| Author | Affiliation |
|---|---|
| Troy E. Madsen, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Anne Bennett, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Steven Groke, BSN | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Anne Zink, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Christy McCowan, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Alex Hernandez, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Stuart Knapp, BS | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Deepthi Byreddy, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Scott Mattsson, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
| Nichole Quick, MD | University of Utah, Division of Emergency Medicine, Salt Lake City, UT |
ABSTRACT
Introduction:
At our 35,000 visit/year emergency department (ED), we studied whether patients presenting to the ED with psychiatric complaints were admitted to the hospital at a higher rate than non-psychiatric patients, and whether these patients had a higher rate of reevaluation in the ED within 30 days following the index visit.
Methods:
We reviewed the electronic records of all ED patients receiving a psychiatric evaluation from January to February 2007 and compared these patients to 300 randomly selected patients presenting during the study period for non-psychiatric complaints. Patients were followed for 30 days, and admission rates and return visits were compared.
Results:
Two hundred thirty-four patients presented to the ED and were evaluated for psychiatric complaints during the study period. Twenty-four point seven percent of psychiatric patients were admitted upon initial presentation versus 20.7% of non-psychiatric patients (p = 0.258). Twenty-one percent of discharged psychiatric patients returned to the ED within 30 days versus 13.4% of discharged non-psychiatric patients (p=0.041). Patients returning to the ED within 30 days had a 17.1% versus 21.6% admission rate for the psychiatric and non-psychiatric groups, respectively (p=0.485).
Conclusion:
Patients presenting to this ED with psychiatric complaints were not admitted at a significantly higher rate than non-psychiatric patients. These psychiatric patients did, however, have a significantly higher return rate to the ED when compared to non-psychiatric patients.
INTRODUCTION
Crowding is a significant problem facing emergency departments (EDs). Multiple factors contribute to this growing healthcare issue. Numerous studies have focused on the idea of “recidivists,” or high frequency ED users who are responsible for a disproportionate number of ED visits.1–7 In one study, 4% of the ED patients accounted for 18% of the total ED visits;8 another study found similar results with 3.5% of ED patients comprising 14.3% of all visits.4 These numbers and the described characteristics of recidivists are consistent even when studied in different healthcare systems in various countries, including France,9 the United States,5 Ireland,10 Canada,11 Sweden12 and the United Kingdom.13
Several studies focusing on the characteristics of recidivists make it clear that the prevalence of psychiatric illness is very high in this population.9,14,16 One study, comparing 100 frequent attendees with 100 control patients, found that 11% of the study group presented with psychological problems compared to 1% of patients in the control group and reported alcohol or drug use in 38% of the frequent attendees compared to 6% of the control group.15 Consensus in the literature agrees on the following description of recidivists: men from poor socioeconomic background with marked psychosocial problems and/or complex medical problems. Furthermore, recidivists have a higher than expected mortality and morbidity.16–18 Such information only heightens the urgency to identify and appropriately intervene on behalf of psychiatric recidivists. Such measures may be life-saving and will certainly, though less importantly, be cost-saving.
In this study we focus on a specific group of ED users namely patients who suffer from psychiatric illnesses, who are at increased risk to become recidivists, when compared to the baseline population. Suicidality and other psychiatric complaints are especially prone to recidivism.19,20,21 We addressed this issue of recidivism by comparing the 30-day return rate between patients presenting with a psychiatric complaint and those presenting with all other complaints of a non-psychiatric nature. We hypothesized that psychiatric patients returned to the ED at higher rates than non-psychiatric control patients, but were not admitted to an inpatient unit at a higher rate than these controls.
METHODS
This study was conducted at the University of Utah Medical Center Emergency Department, the primary medical facility of the University of Utah Neuropsychiatric Institute and a unique research environment due to its expansive geographical catchment area, which includes Utah, Nevada, Wyoming, Idaho and western Colorado. The ED evaluates over 35,000 patients per year, and serves as the primary screening site for admission to the region’s largest psychiatric facility, which has 90 inpatient beds and approximately 3,000 inpatient admissions per year. The study was a retrospective chart review using the University of Utah Medical Center electronic medical record database, and was approved by the Institutional Review Board at the University of Utah on January 29, 2008.
