| Author | Affiliation |
|---|---|
| Casey A. Grover | David Geffen School of Medicine at University of California, Los Angeles |
| Reb JH Close, MD | Community Hospital of the Monterey Peninsula, Department of Emergency Medicine, Monterey, CA |
| Kathy Villarreal, RN | Community Hospital of the Monterey Peninsula, Department of Emergency Medicine, Monterey, CA |
| Lee M. Goldman, MD | Community Hospital of the Monterey Peninsula, Department of Emergency Medicine, Monterey, CA |
ABSTRACT
Introduction:
Emergency department (ED) frequent users account for a large number of annual ED visits and often receive radiological studies as a part of their evaluation. We report a pilot study of a case management program for ED frequent users to reduce ED usage and radiation exposure.
Methods:
This observational retrospective study was performed at a community hospital ED. Between May 2006 and April 2008, 96 patients were enrolled in a case management program and were followed through November 2008. The case management program consisted of a multi-disciplinary team of physicians, nurses, social services and specialists in pain management and behavioral health. Patients were enrolled if they had five or more visits to the ED in the previous month, if a concern about a patient’s ED use was raised by staff, or if they were identified by the California prescription monitoring program. Case management addressed specific patient issues and assisted with receiving consistent outpatient care. The number of ED visits per patient and the number of radiological studies at each of these visits was recorded. When reviewing data for analysis, we used the number of total images in all computed tomography (CT) scans during the given time period.
Results:
In the six months prior to enrollment, patients averaged 2.3 ED visits per patient per month. In the six months after enrollment, patients averaged 0.6 ED visits per patient per month (P<0.0001), and all visits after enrollment up to November 2008 averaged 0.4 visits per patient per month (P<0.0001). In the six months prior to enrollment, these patients averaged 25.6 CT images per patient per month. In the six months after enrollment, patients averaged 10.2 CT images per patient per month (P=0.001), and all CT images after enrollment up to November 2008 averaged 8.1 CT images per patient per month (P=0.0001). This represents a decrease in ED use by 83% and a decrease in radiation exposure by 67%.
Conclusion:
Case management can significantly reduce ED use by frequent users, and can also decrease radiation exposure from diagnostic imaging.
INTRODUCTION
With emergency department (ED) use always on the rise and waiting room times ever increasing, management of ED frequent users is becoming a very important issue. Recent literature has defined frequent use as four or more ED visits per year, 1–3 These patients tend to have more psychiatric problems, substance abuse issues, chronic medical conditions, and psychosocial stressors than other ED patients.1–16 Given the resources needed to manage these patients, several methods have been evaluated to decrease their use. Intensive case management and the use of narcotics protocols have been shown to significantly decrease use, 11–12, 17–21 while other efforts have been ineffective in keeping frequent users out of the ED.22–23
Radiation exposure from diagnostic imaging is another issue that emergency physicians (EP) must consider when pursuing a diagnosis. EPs rely increasingly on computed tomography (CT) scans as they provide a rapid way to confirm a diagnosis, prevent misdiagnosis, and pick up incidental pathology that would otherwise be missed.24–28 However, there can be significant radiation exposure from even a single CT scan. An abdominal CT provides on average an effective dose of 10 mSv, which is associated with a 0.05% risk of cancer. For patients receiving more than one CT in a single visit or multiple CT scans over time, the risk of cancer increases significantly.29–32
Although the threshold for frequent use has previously been defined as only four visits per year,1–3many patients seek emergency care significantly more than this. Several studies have identified large groups of patients who use ED services on average 20 times or more per month.15, 22, 34 These patients consume large amounts of healthcare resources and worsen ED crowding.12 Additionally, given how often these patients seek care and the major role that CT plays in patient evaluation in the ED, frequent users may be at an increased risk of radiation exposure by choosing to seek ED care.
Malignancy secondary to radiation exposure from CT scans is an issue that has received attention from both medical and patient audiences. Both patients and providers alike often choose not to use CT scans in ED diagnostic evaluations, citing the risk of malignancy. With this in mind, we chose to examine radiation exposure from CT scans as part of our investigation.
The purpose of this study was to evaluate a pilot program consisting of intensive case-management for frequent users at a community hospital to determine if case management is an effective means of decreasing both frequency of ED use and radiation exposure in frequent users.
METHODS
This observational retrospective study was performed at a 205-bed community hospital in central California with approximately 45,000 visits to the ED each year. This study was granted IRB exemption by the hospital committee on research.
