patient arrival.
Data Collection
Data collection from chart abstraction followed previously published guidelines for conducting retrospective studies.14,15 We standardized data collection with variables of interest defined prior to chart abstraction via investigator meetings. Variables collected included age, mechanism of injury, initial ED Glasgow Coma Scale (GCS) score, initial ED systolic blood pressure (SBP), laboratory testing (including chemistry and hematocrit measurements), abdominal and cranial computed tomographies (CT), Injury Severity Score (ISS), and hospital admission from the ED. GCS and SBP were abstracted from the triage summary/attending EM note (not from the trauma registry). ED data abstraction information was done prior to documenting ISS and hospitalization data. We abstracted ISS data from the radiologic results, procedure notes, and discharge summaries.16,17 The ISS allows stratification of injury severity and is a standard score to identify patients who benefit from trauma center care.18,19 Three investigators (JH, RC, and MM) abstracted all data. Prior to data abstraction, a manual of operations (MOO) was created to define all data points and methods of abstraction. Prior to any abstraction, all investigators met to agree and revise the MOO. After abstraction of 20 cases each, abstractors met to review and finalize the MOO. To minimize any potential abstractor bias, each abstractor abstracted one third of the data from each cohort.
The primary outcome measurements were missed injuries and hospitalization. A missed injury was considered to have occurred if the injury was identified after discharge from the hospital (either discharge from the ED to home or from the hospital to home). An injury not identified in the ED but identified during initial hospitalization was not considered missed by this definition. This was based on return visits to the participating ED or referral to the trauma or ED continuous quality improvement (CQI) committees. Secondary outcome measurements included: 1) CT use, defined as obtaining either a cranial or abdominal CT, and 2) laboratory testing, defined as obtaining a hematocrit level or chemistry measurements.
A random sample of 10% (n=36) of the subjects were abstracted by 2 abstractors to measure inter-rater reliability of the abstractors. Inter-rater reliability was calculated measuring the kappa statistic (weighted kappa for ordinal data).
Data Analysis
We performed data analysis using STATA 11.0 statistical software (STATA Corp, College Station, TX, copyright 2009). Continuous data are presented as the mean ± standard deviation (SD) if normally distributed or median with interquartile range (IQR) if non-normally distributed. Prevalence rates are presented with 95% confidence intervals (CI). We assessed differences in categorical data between the 2 cohorts with chi-square test or Fisher’s exact test (cases of small cell size). We analyzed differences in continuous data with Student’s t-test if normally distributed data. Wilcoxon rank-sum test was used for non-parametric data or ordinal data.
We performed a multivariable logistic regression analysis to identify variables independently associated with hospital admission. We included trauma team upgrade in this analysis to determine if upgrading the trauma team response was associated with hospital admission while including variables to control for degree of injury (mechanism of injury, ISS and GCS).
Finally, we compared minimally injured patients (defined a priori as an ISS less than 6) in the 2 cohorts with regards to the number of CT scans, laboratory tests, and missed diagnosis (injuries identified after discharge from the ED or hospital) and described the risk of obtaining diagnostic testing or missed diagnosis with relative risk (RR) ratios.
RESULTS
We entered 352 patients with a mean age of 2.7 ± 1.5 years into the study. Motor vehicle collisions (183, 52%), falls (83, 24%), and automobile versus pedestrian/bike (58, 16%) were the most common mechanisms of injury. The median ISS was 1 (IQR 1, 5), range 0 – 45. Seventy-five patients (21%) had an ISS greater than 8, and 41 (12%) had an ISS greater than or equal to 16. Excellent reliability between the abstractors existed as kappa values ranged from 0.80 to 0.94.
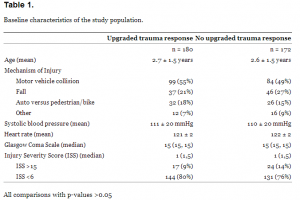
The upgrade trauma team cohort included 180 patients (mean age 2.7 ± 1.5 years), and 172 patients (mean age 2.6 ± 1.5 years) were in the no-upgrade trauma team cohort. Baseline characteristics of those in the upgrade trauma team cohort and those in the no-upgrade trauma team cohort are presented in Table 1. The 2 cohorts appeared similar in age, mechanism of injury, initial SBP, GCS score, and ISS.
