| Author | Affiliation |
|---|---|
| Simon A. Mahler, MD | Louisiana State University Health Sciences Center Department of Emergency Medicine, Shreveport, LA |
| Hoi Y. Chan | Louisiana State University Health Sciences Center Department of Emergency Medicine, Shreveport, LA |
| Donna L. Carden, MD | University of Florida, Department of Emergency Medicine, Gainesville, Florida |
| Christopher Wolcott, MD | Louisiana State University Health Sciences Center Department of Emergency Medicine, Shreveport, LA |
| Steven A. Conrad, MD | Louisiana State University Health Sciences Center Department of Emergency Medicine, Shreveport, LA |
ABSTRACT
Introduction:
Despite American College of Cardiology (ACC) and American Heart Association (AHA) guidelines, many hospitals have door-to-balloon times in excess of 90 minutes. Emergency Department (ED) activation of interventional cardiology has been described as an important strategy to reduce door-to-balloon time. However, prior studies on ED activation have been in suburban hospitals with door-to-balloon times near the ACC/AHA targeted times. To determine if ED activation of interventional cardiology could significantly improve reperfusion times and reach the ACC/AHA target of 90 minutes or less in a safety net hospital, a Level I trauma center and teaching hospital serving primarily uninsured and underinsured patient population with door-to-balloon times ranking in the lowest quartile of United States hospitals.
Methods:
In this study, door-to balloon times before and after implementation of ED activation were compared by retrospective chart review.
Results:
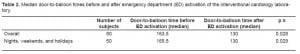
Eighty patients were included in the study, 48 before and 32 after ED activation of interventional cardiology. Median door-to-balloon time decreased from 163.5 minutes before to 130 minutes after ED activation, a significant difference of 33.5 minutes (p=0.028). Door-to-balloon time on nights, weekends and holidays decreased from a median of 165.5 minutes to 130 minutes, a reduction of 35.5 minutes, which also reached statistical significance (p=0.029).
Conclusion:
ED activation of interventional cardiology produced a statistically significant reduction in door-to-balloon time. However, the reduction was not enough to achieve a door-to-balloon time of less than 90 minutes. Safety net hospitals with door-to-balloon times in the lowest quartile nationally may require multiple strategies to achieve targeted myocardial reperfusion times.
INTRODUCTION
Timely percutaneous coronary intervention (PCI) with balloon angioplasty reduces morbidity and mortality of patients with ST-elevation myocardial infarction (STEMI).1,2 American College of Cardiology (ACC) and American Heart Association (AHA) guidelines recommend that a STEMI patient presenting to the Emergency Department (ED) have door-to-balloon times of 90 minutes or less.3 The Joint Commission has identified door-to-balloon time of less than 90 minutes as a core measure of healthcare quality.