A case management pilot program was developed by the ED staff to adequately meet the needs and improve the overall care of patients recurrently seeking care in the ED for chronic medical problems, including narcotic or benzodiazepine addiction. The program is chaired and operated by an ED nurse, who oversees a committee consisting of ED physicians, a chemical dependency physician, hospitalist physicians, pain management clinicians, behavioral health physicians and nurses, as well as social service providers. Patients were enrolled in the case management program if they were identified as having five or more visits to the ED in the month prior to enrollment. Patients could also be enrolled if nursing staff or physicians requested a case management evaluation for a particular patient based on patient pattern uses. Additionally, patients could be enrolled if one of the ED physicians received a letter from the California prescription monitoring program regarding a patient. The case management team met once a month for 90 minutes to discuss both patients currently being managed and patients newly identified as needing case management.
When a patient was first presented to the case management team, the chair provided a tally of his or her recent ED visits, with a listing for each of the visits of the chief complaint, studies performed, ED treatments provided, and prescriptions given. Also included were a record of the patient’s admissions from the ED and medical problems including regular medications. Based on this information, the case management team determined the chronic problem or problems underlying the frequent use of the ED and then developed a plan to manage these problems in the outpatient setting. Patient care plans consisted of referral to outpatient resources for the management of patients’ chronic problems outside of the ED. Such resources included chemical dependency treatment for addiction, pain management for chronic pain, psychiatric services for untreated anxiety or depression, and primary care for those without a primary care provider. Patients without insurance could also be referred to social services for assistance in getting Medi-cal/Medicaid insurance. Additionally, to prevent repeat use for the same chronic problems, the team created recommendations regarding what treatments could be given in the ED. For example, the team recommended that patients with chronic pain not receive narcotics for their chronic pain; rather, the patient’s primary care physician (PMD) or pain management physician would be contacted. Similarly, recommendations for patients with opiate or benzodiazepine addiction often involved not using opiates or benzodiazepines except in case of new and acute issues, such as trauma. Patients received letters at their listed mailing addresses informing them of their enrollment in the case management program and the specifics of their plan.
For patients already enrolled in the program, the case management team periodically reviewed all of the patient’s visits to the ED, including those since enrollment. In the case of a significant reduction in the frequency of ED use and adherence by the ED staff to the case management plan, the patient’s plan would be continued and reassessed at a later meeting. For patients with minimal decreases in ED use, the case management team reassessed the patient’s problems to develop a new plan to implement.
Once patients were enrolled, documents regarding their case management plan were placed into the patient’s medical record, allowing EPs and other physicians treating the patient to have easy access to the care plan. Furthermore, to improve adherence to the plan, patients in case management were identified upon arrival to the ED and a note was placed on the ED status board in the comments section to alert treating physicians and nursing staff of the patient’s enrollment in the case management program.
In analyzing data for our study, we used the hospital’s medical record system to obtain data regarding the frequency of patients’ visits, chief complaints at each visit, nature of their care plan, basic demographic information about each patient, referrals attended, and the number of CT scans received. We recorded the total number of CT scan images at each visit to compare radiation exposure from CT scans before and after program enrollment.
Our study had two primary outcome measures. The first was the number of visits per patient per month to the ED, and the second was the number of CT scans per patient per month. We recorded the number of patient visits per month and number of CT scans received per month for the six months prior to enrollment in the program and the six months after enrollment. To assess the efficacy of the case management over a longer time period, all enrolled patients were followed through November 2008, when our study data collection ended. Patient visits per month and the number of CT scans per month were recorded for this time period.
Our study also had three secondary outcome measures. We compared admission rates before and after enrollment in the program as a method of discerning if the case management program was preventing people from seeking care when needing admission. We also evaluated the rate of attendance of our major referrals for the program to determine if patients were receiving the care recommended to them. Of the patients who were referred to obtain insurance, obtained a PMD, received care from the pain management service, received a chemical dependency evaluation, or received an evaluation and care from the psychiatry service, we examined the percentage of our patients successfully receiving these services. Finally, for each patient we determined the most common chief complaints that brought them to the ED for care both before and after enrollment as a means of assessing whether or not the patient’s chronic problems were being adequately addressed. In case a patient presented frequently for two separate issues, both of these were recorded as their most common chief complaint.
