| Author | Affiliation |
|---|---|
| Robert M. Rodriguez, MD | Department of Emergency Services, San Francisco General Hospital, University of California San Francisco, San Francisco, CA |
| Opal Taylor, MD | Department of Emergency Medicine, Alameda County Medical Center, Oakland, CA |
| Sushma Shah, MD | Department of Emergency Medicine, Alameda County Medical Center, Oakland, CA |
| Susan Urstein, MD | Department of Emergency Medicine, Alameda County Medical Center, Oakland, CA |
ABSTRACT
Introduction
In a sample of patients undergoing procedural deep sedation in the emergency department (ED), we conducted a prospective, randomized, single-blinded trial of audio-therapy for smoking cessation.
Methods
We asked subjects about their smoking, including desire to quit (0–10 numerical scale) and number of cigarettes smoked per day. Subjects were randomized to either a control tape (music alone) or a tape with repeated smoking-cessation messages over music. Tapes were started with first doses of sedation and stopped with patient arousal. Telephone follow-up occurred between two weeks and three months to assess the number of cigarettes smoked per day. Study endpoints were self-reported complete cessation and decrease of half or more in total cigarettes smoked per day.
Results
One hundred eleven patients were enrolled in the study, 54 to intervention and 57 to control. Mean desire to quit was 7.15 ± 2.6 and mean cigarettes per day was 17.5 ± 12.1. We successfully contacted 69 (62%) patients. Twenty-seven percent of intervention and 26% of control patients quit (mean difference = 1%; 95% CI: −22.0% to 18.8%). Thirty-seven percent of intervention and 51% of control patients decreased smoking by half or more (mean difference = 14.6%; 95% CI: −8.7% to 35.6%).
Conclusion
Suggestive audio-therapy delivered during deep sedation in the ED did not significantly decrease self-reported smoking behavior.
INTRODUCTION
Cigarette smoking is the leading modifiable cause of disease in the United States.1Approximately 440,000 people die annually of cigarette smoking-related causes, with an associated 5.6 million years of potential life lost. At least $75 billion are spent in the treatment of smoking-related illness.2 It is estimated that 8.6 million Americans have serious illnesses attributed to smoking, and about 10% of all current and former adult smokers have a smoking-attributable chronic illness.3 The burden of smoking-related disease is seen in all healthcare settings, including the emergency department (ED).4,5
Smoking cessation was noted as a national priority for health promotion and disease prevention in Healthy People2000 and 2010.6 Public health authorities in emergency medicine have likewise called for ED–based randomized trials and other interventions.4,5,7 A variety of techniques have been proposed to assist people to quit smoking, and there have been trials suggesting roles for hypnosis and suggestion-based methods for smoking cessation.8–12 Studies of smoking-cessation messages administered by tape recordings (suggestive audio-therapy) delivered during general anesthesia have produced variable results.13–15 Myles14 found significant reductions in overall amount of smoking in patients randomized to intervention in one study, but Myles et al15 failed to demonstrate significant changes in smoking in a second trial. The purpose of our study was to test the hypothesis that suggestive audio-therapy delivered during deep sedation in the ED would decrease subsequent self-reported smoking.
METHODS
Study Design, Setting and Population
This study was a prospective, randomized, single-blinded trial. The two endpoints were complete smoking cessation and a decrease of >50% in the number of cigarettes smoked per day comparing subjects’ pre- and post-intervention self-reports. The study was conducted from January 2001 to December2003 at an urban, county hospital ED with an annual census of approximately 70,000 patients. All adult smokers undergoing procedural deep sedation were eligible for enrollment. The exclusion criteria were: 1) no desire to quit smoking defined as 0 on a 0–10 numerical scale; 2) hearing impairment to the degree that the subject could not hear an audiotape; 3) poor English-language comprehension; and 4) developmental delay, dementia, delirium or current psychiatric illness precluding adequate informed consent. Patients were enrolled when the investigators and research assistants were available, from 8 AM to 8 PM on weekdays.
Study Protocol
Tape Preparation
Thirty minutes of music (Pachelbel’s Canon) was recorded on the control tape. On the intervention tape, after one minute of the music, a scripted smoking-cessation message was recorded by a neurolinguistic professional over the background music. This smoking-cessation message had been used during hypnosis therapy for smoking cessation but had not been validated in any manner. Tapes were labeled “A” (intervention)and “B” (control) by an investigator who was blinded to tape assignment. Tapes were periodically assessed for clarity by clerks who were not involved in the study.