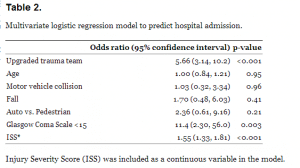
One-hundred twenty-one (67%, 95% CI 60, 74%) patients in the upgrade trauma team cohort and 73 (42%, 95% CI 35, 50%) in the no-upgrade trauma team cohort were admitted. We performed a multivariate analysis to identify variables independently associated with hospital admission. After controlling for head injury with the GCS score and severity of injury with the ISS, the upgrade trauma team cohort was independently associated with hospital admission Table 2.
A total of 275 patients had an ISS less than 6, including 144 (80%) in the upgrade trauma team cohort and 131 (76%) in the no-upgrade trauma team cohort. An increased likelihood of receiving a CT as part of the ED evaluation was identified in those patients in the upgrade trauma team cohort (97/144, 67%, 95% CI 59, 75%) as compared to those in the no-upgrade trauma team cohort (66/131, 50%, 95% CI 42, 59%, Relative risk = 1.34, 95% CI 1.09, 1.64). Similarly, an increased likelihood of receiving laboratory testing occurred in those patients in the upgrade trauma team cohort (111/144, 77%, 95% CI 69, 84%) as compared to those in the no-upgrade trauma team cohort (59/131, 45%, 95% CI 36, 54%, Relative risk = 1.71, 95% CI 1.39, 2.11).
Six patients had return visits to the ED (4 in the upgrade and 2 in the no upgrade cohort). No cases of missed diagnosis were identified in the upgrade cohort (0%, 95% CI 0, 1.7 %) or the no-upgrade cohort (0%, 95% CI % 0. 1.7%). The 6 patients returned for the following: vomiting (2), abdominal pain (1), radiology call back for possible hepatic injury on abdominal CT scan (1), suture removal (1), transient ataxic gate (1). The patient with possible hepatic injury on abdominal CT was initially admitted to the hospital. The faculty radiologist reviewed the initial CT interpretation of normal and considered a possible hepatic injury to be present. The patient was re-evaluated in the ED by both the ED team and pediatric surgery team and felt not to have a definitive hepatic injury and discharged home. This patient was in the upgrade cohort.
DISCUSSION
The study demonstrates that increasing the trauma team response simply due to young age of the injured patient does not result in appreciable clinical benefit. No cases of missed injury from the ED were identified regardless of the trauma team composition. Furthermore, increasing the trauma team resulted in a notable increase in resource use. Rates of hospitalization, CT use, and laboratory testing all increased when the trauma team response was increased, regardless of the degree of patient injury.
We believe the increased resource use is a result of a “framing bias.”20–22 The upgraded trauma team is normally activated for the most-injured patients. Once the team is activated, the members expect to provide care to a severely injured patient and thus evaluate and treat the patient as if he were seriously injured. The team is “anchored”22 to the pre-arrival belief that the patient will be seriously injured, thus an expectation for an aggressive diagnostic work-up and planned hospitalization is made. When this belief is removed (patient does not undergo secondary triage as a severely injured patient), less diagnostic testing and fewer hospitalizations occur as the clinicians’ expectations originate at a different origin.
Evaluating injured children is potentially difficult due to their young age and limited verbal skills.23 Injured children are known to have special needs that must be addressed to provide the best quality of care.24 Recognition of these difficulties has resulted in different evaluation strategies for those who are very young.25,26 Concerns regarding the difficulty in evaluating the youngest children likely generated the impetus to upgrade trauma team response simply due to young age of the injured child.
Surveys demonstrate that significant variation exists among the composition and activation criteria for trauma teams outside of the United States.3,4 Such variation is not known to occur within the U.S. but is highly likely. Variation in pediatric trauma care is a known problem and is considered a cause of decreased quality of care.23,27–29 In the current era of providing quality, cost-effective care, determining appropriate resource use is paramount. Although this study identifies a particular variable (upgrading trauma team response for young age of the patient) that appears to not be effective, further investigation is necessary to determine the most appropriate response for pediatric trauma patients arriving to the ED.
Previous work on “secondary trauma triage” has primarily focused on appropriate indications for trauma team activation in adult patients.5,9,10,12 Despite this work, definitive indications for trauma team activation in adult patients remain unidentified. The data are more confusing in the pediatric population, likely due to the limited data available and the complexity of these patients.