Despite ACC/AHA guidelines, many hospitals have median door to balloon times in excess of 90 minutes.4–6 A recent study calculated door-to-balloon time for 365 United States hospitals and found a median door-to-balloon time of 100.4 minutes. More than 15% of hospitals in this study had median door-to-balloon times greater than 120 minutes.5 An observational study by the National Registry of Myocardial Infarction examined door-to-balloon times for 13,387 STEMI patients and found a mean time of 113 minutes.7 Many hospitals have explored strategies to reduce door-to-balloon time, and the ACC/AHA has recently created a campaign for improving reperfusion times called “GAP-D2B: An Alliance for Quality.” The goal of this initiative is to increase the percentage of patients in U.S. hospitals receiving PCI within 90 minutes from the current level of 35% to 75%.8
An effective yet infrequently used strategy to reduce door-to-balloon time is ED physician activation of interventional cardiology upon identification of a STEMI on electrocardiogram (ECG). 5, 9–14Commonly, interventional cardiology teams are activated by a cardiology fellow or cardiologist after they have been consulted by the emergency physician (EP).5 The process of consultation can be time consuming, particularly if the cardiologist is not in the hospital and must evaluate the patient in the ED prior to activating the interventional cardiology team. By allowing the EP to activate the cardiac catheterization laboratory, the time previously used for cardiology consultation is eliminated. Several recent retrospective studies and a survey of U.S. hospitals suggest that ED activation of the catheterization laboratory significantly reduces door-to-balloon time.5, 9–14
Several reports in the recent literature documenting improvements in door-to-balloon times due to ED activation of interventional cardiology were conducted in suburban hospitals, with initial reperfusion times at or below the ACC/AHA targets.9–11 While ED activation has improved door-to-balloon times in these study settings, the results may not be generalizable to all practice environments. The effect of ED activation in hospitals caring for mostly uninsured or under-insured patients, the so-called safety net hospitals, is less clear. The purpose of this investigation was to determine the effect of ED activation of interventional cardiology in a safety net hospital with a ranking in the lowest quartile of U.S. hospitals for reperfusion times.5
METHODS
We retrospectively studied patients with STEMI or a new left bundle branch block, presenting to Louisianna State University Health Sciences Center Shreveport ED from November 2004 to May 2009. STEMI was defined by the ACC/AHA ECG criteria as an elevation of the ST segment greater than 1 mm in two or more contiguous leads.3 The protocol compared door-to balloon times before and after implementation of a policy in October 2006, that allowed ED activation of interventional cardiology. This study was approved by the institutional review board of the sponsoring organization.
Louisianna State University Health Sciences Center Shreveport is a teaching hospital, Level I trauma center and tertiary care center serving a largely uninsured or underinsured patient population. PCI is available 24 hours a day. However, from 5:00 PM to 7:00 AM on weekdays, weekends and holidays (after-hours), the interventional cardiology team must be called from home. Prior to October 2006, the interventional cardiology team could only be activated by a cardiology fellow or cardiology attending physician.
We conducted a chart review on each patient presenting to the ED with a STEMI during the 55-month study period. The data collected included a “door time,” which was recorded on the nursing record. If a patient had no recorded door or balloon time, they were excluded from the study. Time intervals were calculated separately by two of the authors and any disagreement was settled by consensus.
We separated patient data into two groups, before and after ED activation of interventional cardiology. Patient characteristics, such as age, race, and gender, were compared between the two groups (using a t-test for age and nonparametric analysis for age and gender). We compared median door-to-balloon times in the two groups using nonparametric analysis with a Wilcoxon Mann-Whitney test. Patients were also separated into daytime (Monday–Friday; 7am–5pm) and after-hours subgroups (weeknights 5pm–7am, weekends and holidays) in both the before and after ED activation groups. Subgroup statistical analysis was conducted with nonparametric analysis. A p value of less than 0.05 was considered statistically significant. All statistical analysis was preformed with SPSS 11.0 (Chicago, Illinois) for windows.
RESULTS
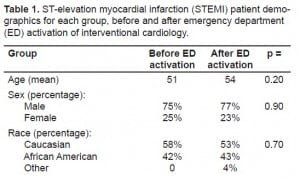
During the 55-month study period, we identified 85 STEMI patients of which five were excluded for a missing door or balloon time. There were no subjects identified as receiving emergent catheterization for a new left bundle branch block. We performed data analysis on 80 patients, 48 prior to ED activation of interventional cardiology and 32 after. The two groups were similar in patient characteristics, such as race, age, and gender (Table 1). Median door-to-balloon time for the before and after groups was 163.5 minutes and 130 minutes respectively. Implementation of ED activation of interventional cardiology reduced median door-to-balloon time by 33.5 minutes, which reached statistical significance (p=0.028). Patients presenting during after hours had median door-to-balloon times of 165.5 minutes before and 130 minutes after ED activation of interventional cardiology. This represents a reduction of 35.5 minutes, a result that also reached statistical significance (p=0.029). Despite a significant decrease in median door-to-balloon time, ED activation failed to achieve the ACC/AHA target of 90 minutes or less. Results are summarized in Table 2.
