| Author | Affiliation |
|---|---|
| J. Christian Fox, MD, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Seric Cusick, MD, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| William Scruggs, MD, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Travis W. Henson, MD | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Craig L Anderson, MPH, PhD | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Graciela Barajas, BS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Alexander Zlidenny, MD, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| JoAnne McDonough, MD, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
| Mark I. Langdorf, MD, MHPE, RDMS | Department of Emergency Medicine, University of California, Irvine School of Medicine |
ABSTRACT
Introduction
Medical student ultrasound education is sparse. In 2002, we began the first medical student rotation in emergency ultrasound. To evaluate if medical students can learn and retain sonographic skills during a two- or four-week elective.
Methods
We gave students an exam on the first and last days of the rotation. Six months later, students took the exam a third time. A control group was used for comparison.
Results
Over a 19-month period, we enrolled 45 students (25 on the two-week and 20 on the four-week elective). The four-week student post-test score was significantly better than the two- week post-test score (81% vs 72%, p=0.003). On the six-month exam, the four-week student post-test score was significantly better than the two-week post-test score (77% vs 69%, p=0.008). The control group did not statistically improve.
Conclusion
Medical students can learn bedside ultrasound interpretation with clinical integration and retain the knowledge six months later.
INTRODUCTION
Emergency physicians (EPs) have used bedside ultrasound for almost two decades1,2 with studies demonstrating its accuracy and utility.3–15 Bedside ultrasound is required for residency training in Emergency Medicine (EM)6 and is used in other specialties, but it is not routinely taught in U.S. medical schools. Several studies have evaluated emergency ultrasound (EU) curricula for resident and practicing physicians, but this is the first study to address medical student learning in emergency ultrasound. 16–19
We established the first Emergency Department (ED)-based, fourth-year medical student rotation for EU in 2002. We offer both two- and four-week rotations. Each week includes two hours of didactics and five hours of image interpretation review (approximately 100 scans), the content of which varied during the study period according to patient variability and didactic scheduling. Each student spent 40 hours per week in the ED performing bedside ultrasounds with supervision by resident and attending EPs. This EM group consists of several registered diagnostic medical sonographer (RDMS) certified-physicians and other EPs who hold hospital credentialing in the interpretation of EU. Each student had the opportunity to work with a variety of attending EPs, including the emergency ultrasound fellow and the director of emergency ultrasound.
Purposes
We sought to determine if these rotations promote improved image interpretation and clinical integration, and whether these skills were retained six-months later. Furthermore, we hypothesized that students would score better after a four-week than a two-week rotation.
METHODS
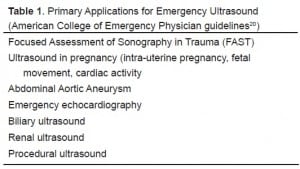
We prospectively enrolled medical students over a 19-month period at our academic, urban, Level I trauma center ED. Informed consent was obtained from each student. We designed a 35-question exam, covering the primary applications of EU as described in the American College of Emergency Physicians Emergency Ultrasound Guidelines (Table 1).20 In addition, we tested ocular ultrasound, detection of soft-tissue abscess, and deep venous thrombosis (DVT). Of the 35 questions, 13 assessed physics and image-acquisition techniques, 13 involved image interpretation with clinical integration, and nine were purely image interpretation, with the majority of the images demonstrating positive findings. An interactive DVD with live ultrasound video clips accompanied the exam (available on journal website at www.insertdvdtesthere.com). The university IRB committee approved the study.
We instructed students in ultrasound physics and instrumentation, and aortic, biliary, pelvic (transabdominal/endovaginal), renal, DVT, trauma, cardiac, soft tissue, and ocular ultrasound. Students also did four hours of DVD self-study in both rotations. Didactic and tape review instructors were RDMS-certified EM faculty and fellows. Finally, students were encouraged to read a 500-page collection of selected ultrasound textbook chapters and research articles.