A prior study evaluating 2,311 children from a single trauma registry suggested that activating the surgeon for a pediatric trauma code was of low utility unless the mechanism was penetrating trauma. This decision would significantly decrease the need for a surgeon during the initial ED evaluation as patients without penetrating injury had a low likelihood of needing emergency surgery. This decision instrument, however, has not been validated, and it did not assess for possible improvements in care that may occur with the presence of a surgeon (decreased missed injuries).11 A second study modified the pediatric trauma score and used it to predict trauma team activation.9 This retrospective study identified all seriously injured children (ISS > 10) with the modified pediatric trauma score. The study, however, applied the instrument at the time of patient arrival to the ED and did not assess its use by prehospital providers. As decisions on “secondary trauma triage” are made from prehospital provider reports, the tool requires assessment when implemented using information from the prehospital providers. Finally, a retrospective study of 152 “surgeon-directed trauma team activations” suggests that physiologic variables are sufficient to determine secondary triage.30
These 3 studies highlight the confusion in determining the need for surgeon presence in the ED at the time of patient arrival. Two of these studies considered the trauma surgeon necessary only in instances of emergency surgery,11,30 whereas another considered an ISS cutoff (ISS >10)9 as the outcome of interest. Although improvements in care may be recognized by having a surgeon available for patients who do not require surgery, it is not necessarily a requirement that a surgeon be present at the time of ED arrival for all patients with an ISS >10. In the current era, with EPs and pediatric EPs trained in providing pediatric trauma care, many of these patients can be properly evaluated and initially treated by EPs with selective determinations made about the need for a surgeon. In addition, further triage may be performed at the time of patient arrival (i.e. dismiss the trauma team) if the patient is clearly minimally injured. This process requires future study.
LIMITATIONS
This study was retrospective and therefore subject to the limitations of a medical record review. However, we performed the review following methodologically rigorous guidelines to minimize the potential bias from the review.14,15 In addition, this was a before-and-after study and subject to the bias inherent with such design. We are not aware of temporal changes at the institution that resulted in significant changes in hospitalization or evaluation practices (CT use) during the study period. In addition, recent evidence indicates that despite knowledge of radiation risks associated with CT, its use continues to increase across the entire U.S. and Ontario.31 Furthermore, this study demonstrated ED CT use in children <5 years of age nearly doubled from 2003 to 2008. Thus, if temporal changes biased our study, we would expect CT use to have increased in the later cohort (not decrease as was identified).
The 2 populations appeared similarly injured based on vital signs, age, mechanisms of injury, GCS scores, and ISS. Furthermore, we performed a regression analysis in an attempt to control for possible confounding variables. Finally, the study was conducted at a pediatric Level 1 trauma center with personnel experienced in the care of injured children. The results may not be generalizable to all centers. We did not identify any cases of missed injuries (injuries identified after discharge to home). It is possible that a missed injury was identified at another hospital and the patient was never referred to the study site. At such a low rate (<1%), the sample size required to identify differences between the 2 cohorts would be so large that it would not be feasible to review records to this degree. A multicenter study would facilitate a larger sample size. Although the rate of missed injuries was zero, the current sample size allows for very small confidence intervals around the rate of missed injuries.32 We did not study other potential improvements that may be recognized by increased trauma team response.
We did not conduct a formal cost-effectiveness analysis. However, no clinical benefit was identified with increasing the trauma team response, such that a cost-effectiveness analysis would not be appropriate as it would demonstrate increased costs with no clinical benefit. Finally, due to the retrospective methodology, we were unable to determine any potential harm by additional testing (i.e. unnecessary hospitalization for false positive test results).
CONCLUSION
Increasing the ED trauma team response based upon young age of the patient results in increased resource use without apparent clinical benefit. For locations with EPs capable of evaluating and treating injured children, increasing ED trauma team resources solely for young age of the patient is not recommended.