We analyzed data with Microsoft Excel 2007, using a paired, two-tailed t-test to generate p values in comparing ED visits per patient per month and CT images per patient per month in the six months prior to enrollment to both the six months after enrollment as well as to the time period from enrollment through November 2008.
RESULTS
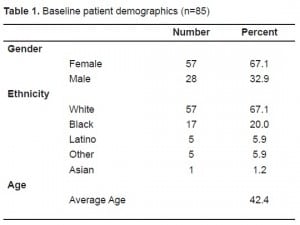
Between May 2006 and April 2008, 96 patients were enrolled in the case management program, and all were followed through November 2008. Eighty-nine patients were enrolled because of the frequency of their visits or staff concerns, and seven were enrolled after notification by the California prescription monitoring program. Of these 96 patients, four had plans that, for unclear reasons, were consistently not followed by ED staff, five had plans that did not address the patient’s underlying problem, and two had medical records could not be found. These three groups were excluded from data analysis; thus, we included 85 patients in the case management program in the analysis. Baseline patient demographics of the 85 patients enrolled can be found in Table 1. Only one of the 85 patients (1.2%) included in the analysis died after enrollment.
In the six months prior to enrollment in the program, patients averaged 2.3 ED visits per patient per month. In the six months after enrollment, patients averaged 0.6 ED visits per patient per month (P<0.0001), and all visits to the ED after enrollment up to November 2008 averaged 0.4 visits per patient per month (P<0.0001).
In the six months prior to enrollment in the case management program, these patients averaged 25.6 CT studies per patient per month. In the six months after enrollment, these patients averaged 10.2 CT studies per patient per month (P=0.001), and all CT studies after enrollment up to November 2008 averaged 8.1 CT scans per patient per month (P=0.0001).
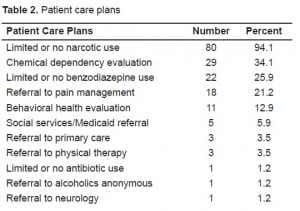
The specific interventions of the patient care plans as a part of the case management program are outlined in Table 2. The admission rate, measured as admissions per ED visits, during the six months prior to enrollment in the program was 11%. In the six months after admission, the admission rate was 8.5% (P=0.43), while the admission rate for all visits after enrollment through November 2008 was 7.9% (P=0.19).
As far as the efficacy of our referrals, the primary physician status and insurance status for all patients before and after enrollment in the program is outlined in Table 3. Notably, of the three patients who did not have a PMD prior to enrollment and were referred to get one, all three (100%) received a PMD. Additionally, of the five patients that did not have insurance prior to enrollment and were referred to social services to obtain insurance, four of these patients (80.0%) received Medi-Cal/Medicaid after enrollment. Of the 29 patients who were referred to the chemical dependency service, three (10.3%) attended their referral. Of the 18 patients sent to the pain management service, six (33.3%) attended their referral. Finally, of the 11 patients referred to psychiatry, five (45.4%) attended the referral given to them. Of the 66 referrals given for these five services, only 21 referrals were successfully attended (31.8%).

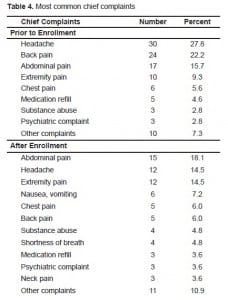
Finally, the most common chief complaints for ED visits both before and after enrollment are outlined in Table 4. The most common chief complaint was the same prior to and after enrollment in 31 of the 85 enrolled patients (36.5%).
DISCUSSION
Prior to discussing the results of our intensive case management program, it is important to point out that much of the previous literature on frequent users of ED services focuses on those patients that are homeless.10–12,15,21 Of the patient population in our case management program, only one of the 85 patients (1.2%) was homeless. Thus, our study likely represents a much different group of patients than previously studied.