DISCUSSION
EDs of Level I trauma centers and teaching hospitals, the nation’s safety net hospitals, are some of the busiest and most crowded in the United States.15 Moreover, ED crowding has been associated with adverse cardiovascular outcomes, such as delayed door-to-needle time in patients thrombolyzed in the ED for suspected acute myocardial infarction.16 Thus, measures shown to reduce door-to-balloon time in suburban hospitals with reperfusion times approaching the Joint Commission and ACC/AHA target times may not be effective in all healthcare environments, particularly, safety net hospitals. The purpose of this study was to determine the effect of ED activation of interventional cardiology in a Level I trauma center and teaching hospital with door-to-balloon times in the lowest quartile of U.S. hospitals. Our results demonstrate that ED activation of interventional cardiology significantly reduced door-to-balloon times. However, it failed to reduce the median door-to-balloon time to the ACC/AHA and Joint Commission target of 90 minutes or less.
Failure to reduce door-to-balloon times below 90 minutes through ED activation of interventional cardiology is not unique to this study. Despite statistically significant results, three of six previous studies on ED activation failed to achieve door-to-balloon times of less than 90 minutes.12–14 In fact, only two studies demonstrated reductions in door-to-balloon times to less than 90 minutes in institutions where reperfusion times were in excess of ACC/AHA recommendations.10–11
Accurately defining delays that occur in safety net hospitals may provide strategies to improve door-to-balloon times in similar hospitals nationwide. To achieve this goal it may be useful to separate door-to-balloon times into component intervals. Two important intervals that comprise total door-to-balloon time are door-to-activation time and activation-to-balloon time. EP activation of the interventional cardiology team is a strategy aimed at reducing door-to-activation time. Other steps described in the literature to reduce door-to-activation time include policies for decreasing door-to-ECG time. Unfortunately, these policies appear to have little effect on door-to-balloon time and may not be the best option to decrease reperfusion times in many healthcare environments.5Several studies have demonstrated reduction of door-to-balloon times by prehospital activation of the interventional cardiology team.17
Another important component of door-to-balloon time is the activation-to-balloon time interval. It has been demonstrated that significant transport delays are associated with a policy of having patients wait in the ED until the catheterization laboratory communicates readiness for patient transport. Hospitals that transport the patient at a set time interval following activation of the catheterization laboratory have significantly shorter door-to-balloon times.5 Real-time feedback for ED and catheterization laboratory personnel was also recently reported as having a significant effect on overall door-to-balloon times.5
Door-to-balloon time in the current study appeared to be influenced by the time of patient presentation to the ED. When the interventional cardiology team is not in the hospital, potential delays may occur in team communication, in transit to the hospital, in setting up necessary equipment, and in patient transport to the catheterization laboratory. Expectations that the interventional cardiology team arrive in the catheterization laboratory within 20 minutes of team activation have been strongly associated with reduction in door-to-balloon times. Thus, further defining reasons for activation-to-balloon delays during after-hours may reduce overall door-to-balloon time in a variety of healthcare environments.
LIMITATIONS
There are several limitations of this study. For example, retrospective studies generally demonstrate associations rather than causation and therefore generate less meaningful results than prospective, randomized trials. Chart reviews are also limited by inaccurate or incomplete records. Most data points used in this study came from nursing notes or physician’s documentation, which are subject to human error and bias. Bias can also be introduced as investigators interpret absent or conflicting data. The authors attempted to limit bias by using a standardized data collection method with uniform handling of missing or conflicting data and by having the authors independently review many of the same charts. Further, five patients were excluded from data analysis for missing door or balloon times. This study may also be limited by a small number of patients enrolled. However, previous studies such as Jacoby et al.11, Singer et al.12 and Kraft et al.14 were also small with only 44, 88 and 97 patients respectively. All three of these studies were able to demonstrate statistically significant reductions in door-to-balloon time despite their small patient enrollment.