Consent, Randomization, and Enrollment
The institutional review board at our hospital approved the study. All patients undergoing deep sedation during the investigators’ and research assistants’ hours were asked if they smoked cigarettes and if they had any desire to quit. Those who wanted to quit and agreed to participate in the study provided written informed consent. No monetary compensation was offered for participation. Patients were randomized according to a computer-generated random sequence of the letters A and B.
Intervention
In addition to standard demographic questions, subjects were asked about their daily cigarette use and to rate their desire to quit on a numerical rating scale, in which 0 = no desire to quit and 10 = extreme desire to quit. Headphones were placed over subjects’ ears; volume was adjusted during the first minute of equivalent tape so that subjects could hear but investigators could not. Tapes were then stopped and restarted with onset of sedation. The mean total tape playing time was 17.3 ± 4.6 minutes. Tapes were played throughout deep-sedation procedures and terminated on arousal. All patients underwent deep sedation with a sedative and ananalgesic: most commonly, propofol at a mean dose of 189mg and fentanyl at a mean dose of 182 mcg. Sedatives and analgesics were delivered as intermittent boluses according to the ED’s standard deep-sedation protocol, titrating agents to procedural sedation scores of 3 (4-point scale), corresponding to “minimal or no withdrawal to painful stimulus.”
After arousal, subjects were asked if they remembered any portion of the procedure. To preserve blinding of investigators and avoid introduction of bias, subjects were not asked whether they remembered any message delivered by the tapes. Before discharge from the ED, subjects were asked to give their best phone number for contact and were informed that research assistants would be calling them for follow up.
Follow up
Investigators blinded to tape assignment attempted to contact all subjects by telephone beginning two weeks after the ED visit. At least five attempts were made to contact subjects over three months. During follow-up calls, subjects were asked again to quantify their daily cigarette consumption using a standardized data collection instrument.
Data Analysis
Based on a baseline decrease in smoking of approximately25% (estimated placebo effect for the control group), aclinically important decrease in smoking between groups of 20%, a power of 80%, a significance level of 0.05, and aonesided analysis, we calculated a sample size of a total of138 subjects. A midway interim analysis was planned after 69patients to determine potential utility versus futility—defined a priori as a less than 10% chance that the study would demonstrate significant benefit with completion of the original sample size. Baseline characteristics were analyzed using the chi-square test, the Fisher exact test, and the Student’s t test, as indicated. The primary outcome measures were reported as the mean difference between groups with 95% confidence intervals. Data was entered using Microsoft Excel (Microsoft Corporation, Redmond, WA) and analyzed using STATA 7.0(Stata Corporation, College Station, TX).
RESULTS
The study was stopped because of futility. One hundred eleven subjects were enrolled (Table 1). Fifty-four subjects were randomized to the intervention tape, and 57 to the control tape (Figure). Fifty-three percent of intervention-group and 72% of control-group subjects had quit smoking at sometime in the past (Table 2). The most frequent method used was “cold turkey.” Only six (5%) patients from both groups recalled any part of the painful procedure.
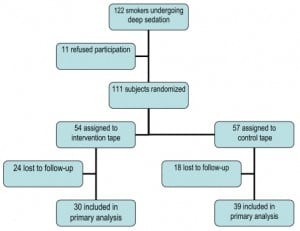
Flow of screening, enrollment, and follow-up of participants.

Characteristics of participants in the study
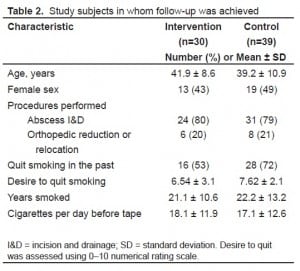
Study subjects in whom follow-up was achieved
Follow up was completed on 62.2% (69/111) of subjects. The control and intervention groups with complete follow up were similar in demographics, proportion that had tried to quit smoking, desire to quit at baseline, and magnitude of smoking(Table 2). There was no significant difference between groups in proportion lost to follow up.