The study group was comprised of all patients who presented between January and February 2007 with a psychiatric complaint for which an evaluation by a licensed clinical social worker (LCSW) was requested by an attending emergency physician (EP). The historical control population consisted of 300 randomly selected patients who presented to the ED with a non-psychiatric complaint during the months of January and February 2007. This number of control patients was selected based on power calculation to detect a 30% difference in admission rates and return visits between groups, assuming 80% power and alpha of 0.05. Historical controls were selected from the ED patient log beginning January 1, which was the first day of the study period, and were selected from across the study period using a random number generator. Those who were evaluated by a LCSW at any point during their stay were excluded from the control population. Psychiatric admission was defined as admission to an inpatient psychiatric unit. Medical students using a template form performed chart reviews. Investigators entered data into a standardized database. Twenty percent of the study charts were reviewed by one of the study’s primary investigators.
A significant source of information about the study population came from notes written by LCSWs. To more thoroughly evaluate psychiatric patients presenting to the ED, LCSWs complete a crisis note detailing their assessment and recommendations for admission versus discharge following the initial evaluation by an EP. Reason for evaluation by a LCSW included suicidal ideation, suicide attempt, psychosis, substance abuse, or any other psychiatric complaint for which the attending EP requested an evaluation. Detailed crisis notes follow a template format and include patient age, gender, presentation, history of suicide attempts, psychiatric history, living situation, and current sources of stress in the patient’s life. All patient-disposition decisions (admission vs. discharge) are made by the LCSW in discussion with the attending EP. LCSWs in the ED follow up on discharged patients through hospital records and community psychiatric facility records.
The control group consisted of patients who presented to the ED with a complaint of a non-psychiatric nature in the time period concurrent with the study group. These complaints represented the full spectrum of potential ED visits including trauma, abdominal pain, chest pain, infection, etc. Patients were excluded from the control group if they had been evaluated by a LCSW for any reason during their stay, as the study group consisted of patients who had received an LCSW evaluation. These patients were found in the electronic database and selected randomly from the months of January through February 2007. We followed all patients included in the study for 30 days for return ED visit and hospitalization upon return visit. In the case of patients with multiple ED visits during the study period, the initial visit during this period was defined as the index visit, and additional visits were defined as repeat visits.
The admission rate, rate of return to ED within 30 days, and admission rate on return visits were compared for the two study groups. We performed statistical analysis using chi-square and Student’s t-test with p<0.05 considered statistically significant (SPSS v. 16.0).
RESULTS
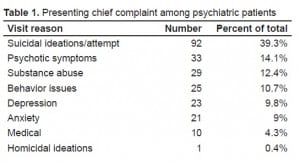
Two hundred thirty-four patients presented to the ED during the study period with a chief complaint of a psychiatric nature and were evaluated by a LCSW. Of these, 92 patients expressed suicidal ideation or confirmed having recently attempted suicide while 142 presented with non-suicidal psychiatric complaints. The most common non-suicidal psychiatric complaints were psychotic symptoms, substance abuse, behavioral issues, anxiety, and depression (Table 1).
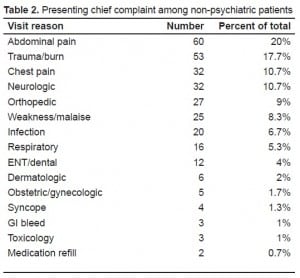
As a comparison group, we selected 300 medical and trauma patients without psychiatric complaints who also presented during this same period. The most common visit reasons among the control group included abdominal pain, orthopedic complaints, trauma, neurologic symptoms, weakness/malaise, and chest pain (Table 2).
Psychiatric patient admission rates at the initial ED visit were higher than that of controls, but this was not statistically significant. Twenty-four point seven percent (58/234) of psychiatric patients were admitted upon initial presentation to the ED compared to 20.7% (62/300) of non-psychiatric patients (p = 0.258) (Figure 1).