CONCLUSION
The results of this study and review of the literature suggest that ED activation of the interventional cardiology team may not be sufficient to reduce door-to-balloon times below the ACC/AHA goal of 90 minutes in all healthcare environments. Although not proven in this study, it is possible the nation’s safety net hospitals require other strategies in addition to ED activation of interventional cardiology to reduce overall door-to-balloon times and improve myocardial reperfusion.
Footnotes
Supervising Section Editor: Jeffrey Druck, MD
Submission history: Submitted July 23, 2009; Revision Received December 4, 2009; Accepted December 27, 2009
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for Correspondence: Simon A. Mahler, MD, Department of Emergency Medicine, Louisiana State University Health Sciences Center-Shreveport, 1501 Kings Hwy, Shreveport, LA 71130
Email smahle@lsuhsc.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283:2941–7. [PubMed]
2. Berger PB, Ellis SG, Holmes DR, Jr, et al. Relationship between delay in performing direct coronary angioplasty in early clinical outcome in patients with acute myocardial infarction: results from the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes (GUSTO-IIb) trial.Circulation. 1999;100:14–20. [PubMed]
3. Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction. Circulation. 2008;117:296–329. [PubMed]
4. McNamara RL, Herrin J, Bradley EH, et al. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J AM Coll Cardiol. 2006;47:45–51.[PMC free article] [PubMed]
5. Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. NEJM. 2006;355:2308–20. [PubMed]
6. Williams SC, Schmaltz SP, Morton DJ, et al. Quality of care in U.S. hospitals as reflected by standardized measures, 2002–2004. NEJM. 2005;353:255–64. [PubMed]
7. Bradley EH, Herrin J, Wang Y. et al. Door-to-balloon times; where can we improve? Time to reperfusion therapy in patients with ST-segment elevation myocardial infarction (STEMI) AM Heart J. 2006;151:1281–7. [PubMed]
8. Nissen SE, Brush JE, Krumholz HM, et al. GAP-D2B: An alliance for quality. J AM Coll Cardiol.2006;48:1911–12. [PubMed]
9. Thatcher JL, Giseth TA, Adlis S. Improved efficiency in acute myocardial infarction care through commitment to emergency department-initiated primary PCI. J Inv Cardiol. 2003;15:693–8.
10. Khot UN, Johnoson ML, Ramsey C, et al. Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation.2007;116:67–76. [PubMed]
11. Jacoby J, Axelband J, Patterson J, et al. Cardiac cath lab activation by the emergency physician without prior consultation decreases door-to-balloon time. J Inv Cardiol. 2005;17:154–5.
12. Singer AJ, Shembekar A, Visram F, et al. Emergency department activation of an interventional cardiology team reduces door-to-balloon times in ST-segment-elevation myocardial infarction. Ann Emerg Med. 2007;50:538–44. [PubMed]
13. Kurz MC, Babcock C, Sinha S, et al. The impact of emergency physician-initiated primary percutaneous coronary intervention on mean door-to-balloon time in patients with ST segment-elevation myocardial infarction. Ann Emerg Med. 2007;50:527–34. [PubMed]
14. Kraft PL, Newman S, Hanson D, et al. Emergency physician discretion to activate the cardiac catheterization team decreases door-to-balloon time for acute ST-elevation myocardial infarction.Ann Emerg Med. 2007;50:520–6. [PubMed]
15. United States General Accounting Office Report to the ranking minority member committee on finance. Hospital emergency departments. Crowded conditions vary among hospitals and communities. Mar, 2003. GAO-03-460;
16. Schull MJ, Vermeulen M, Slaughter G, et al. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577–85. [PubMed]
17. Brown JP, Mahmud E, Dunford JV, et al. Effect of prehospital 12-lead electrocardiogram on activation of the cardiac catheterization laboratory and door-to-ballon time in ST-segment elevation acute myocardial infarction. Am J Cardiol. 2008;101:158–61. [PubMed]