Frequency of use
Literature on frequent users has demonstrated numerous reasons as to why patients choose to repeatedly seek care in the ED. Patients have reported that they prefer ED care because they anticipate that their regular physician will not be able to take care of them, the ED is easy to get to, and emergency services are conveniently available 24 hours per day.35–36 Chronic pain and the desire for narcotics and other psychoactive drugs are two additional, common reasons why patients may choose to frequent the ED, with some estimates of drug-seeking patients accounting for as high as one-fourth of ED visits.8–9,15–16,18,37 Furthermore, one prior study of case management for frequent users found that approximately two-thirds of ED frequent users required interventions involving restriction of narcotics prescriptions.22 With 94% of the patients in our case management program requiring interventions involving restriction or limitation of narcotics, chronic pain and chemical, dependency must be regarded as important issues in frequent users. The restriction of narcotics in frequent users, both in our data as well as in other studies, markedly decreased ED usage.18, 22
Nearly 90% of patients in our program had a PMD prior to enrollment in case management, and nearly 90% had health insurance prior to enrollment. These figures strongly suggest that lack of access to care was not an underlying reason for repeated ED usage in our group of patients, but rather patients were either not being adequately treated for their chronic medical conditions by their regular physicians or were choosing to seek ED care in an attempt to obtain prescription medications for underlying substance abuse problems.
Regardless of why patients choose to come to the ED for care, crowding is an increasingly common problem that is only made worse by frequent users.12,38 Case management has been previously documented as an effective means of reducing ED use by frequent users,11–12,17–21 which we also found to be the case with our case management program. Between May 2006 and April 2008, the frequent users who eventually enrolled in the program averaged 2.3 visits per patient per month, which accounted for 1,173 visits in the six months prior to their enrollment. Should this have continued without intervention, this group of 85 patients would have accounted for 2,346 visits per year, which would make up approximately 5% of all visits to our ED. After enrollment in the program, these patients averaged 0.6 visits per patient per month for the first six months, which accounted for only 290 visits in the six months after their enrollment, a decrease in the number of visits by 75%. Following the patients for longer than the six months after their enrollment demonstrated that these patients only averaged 0.4 visits per patient per month, or just 398 visits per year. Thus, our case management program has decreased the number of visits by frequent users by 83%, and has saved the department 1,948 visits per year. As mentioned above, one of the limitations of the study was that patients were not always identified as being in case management upon arrival to the ED. With changes in patient tracking and recognition, we may be able to ensure that patient plans are followed more closely. Thus, further reductions in use beyond what we have already accomplished may be possible.
Frequent users are known to have conflicts with staff, tend to be heavy users of healthcare resources, and are often dissatisfied with their healthcare.1,2,4 Given that frequent users tend to have more psychological, substance abuse, and chronic medical issues than other ED patients,1–16 it becomes clear that their evaluation and treatment is time-consuming. It is difficult to estimate how much time and effort was saved by eliminating these visits, but it may well represent more time saved than elimination of visits by other ED patients.
One final point to consider on the topic of the frequency of ED use by the patients in our program is the cost associated with their care. Although we did not perform a formal financial analysis of our program, we can estimate the effect of our program on healthcare costs with reasonable accuracy. The average ED visit bills approximately $1,000.15 Considering that our program decreased visits by about 2,000 visits per year, this likely represents nearly two million dollars annual savings to patients and insurance companies. Because many of our patients have Medicare or Medicaid/Medi-Cal insurance, this represents significant savings to overburdened government insurance plans. This finding is supported by additional research showing that case management programs effectively reduce costs associated with care of frequent users.12,21 Furthermore, nearly 60% of the patients in our program had Medicare or Medicaid/Medi-Cal insurance. With declining reimbursements for ED visits by these two plans,14 a significant decrease in the number of visits per year by patients with Medicare or Medicaid/Medi-Cal insurance may also represent a reduction in the number of non-profitable visits for the department. For EDs that serve a large population of homeless and/or uninsured patients, such a reduction in use by these patients would markedly reduce the number of uncompensated visits as well.
Efficacy of the program in meeting patient needs
Although we did not have any direct means of assessing patient satisfaction with the program, we recorded several data points for each patient that gives us a more thorough understanding of our case management program efficacy. First, in examining the patients’ most common chief complaints, only 31 out of 85 patients (36.5%) had the same common chief complaint before and after admission in the program. We interpret this to mean that the underlying chronic problem was managed well enough in 63.5% of patients that they were less inclined to seek recurrent ED treatment. An alternative explanation is that patients with narcotic addiction issues, once informed that they would no longer receive narcotics except in the case of acute medical illness, chose to change their chief complaint in an attempt to bypass any restrictions placed on them so as to receive narcotics.