The 30-day ED return visit rate for psychiatric patients who were discharged from the ED was significantly higher than that of the control group who were discharged: 21% (37/176) of psychiatric patients returned vs. 13.4% (32/238) of non-psychiatric patients (p=0.041). Among patients who were admitted to the hospital on initial ED visit, 7% (4/58) of psychiatric vs. 8% (5/62) of non-psychiatric patients returned to the ED within 30 days. Upon return ED visit, 17.1% (7/41) of psychiatric patients and 21.6% (8/37) of non-psychiatric patients were admitted to the hospital (Figure 1).
Overall, admitted psychiatric patients were less likely to return to the ED within 30 days of their index visit; 21% of discharged psychiatric patients vs. 6.9% of admitted psychiatric patients returned (p=0.014). There was not a significant difference in 30-day return rates between male (18.8%, 22/117) and female (16.2%, 19/117) psychiatric patients (p=0.606).
Among psychiatric patients, we compared return ED visits between those complaining of suicidal ideations and those with other psychiatric complaints. Thirty-one point five percent (29/92) of suicidal patients vs. 20.4% (29/142) of non-suicidal patients were admitted at the time of the initial ED visit (p=0.055). Discharged suicidal patients were not more likely to return within 30 days (17.5% of suicidal vs. 23% of non-suicidal, p=0.386) nor to be admitted upon return ED visit (8.3% of suicidal vs. 20.7% of non-suicidal, p=0.339). There were no completed suicides during the study period.
As the LCSW evaluations included patients with substance abuse, we also compared return ED visits between patients who were evaluated for substance abuse to those with other psychiatric complaints. Seventeen point two percent (5/29) of those primarily evaluated with substance abuse were admitted to the hospital at the index ED visit vs. 25.9% of those with other psychiatric complaints (p=0.315). Return ED visit rates were nearly identical between groups: 17.2% (5/29) of substance abuse patients vs. 17.6% (36/205) of other psychiatric patients returned to the ED within 30 days (p=0.966).
DISCUSSION
Individuals presenting to EDs with psychiatric complaints represent a patient population for which recidivism is a common occurrence. Reasons for revisits are multi-factorial; however, because many patients face decreasing access to both inpatient and outpatient psychiatric services, the ED has become their sole safety net for obtaining needed care.
High recidivism in this population may be one of several factors that contribute to the growing problem of ED overcrowding. Recidivists may be judged by ED staff to have non-urgent concerns and given a lower priority, setting them up to have a serious problem overlooked.8 The increased use of medical care does not correlate with increased quality of care. Conflicting counsel and medications pose a threat to any frequent ED user.
High frequency ED users use other sources of medical care at a higher rate than the general population.15,8 While our data does not directly deal with this issue, it reinforces the necessity of finding care that works for this population. The literature on this topic provides one such explanation for recidivists – simply that recidivists are a medically and psychosocially vulnerable group.1,5,16,18,26–28 Therefore, recidivists not only need more care but actually seek more care, suggesting that simply transferring care from the ED to primary care may not be the solution. Some continue this line of reasoning, stating that with increased severity of medical conditions, the ED may be a more appropriate place for recidivists than primary care facilities.5,29
When our data are evaluated within the sub-population of psychiatric recidivists, the issue becomes the high risk that this population presents to themselves. In this study we determined that psychiatric patients return to the ED at a significantly higher rate than those patients with a non-psychiatric complaint. Past studies have highlighted the urgency of this problem by connecting excess mortality rates with recidivism.30–33 In a five-year follow-up study by Ostamo et al.,33completed suicide was the cause of excess mortality in 37% of female deaths and 44% of male deaths among suicidal emergency patients. The risk of completed suicide is particularly high during the first year following an attempt,33–35 suggesting that immediate repeat visits must be handled with a heightened sense of caution and attention to the accuracy of assessment. Further analysis is needed to better characterize patients who return to the ED, require admission on repeat visit, or continue to demonstrate self-harm behavior upon discharge.