On the first day of the elective, students were approached for enrollment whether on the two or four week rotation, and before any ultrasound instruction. None refused. We planned to exclude students if they had prior ultrasound instruction or experience. None did. Students took the exam on day one and again on the final day of their rotation. Six months after the completion of the rotation, a follow-up exam with DVD was mailed to the students to be completed at their convenience. The same exam was used each time, but students were blinded to both the correct answers and their previous score. Students who completed the six-month exam received a gift card for a large, multi-national coffee chain. Nine students who did not take the emergency ultrasound rotation (control group) took the same exam on two occasions four weeks apart. We calculated p-values using the Student’s t-test, analysis of variance (ANOVA), and a linear regression model that included the pre-test score and a binary variable for the difference between the two and four week electives. Statistical significance was set at p < 0.05.
RESULTS
Over a 19-month period, we enrolled 45 students (25 on the two-week and 20 on the four-week elective). Their results are summarized in Table 2. Thirty-four of 45 students (76%) completed the six-month follow-up exam. Table 3 shows these results compared to the four-week group’s pre-tests.
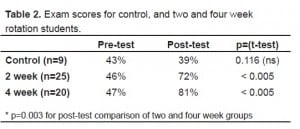
Exam scores for control, and two and four week rotation students.
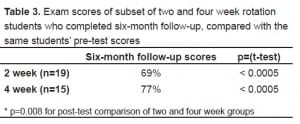
Exam scores of subset of two and four week rotation students who completed six-month follow-up, compared with the same students’ pre-test scores
There was no difference between pre-test scores in the three groups (p=0.688 by ANOVA). However, there was a statistically significant improvement in the post-test scores for the four-week group as compared with the two-week group (p=0.005), as well as six-month follow-up scores between the groups (p=0.008). These two comparisons were made using linear regression controlling for pre-test scores. Therefore, not only did scores improve after the two and four week rotations, but both groups retained this improved performance at the six-month follow up.
DISCUSSION
This study is the first to investigate the effectiveness of a medical student rotation in bedside ultrasound in the ED. Such education is broadly applicable outside of EM, including obstetrics and gynecology, surgery, critical care and office-based practices. Our results demonstrate that students have a significant increase in their ability to interpret ultrasound images and integrate them into clinical decision-making after a short period of training. Although the students on the four-week rotation showed a greater improvement than the two-week students at both the completion of the rotation and the six-month follow up, the two-week students nonetheless showed a significant improvement. These results suggest that incorporating ultrasound education into medical school curricula is feasible and can be successful in a short rotation.
More than 32,000 emergency physicians practice in the United States, but only a small fraction are ultrasound trained. A recent survey documents that ultrasound equipment is consistently available in only 19% of U.S. EDs.21 The primary reason cited for this limited availability was lack of EP training. Our study of medical students suggests relatively short, focused periods of training are effective and may begin to bridge this training gap.
LIMITATIONS
This study tested image interpretation and integration into patient management but did not test actual image acquisition. Therefore, we cannot comment on whether two or four weeks of bedside training is sufficient to develop and retain these skills. As our exam addressed clinical management of patients based on ultrasound findings, we cannot separate ultrasound skills from improved clinical acumen during the rotation. It is possible that students who chose a four-week elective in EU are more motivated to learn EM than those choosing two weeks, and this could account for the improved test performance. Furthermore, an inclusion bias may be present; the 76% that chose to complete the six- month follow-up examination may have been the same students who were more motivated during the rotation and had greater retention of information.
The examination focused on detection of “positive” ultrasound findings suggestive of pathology. To most accurately assess image-interpretation skills, a more thorough exam would have consisted of multiple normal, abnormal and indeterminate examples for each indication; however, the investigators were concerned that a lengthier exam could have decreased the completion rate. Given that the pre- and post-test were identical, we cannot exclude improvement in scores based simply on taking the same test twice. However, our control group, with no ultrasound training did not improve their test scores, making this confounder unlikely. Due to the variable nature of the ED patient population, the bedside ultrasounds performed by the students and the images available for review during the image interpretation sessions were not controlled for and may have affected individual student performance on questions evaluating certain applications.
We also did not control for the number of scans that either group performed, the random variability in the proportion of each type of scan performed by each student, or any ultrasound experience following the post-test but preceding the six-month follow-up examination. Finally, this educational study was performed at only one site, and therefore generalizability is limited.