A second measure of success of our case management program is the efficacy of our referrals. The overall attendance rate of our five major referrals (PMD, insurance, chemical dependency, pain management, and psychiatry) was 31.8%. An initial look at this number may suggest that our program was ineffective in treating our patients. Previous evidence has shown that frequent users are notoriously poor at keeping appointments, and the low success rate of our referrals supports this claim.16, 21 However, individual examination of each of the referrals reveals an interesting trend. The two referrals with the highest success rate were to obtain a primary physician and insurance, at 100% and 80.0%, respectively. These are services that patients may view as important and are thus more motivated to attend. Our referrals to psychiatry had an intermediate success rate of 45.4%. Furthermore, one referred patient died of cardiopulmonary disease shortly after his referral to psychiatry, so our success rate may actually be as high as 50.0%. Our interpretation of this intermediate success rate is that our patients with psychiatric needs often have limited insight into their problem, and it is likely that only patients with adequate insight and judgment actually attended their appointments. Finally, our success rate of referrals to pain management and chemical dependency were very low, at 33.3% and 10.3%, respectively. We feel that these low success rates are the direct result of the large number of patients in our program having narcotic addiction problems. Rather than wanting treatment for their addiction or receiving opiate narcotics on a set schedule by a pain management physician, we believe that these patients were only interested in obtaining more narcotics. Our experience is that only a small number of our narcotic addiction patients have the motivation and insight to seek treatment and improve their condition.
Radiation exposure
Risks associated with diagnostic imaging are an important issue that EPs must consider when evaluating patients in the ED.24, 25 EP, both in an effort to rule out life threatening disease and to ensure that no pathology is missed, have become increasingly reliant on diagnostic imaging. Needless to say, frequent users appear to be at an increased risk of radiation exposure given their repeat ED evaluations. Prior to enrollment in the case management program, our group of patients averaged 25.6 CT scans per patient per month, which corresponds to approximately 300 CT studies per patient per year. When followed from the time of their enrollment to the end of the study in November 2008, patients in the case management program averaged 8.1 CT scans per patient per month, which corresponds to approximately 100 CT studies per patient per year. Our case management program thus reduced radiation exposure from CT scans by two-thirds. The reduction in the number of CT studies by 200 per patient per year roughly corresponds to each patient saving about one abdominal CT scan per year. Literature has shown that the average abdominal CT exam has an effective dose of radiation of about 10 mSv, 32 and that the corresponding risk of cancer associated with this dose of radiation is 0.05%, or 1 in 2000.30,32 Although we reduced radiation exposure by two-third in those patients in our case management program, the number needed to treat (NNT) to prevent one cancer per year is 2,000 patients. However, this NNT is only for one year. Should these same patients remain in the case management program and maintain similar ED use patterns, it is likely that one case of cancer due to diagnostic imaging will be prevented in this group of 85 patients over the next 24 years. Our case management program is ongoing, adding new patients every month. As the number of patients’ increases, the number of years needed to prevent one cancer will decrease. Additionally, should a similar case management model be used in other EDs, the number of patients that benefit from reduced radiation exposure will continue to rise.
LIMITATIONS
Our study had several limitations. First, it is limited by a relatively small number of patients enrolled in the program. Second, our retrospective observational study design has inherent limitations. The patients in our study represented the group using emergency services the most, and without randomization it is difficult to exclude regression towards the mean as an explanation for our findings. Third, our selection of patients may have been biased towards those with narcotic use issues, as patients could be enrolled in the case management program simply if staff expressed concerns about a patient. Those with chronic pain or those seeking narcotics are often very difficult to manage, and thus may have been disproportionally enrolled in the program, based upon staff concern. This effect may have been compounded by the fact that inclusion criteria also included notification by the California prescription drug monitoring program.
An additional weakness is that the original program design depended on all patients in case management to be immediately identified upon arrival to the ED to rapidly implement their case management plan. Due to limitations in status board software and staff recognition of patients in the program, patients were not always identified upon presentation. Thus, on rare occasions, patients in case management were not identified at all and given treatment conflicting with their care plan. Similarly, on rare occasions the recognition of patients was delayed until after they had already been given treatment in conflict with their care plan. Such lapses in the case management plan may have encouraged patients to attempt to resume higher frequency of use in the attempt to obtain restricted treatments. However, it is our experience that high frequency use patterns are maintained in only those patients whose case management plans are consistently ignored by treating staff. It is for this reason that only the four patients whose plans were repeatedly disregarded were excluded from the analysis.
Finally, as much as we attempted to determine whether or not our program was successful in actually treating patients’ chronic problems by comparing chief complaints before and after enrollment, we have no direct measure of patient satisfaction with the program and no measure of the quality of life of our patients before or after enrollment. Many of our patients chose to never return to the department for care or only seek care in the department when emergent conditions arose, which makes their assessment rather difficult. Similarly, our IRB approval was only for a retrospective chart analysis.