LIMITATIONS
Limitations of this study are those common among all studies with a retrospective chart review design. The accuracy of the records may have been compromised by the author of the records, the interpretation of the reader or any of the intervening steps. The assessment of repeat visits was determined by the availability of LCSW notes or ED physician notes rather than a hospital consensus database that may be more accurate. A limitation of this study is that the diagnosis of mental disorders was made by the clinical judgment of the attending EP rather than by the utilization of a standardized diagnostic tool.
Additionally, we included patients only from the months of January and February, 2007. This presents the potential for bias, as certain medical conditions may be more or less likely during this period, and seasonal condition may create the potential for variations in return visit rates. Lastly, because this is a single-institution study and the results may not be applicable or generalizable to other institutions. Our hospital serves as a regional referral center, which may skew the results due to the complexity of patients. We felt, however, that this would be at least partially counterbalanced by the medical control group, as our facility serves as a referral center for all medical complaints.
CONCLUSION
Psychiatric patients are especially prone to recidivism. In our study, this population was significantly more likely than medical controls to return to the ED within 30 days. Their recidivism makes this population amenable to preventive measures, while its severity highlights the critical need for prevention. Appropriately identifying patients for discharge versus inpatient treatment may both ease the burden on EDs as short-term repeat visits are prevented and more importantly, prevent the tragic outcomes of completed self-harm behaviors and continued suffering in this population.
Additional research is needed to identify those psychiatric patients best suited for admission versus discharge. Future research may also focus on alternatives to the ED that are available to psychiatric patients in need of care. Lastly, defining the role and interplay of roles among primary care physicians, psychiatrics, and EDs in the care of psychiatric patients may highlight potential solutions to the problem of psychiatric recidivists.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted November 6, 2008; Revision Received February 16, 2009; Accepted March 22, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Troy Madsen, MD, Division of Emergency Medicine, University of Utah, 30 N. 1900 E. 1C26, Salt Lake City, UT 84132
Email: troy.madsen@hsc.utah.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Malone RE. Heavy users of emergency services: social interaction of a policy problem. Soc Sci Med. 1995;40:469–77. [PubMed]
2. Ullman R, Block JA, Stratmann WC. An emergency room’s patients: their characteristics and utilization of hospital services. Med Care. 1975;13:1011–20. [PubMed]
3. Schneider KC, Dove HG. High Users of VA emergency room facilities: are outpatients abusing the system or is the system abusing them? Inquiry. 1983;20:57–64. [PubMed]
4. Huang JA, Tsai WC, Chen YC, et al. Factors associated with frequent use of emergency services in a medical center. J Formos Med Assoc. 2003;102:222–8. [PubMed]
5. Lucas RH, Sanford SM. An analysis of frequent users of emergency care at an urban university hospital. Ann Emerg Med. 1998;32:563–8. [PubMed]
6. Okuyemi KS, Frey B. Describing and predicting frequent users of an emergency department. J Assoc Acad Minor Phys. 2001;12:119–23. [PubMed]
7. Olsson M, Hansagi H. Repeated use of the emergency department: qualitative study of the patient’s perspective. Emerg Med J. 2001;18:430–4. [PMC free article] [PubMed]
8. Hansagi H, Olsson M, Sjöberg S, et al. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001;37:561–7. [PubMed]
9. Lang T, Davido A, Diakité B, et al. Using the hospital emergency department as a regular source of care. Eur J Epidemiol. 1997;13:223–8. [PubMed]