CONCLUSION
This study demonstrates that medical students are able to acquire skills necessary for image interpretation of fundamental emergency ultrasound applications and integrate this into clinical scenarios. A four-week rotation is superior to a two-week rotation. Students are able to retain a significant amount of their training six months after the rotation.
Footnotes
Submission history: Submitted May 8, 2007; Accepted July 9, 2007.
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: J. Christian Fox, M.D. Department of Emergency Medicine, University of California, Irvine, 101 The City Drive, Orange, California 92868
Email: jchristianfox@gmail.com
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. Jehle D, Davis E, Evans T, Harchelroad F, Martin M, Zaiser K, Lucid J. Emergency department sonography by emergency physicians. Am J Emerg Med. 1989;7:605–611.[PubMed]
2. Heller M, Melanson SW. Applications for ultrasonography in the emergency department. Emerg Med Clin North Am. 1997;15:735–744. [PubMed]
3. Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med.2005;12:844–849. [PubMed]
4. Squire BT, Fox JC, Anderson CL. Abscess: applied bedside sonography for convenient evaluation of superficial soft tissue infections. Acad Emerg Med. 2005;12:601–606.[PubMed]
5. Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879–885. [PubMed]
6. Schlager D, Lazzareschi G, Whitten D, Sanders AB. A prospective study of ultrasonography in the ED by emergency physicians. Am J Emerg Med. 1994;12:185–189. [PubMed]
7. Miller AH, Roth BA, Mills TJ, Woody JR, Longmoor CE, Foster B. Ultrasound guidance versus the landmark technique for the placement of central venous catheters in the emergency department. Acad Emerg Med. 2002;9:800–805. [PubMed]
8. Kuhn M, Bonnin RL, Davey MJ, Rowland JL, Langlois SL. Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate, and advantageous. Ann Emerg Med. 2000;36:219–223. [PubMed]
9. Rodgerson JD, Heegaard WG, Plummer D, Hicks J, Clinton J, Sterner S. Emergency department right upper quadrant ultrasound is associated with a reduced time to diagnosis and treatment of ruptured ectopic pregnancies. Acad Emerg Med. 2001;8:331–336. [PubMed]
10. Costantino TG, Bruno EC, Handly N, Dean AJ. Accuracy of emergency medicine ultrasound in the evaluation of abdominal aortic aneurysm. J Emerg Med. 2005;29:455–460. [PubMed]
11. Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46:456–461. [PubMed]
12. Frazee BW, Snoey ER, Levitt A. Emergency Department compression ultrasound to diagnose proximal deep vein thrombosis. J Emerg Med. 2001;20:107–112. [PubMed]
13. Mandavia DP, Hoffner RJ, Mahaney K, Henderson SO. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38:377–382. [PubMed]
14. Kendall JL, Shimp RJ. Performance and interpretation of focused right upper quadrant ultrasound by emergency physicians. J Emerg Med. 2001;21:7–13. [PubMed]
15. Blaivas M. Incidence of pericardial effusion in patients presenting to the emergency department with unexplained dyspnea. Acad Emerg Med. 2001;8:1143–1146. [PubMed]
16. Jang T, Aubin C, Naunheim R. Minimum training for right upper quadrant ultrasonography. Am J Emerg Med. 2004;22:439–443. [PubMed]
17. Jang T, Sineff S, Naunheim R, Aubin C. Residents should not independently perform focused abdominal sonography for trauma after 10 training examinations. J Ultrasound Med. 2004;23:793–797. [PubMed]
18. Jang T, Docherty M, Aubin C, Polites G. Resident-performed compression ultrasonography for the detection of proximal deep vein thrombosis: fast and accurate.Acad Emerg Med. 2004;11:319–322. [PubMed]
19. Blaivas M, Theodoro D. Comparison of perceived and actual times spent by residents performing ultrasound examinations on patients. Acad Emerg Med. 2003;10:397–399.[PubMed]
20. American College of Emergency Physicians. ACEP emergency ultrasound guidelines-2001. Ann Emerg Med. 2001;38:470–481. [PubMed]
21. Moore CL, Molina AA, Lin H. Ultrasonography in community emergency departments in the United States: access to ultrasonography performed by consultants and status of emergency physician-performed ultrasonography. Ann Emerg Med. 2006;47:147–153.[PubMed]