DIRECTIONS FOR FUTURE STUDY
While our data shows that the patients in our case management program markedly decreased use of our ED, it is not clear how their use of other healthcare sites changed after enrollment in the program. There are two other community hospitals and one small county hospital within 35 miles of our study site. To improve care of the patients in our community, we plan to work with the surrounding hospitals to both assess frequent use patterns at the surrounding hospitals and create a group case management program. Additionally, our current data do not measure to what extent patient use of primary care resources changed before and after enrollment. We also plan to work more closely with the PMD in the community to assess how our case management program affects the use of primary care resources.
Additionally, our study was limited by the small number of patients enrolled, the inherent limitations of a retrospective analysis, and our lack of assessment of patient satisfaction and quality of life. Given our success with this pilot study, we plan further and more methodologically sound research to better study our frequent users program.
Finally, one of the most important lessons that we have learned in the operation of the case management program is that its success is contingent upon staff compliance with patient plans. As mentioned previously, there were instances in which patients whose plans involved the restriction of narcotics were not recognized, and they were able to obtain narcotics. In these cases, patients returned to the ED multiple times in the following days, ostensibly in hope of obtaining narcotics again. The biggest obstacle we face to improve compliance with case management plans is that our status board software does not display whether or not patients have case management plans. Case management status is only currently listed if a patient is recognized by staff and a note is placed in the comments section under that patient’s name. We have been discussing this issue with our software provider in an attempt to resolve this issue and look forward to creating a system in which case management patients are readily identified by all staff in the department.
CONCLUSION
Case management for frequent users of the ED is an effective way to reduce repeat use of emergency services and to reduce radiation exposure from repetitive diagnostic imaging. Furthermore, chronic pain and substance abuse are prevalent issues in ED frequent users and should be considered in the evaluation of these patients.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted June 20, 2009; Revision Received September 12, 2009; Accepted December 27, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Casey A Grover c/o Reb JH Close, MD, Department of Emergency Medicine, Community Hospital of the Monterey Peninsula, PO Box HH, Monterey, CA 93942
Email: caseygrover@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Hunt KA, Weber EJ, Showstack JA, et al. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006 Jul;48(1):1–8. Epub 2006 Mar 30. [PubMed]
2. Byrne M, Murphy AW, Plunkett PK, et al. Frequent attenders to an emergency department: a study of primary health care use, medical profile, and psychosocial characteristics. Ann Emerg Med. 2003 Mar;41(3):309–18. [PubMed]
3. Locker TE, Baston S, Mason SM, et al. Defining frequent use of an urban emergency department.Emerg Med J. 2007 Jun;24(6):398–401. [PMC free article] [PubMed]
4. Ledoux Y, Minner P. Occasional and frequent repeaters in a psychiatric emergency room. Soc Psychiatry Psychiatr Epidemiol. 2006 Feb;41(2):115–21. Epub 2006 Jan 31. [PubMed]
5. D’Onofrio G. Treatment for alcohol and other drug problems: closing the gap. Ann Emerg Med.2003;41:814–7. [PubMed]
6. Rockett IRH, Putnam SL, Jia H, et al. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann Emerg Med. 2003;41:802–13. [PubMed]
7. Chan BTB, Ovens HJ. Frequent users of emergency departments. Do they also use family physicians’ services? Can Fam Physician. 2002;48:1654–60. [PMC free article] [PubMed]
8. Hansen GR. The drug seeking patient in the emergency Room. Emerg Med Clin North Am. 2005 May;23(2):349–65. [PubMed]
9. Hansen GR. Management of chronic pain in the acute care setting. Emerg Med Clin North Am.2005 May;23(2):307–38. [PubMed]
10. Malone RE. Whither the almshouse? Overutilization and the role of the emergency department. J Health Polit Policy Law. 1998 Oct;23(5):795–832. [PubMed]
11. Sadowski LS, Kee RA, VanderWeele TJ, et al. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. JAMA. 2009 May;301(17):1771–8. [PubMed]
12. Shumway M, Boccellari A, O’Brien K, et al. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial. Am J Emerg Med. 2008 Feb;26(2):155–64. [PubMed]
13. Care plans for frequent flyers save money, cut costs. Hosp Case Manag. 2006 Feb;14(2):22, 30–1.[PubMed]
14. Belcher JV, Alexy B. High-resource hospital users in an integrated delivery system. J Nurs Adm.1999 Oct;29(10):30–6. [PubMed]
15. Report: 9 Made 2, 7000 ER Visits in 6 Years. CBS NEWS Web site. Available at:http://www.cbsnews.com/stories/2009/04/02/health/main4912621.shtml. Accessed September 7, 2009.