10. Murphy AW, Leonard C, Plunkett PK, et al. Characteristics of attenders and their attendances at an urban accident and emergency department over a one year period. J Accid Emerg Med.1999;16:425–7. [PMC free article] [PubMed]
11. Brown EM, Goel V. Factors related to emergency department use: results from the Ontario Health Survey 1990. Ann Emerg Med. 1994;24:1083–91. [PubMed]
12. Hansagi H, Edhag O, Allebeck P. High consumers of health care in emergency units: how to improve their quality of care. Qual Assur Health Care. 1991;3:51–62. [PubMed]
13. Foroughi D, Chadwick L. Accident and emergency abusers. Practitioner. 1989;233:657–9.[PubMed]
14. Andrén KG, Rosenqvist U. Heavy users of an emergency department: psycho-social and medical characteristics, other health care contacts and the effect of a hospital social worker intervention. Soc Sci Med. 1985;21:761–70. [PubMed]
15. Byrne M, Murphy AW, Plunkett PK, et al. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med.2003;41:309–18. [PubMed]
16. Hangsagi H, Allenbeck P, Edhag O, et al. Frequency of emergency department attendances as a predictor of mortality: nine-year follow-up of population-based cohort. J Public Health Med.1990;12:39–44. [PubMed]
17. Hayward RA, Bernard AM, Freeman HE, et al. Regular sources of ambulatory care and access to health services. Am J Public Health. 1991;81:434–8. [PMC free article] [PubMed]
18. Genell Andrén K, Rosenqvist U. Heavy users of an emergency department–a two year follow-up study. Soc Sci Med. 1987;25:825–31. [PubMed]
19. Tejedor MC, Díaz A, Castillón JJ, et al. Attempted suicide: repetition and survival–findings of a follow-up study. Acta Psychiatr Scand. 1999;100:205–11. [PubMed]
20. Hall DJ, O’Brien F, Stark C, et al. Thirteen-year follow-up of deliberate self-harm, using linked data. Br J Psychiatry. 1998;172:239–42. [PubMed]
21. US Public Health Service National strategy for suicide prevention: goals and objectives for action.Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2001.
22. McMillan JR, Younger MS, DeWine LC. Satisfaction with hospital emergency department as a function of patient triage. Health Care Manage Rev. 1986;11(3):21–7. [PubMed]
23. Hansagi H, Carlsson B, Brismar B. The urgency of care need and patient satisfaction at a hospital emergency department. Health Care Manage Rev. 1992;17:71–5. [PubMed]
24. Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health. 1993;83:372–8. [PMC free article] [PubMed]
25. Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician. JAMA. 1991;266:1085–90. [PubMed]
26. McCusker J, Healey E, Bellevance F, et al. Predictors of repeat emergency department visits by elders. Acad Emerg Med. 1997;4:581–8. [PubMed]
27. Purdie RFJ, Honigman B, Rosen P. The chronic emergency department patient. Ann Emerg Med.1981;10:298–301. [PubMed]
28. Rask KJ, Williams MV, McNagny SE, et al. Ambulatory health care use by patients in a public hospital emergency department. J Gen Intern Med. 1998;13:614–20. [PMC free article] [PubMed]
29. Lowe RA, Bindman AB. Judging who needs emergency department care: a prerequisite for policy-making. Am J Emerg Med. 1997;15:133–6. [PubMed]
30. Nielsen B, Wang AG, Brille-Brahe U. Attempted suicide in Denmark. IV. A five-year follow-up.Acta Psychiatr Scand. 1990;81:250–4. [PubMed]
31. Suokas J, Suominen K, Isometsa E, et al. Long-term risk factors for suicide mortality after attempted suicide–findings of a 14 year follow-up study. Acta Psychiatr Scand. 2001;104:117–21.[PubMed]
32. Nordström P, Asberg M, Aberg-Wistedt A, et al. Attempted suicide predicts suicide risk in mood disorders. Acta Psychiatr Scand. 1995;92:345–50. [PubMed]
33. Ostamo A, Lönnqvist J. Excess mortality of suicide attempters. Soc Psychiatry Psychiatr Epidemiol. 2001;36:29–35. [PubMed]
34. Nordström P, Samuelsson M, Asberg M. Survival analysis of suicide risk after attempted suicide.Acta Psychiatr Scand. 1995;91:336–40. [PubMed]
35. Isometsa ET, Lonnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry.1998;173:531–5. [PubMed]