Footnotes
Address for Correspondence: James F. Holmes, MD, MPH. Department of Emergency Medicine, UC Davis School of Medicine, 2315 Stockton Blvd, PSSB 2100, Sacramento, CA 95817. Email: jfholmes@ucdavis.edu. 11 / 2013; 14:569 – 575
Submission history: Revision received May 16, 2012; Submitted May 24, 2013; Accepted May 29, 2013
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Heron M Deaths: leading causes for 2007. Natl Vital Stat Rep. 2011; 59:1-95
2. Heron M, Hoyert DL, Murphy SL Deaths: final data for 2006. Natl Vital Stat Rep. 2009; 57:1-134
3. Larsen KT, Uleberg O, Skogvoll E Differences in trauma team activation criteria among Norwegian hospitals. Scand J Trauma Resusc Emerg Med. 2010; 18:21
4. Smith J, Caldwell E, Sugrue M Difference in trauma team activation criteria between hospitals within the same region. Emerg Med Australas. 2005; 17:480-487
5. Cherry RA, King TS, Carney DE Trauma team activation and the impact on mortality. J Trauma. 2007; 63:326-330
6. Green SM Is there evidence to support the need for routine surgeon presence on trauma patient arrival?. Ann Emerg Med. 2006; 47:405-411
7. Kohn MA, Hammel JM, Bretz SW Trauma team activation criteria as predictors of patient disposition from the emergency department. Acad Emerg Med. 2004; 11:1-9
8. Shapiro MJ, McCormack JE, Jen J Let the surgeon sleep: trauma team activation for severe hypotension. J Trauma. 2008; 65:1245-1250
9. Simon B, Gabor R, Letourneau P Secondary triage of the injured pediatric patient within the trauma center: support for a selective resource-sparing two-stage system. Pediatr Emerg Care. 2004; 20:5-11
10. Steele R, Gill M, Green SM Do the American College of Surgeons’ “major resuscitation” trauma triage criteria predict emergency operative management?. Ann Emerg Med. 2007; 50:1-6
11. Steele R, Green SM, Gill M Clinical decision rules for secondary trauma triage: predictors of emergency operative management. Ann Emerg Med. 2006; 47:135
12. Tinkoff GH, O’Connor RE Validation of new trauma triage rules for trauma attending response to the emergency department. J Trauma. 2002; 52:1153-1158
13. Demetriades D, Sava J, Alo K Old age as a criterion for trauma team activation. J Trauma. 2001; 51:754-756
14. Gilbert EH, Lowenstein SR, Koziol-McLain J Chart reviews in emergency medicine research: Where are the methods?. Ann Emerg Med. 1996; 27:305-308
15. Worster A, Bledsoe RD, Cleve P Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005; 45:448-451
16. Civil ID, Schwab CW The Abbreviated Injury Scale, 1985 revision: a condensed chart for clinical use. J Trauma. 1988; 28:87-90
17. Copes WS, Champion HR, Sacco WJ The Injury Severity Score revisited. J Trauma. 1988; 28:69-77
18. MacKenzie EJ, Weir S, Rivara FP The value of trauma center care. J Trauma. 2010; 69:1-10
19. Mullins RJ, Veum-Stone J, Helfand M Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994; 271:1919-1924
20. Christensen C, Heckerling PS, Mackesy ME Framing bias among expert and novice physicians. Acad Med. 1991; 66:S76-78
21. Cosby KS A framework for classifying factors that contribute to error in the emergency department. Ann Emerg Med. 2003; 42:815-823
22. Elstein AS Heuristics and biases: selected errors in clinical reasoning. Acad Med. 1999; 74:791-794
23. Dowd MD Effect of emergency department care on outcomes in pediatric trauma: what approaches make a difference in quality of care?. J Trauma. 2007; 63:S136-139
24. . Emergency Care for Children: Growing Pains. 2006;
25. Kuppermann N, Holmes JF, Dayan PS Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009; 374:1160-1170
26. Schutzman SA, Barnes P, Duhaime AC Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics. 2001; 107:983-993
27. Guice KS, Cassidy LD, Oldham KT Traumatic injury and children: a national assessment. J Trauma. 2007; 63:S68-80
28. Ochoa C, Chokshi N, Upperman JS Prior studies comparing outcomes from trauma care at children’s hospitals versus adult hospitals. J Trauma. 2007; 63:S87-91
29. Stylianos S, Egorova N, Guice KS Variation in treatment of pediatric spleen injury at trauma centers versus nontrauma centers: a call for dissemination of American Pediatric Surgical Association benchmarks and guidelines. J Am Coll Surg. 2006; 202:247-251
30. Mukherjee K, Rimer M, McConnell MD Physiologically focused triage criteria improve utilization of pediatric surgeon-directed trauma teams and reduce costs. J Pediatr Surg. 2010; 45:1315-1323
31. Berdahl CT, Vermeulen MJ, Larson DB A tale of two trends: utilization of computed tomography in american and canadian emergency departments. Acad Emerg Med. 2011; 18:S140-150
32. Hanley JA, Lippman-Hand A If nothing goes wrong, is everything all right? Interpreting zero numerators. JAMA. 1983; 249:1743-1745