16. Spillane LL, Lumb EW, Cobaugh DJ, et al. Frequent users of the emergency department: can we intervene. Acad Emerg Med. 1997 Jun;4(6):574–80. [PubMed]
17. Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000 Jun;7(6):637–46. [PubMed]
18. Svenson JE, Meyer TD. Effectiveness of nonnarcotic protocol for the treatment of acute exacerbations of chronic nonmalignant pain. Am J Emerg Med. 2007 May;25(4):445–9. [PubMed]
19. MacLeod DB, Swanson R. A new approach to chronic pain in the ED. Am J Emerg Med.1996;14:323–6. [PubMed]
20. Bernstein E, Bernstein J, Leverson S. Project ASSERT: an ED-based intervention to increase access to primary care, preventive services, and substance abuse treatment system. Ann Emerg Med. 1997;30:181–9. [PubMed]
21. Okin RL, Boccellari A, Azocar F, et al. The effects of clinical case management on hospital service use among ED frequent users. Am J Emerg Med. 2000 Sep;18(5):603–8. [PubMed]
22. Pope D. Frequent users of the emergency department: a program to improve care and reduce visits. Can Med Assoc J. 2000;162:1017–20. [PMC free article] [PubMed]
23. Murphy AW. ‘Inappropriate’ attenders at accident and emergency departments II: health service responses. Fam Pract. 1998 Feb;15(1):33–7. [PubMed]
24. Schwartz DT. Counter-point: Are we really ordering too many CT Scans. West J Emerg Med. 2008 May;9(2):120–2. [PMC free article] [PubMed]
25. Henderson SO. Point: Diagnostic Radiation: Why aren’t we stopping. West J Emerg Med. 2008 May;9(2):118–9. [PMC free article] [PubMed]
26. Nagurney JT, Brown DF, Chang Y, et al. Use of diagnostic testing in the emergency department for patients presenting with non-traumatic abdominal pain. J Emerg Med. 2003;25:363–371.[PubMed]
27. Kowalski RG, Claassen J, Kreiter KT, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA. 2004 Feb;291(7):866–9. [PubMed]
28. Tien HC, Tremblay LN, Rizoli SB, et al. Radiation exposure from diagnostic imaging in severely injured trauma patients. J Trauma. 2007 Jan;62(1):151–6. [PubMed]
29. Amis ES, Jr, Butler PF, Applegate KE, et al. American college of radiology American college of radiology white paper on radiation dose in medicine. J Am Col Radiol. 2007 May;4(5):272–84.
30. Katz SI, Saluja S, Brink JA, et al. Radiation dose associated with unenhanced CT for suspected renal colic: impact of repetitive studies. Am J Roentgenol. 2006 Apr;186(4):1120–4. [PubMed]
31. Brenner DJ, Elliston CD. Estimated radiation risks potentially associated with full-body CT screening. Radiology. 2004;232:735–8. [PubMed]
32. Dixon AK, Dendy P. Spiral CT: how much does radiation dose matter? Lancet. 1998;352:1082–3.[PubMed]
33. Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. New Eng J Med. 2007;357:2277–84. [PubMed]
34. Ruger JP, Richter CJ, Spitznagel EL, et al. Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad Emerg Med.2004 Dec;11(12):1311–7. [PubMed]
35. Murphy AW. In appropriate attenders at accident and emergency departments: definition, incidence, and reasons for attendance. Fam Pract. 1998 Feb;15(1):23–32. [PubMed]
36. McPheeters RA. Counter-Point: Frequent users of the emergency department: meeting society’s needs. West J Emerg Med. 2009 Aug;10(3):195–6. [PMC free article] [PubMed]
37. Zednich AD, Hedges JR. Community-wide emergency department visits by patients suspected of drug-seeking behavior. Acad Emerg Med. 1993;3:312–7.
38. The Lewin Group American Hospital Association Trendwatch Chartbook. American Hospital Association; Chicago, IL: 2004.