For the primary endpoints, no significant differences were found between groups. Eight of 30 (27%) subjects randomized to the intervention tape (A) and 10 of 39 (26%)subjects randomized to the control tape (B) reported complete cessation (mean difference in proportions = 1%; 95%confidence interval (CI): −22.0% to 18.8%). Eleven of 30(36.7%) intervention patients and 20 of 39 (51.3%) control patients reported a decrease in daily smoking by 50% or more(mean difference in proportions = 14.6%; 95% CI: −8.7% to35.6%).
DISCUSSION
In this prospective, single-blinded, randomized controlled trial, audio-therapy delivered under deep sedation did not decrease self-reported smoking behavior. There are multiple possible explanations. The subjects in this study included a large percentage of patients with a history of current injection drug use (most of whom underwent abscess incision and drainage). Such a group may be less amenable to any treatments for addiction. Other potential causes for the failure include ineffectiveness of the scripted message and a level of sedation too deep to allow reception of the message or learning. In addition, subjects may have declared high motivation to quit despite poor true motivation because of the Hawthorne effect––the change in behavior that results from subjects’ knowledge that they are being studied.
Given that the control group trended toward better results, it is possible, although extremely unlikely, that continuing enrollment to our primary projection of sample size would have resulted in a detectable significant decrease in smoking in the intervention group. Incomplete follow up limited our final sample size for analysis, but our telephone follow-up rate of 60% is comparable to telephone follow-up rates in other ED studies, including another smoking-cessation trial.16,17
The most likely reason for failure to show benefit may be that audio-therapy delivered once over a brief period is simply ineffective at treating smoking addiction. The efficacy of hypnosis itself for smoking cessation is suspect; examinations of hypnosis and other suggestive therapy techniques have produced inconsistent results.8–15,18,19 In a review of 59studies of hypnosis and smoking cessation, Green and Lynn determined that the evidence was inconclusive, and they classified hypnosis techniques as being only “possibly efficacious.” 11 A Cochrane systematic review similarly found marked heterogeneity in studies and concluded that there is no evidence that hypnotherapy is superior to otherinterventions.19
Cigarette smoking is an extremely potent addiction, one that may require a long-term, multifaceted approach for quitting; nicotine replacement in the form of patches or gum is likely necessary to treat the physical dependence. Law20 in a systematic review of smoking-cessation interventions determined that only 2% of smokers stopped the behavior for a year as a direct consequence of personal advice by their physician, but Jorenby et al21 found that nicotine replacement therapy in the form of patches or gum was effective for smoking cessation in 13% of smokers in a placebo-controlled trial. It is possible that hypnosis and audio-suggestive intervention still may play a role in conjunction with such measures directed at physical dependence.22
Other investigators have defined the prevalence ofsmokers,5 noted the substantial effect that smoking has one mergency care,4 and issued a call for “teaching moments” and randomized trials in the ED.4,5,7 In another ED–based study, however, Richman et al17found that providing patients with a scripted counseling message did not result in a change in smoking behavior. Despite the failure to show benefit in the Richman study and in our trial, physicians in urgent care clinics, EDs and other non-continuity of care settings must continue to advocate for smoking cessation and other preventive-care measures. These are the only healthcare access points for millions of Americans, providing primary care(often the only care) for a large segment of the population. A need and desire for preventive care through the ED has been demonstrated,23 and multiple successful preventive care initiatives have been implemented.24–28 It is essential that innovative trials aimed at provision of preventive care in EDs and urgent care clinics continue.
Footnotes
Submission history: Submitted May 8, 2007; Accepted June 9, 2007
Full text available through open access at http://escholarship.org/uc/uciem_westjem
Address for correspondence: Robert M. Rodriguez, MD, Department of Emergency Services, San Francisco General Hospital, 1001 Potrero Ave, San Francisco, CA 94110
Email: rrodriguez@sfghed.ucsf.edu
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
1. CDC. Prevalence of current cigarette smoking among adults and changes in prevalence of current and some day smoking – United States, 1996–2001. MMWR. 2003;52:303–307. [PubMed]
2. CDC. Annual smoking-attributable mortality, years of potential life lost, and economic costs-United States, 1995–1999. MMWR. 2002;51:300–303. [PubMed]
3. CDC. Cigarette smoking-attributable morbidity – United States, 2000. MMWR.2003;52:842–844. [PubMed]
4. Bock BC, Becker B, Monteiro R, et al. Physician intervention and patient risk perception among smokers with acute respiratory illness in the emergency department. Prev Med.2001;32:175–181. [PubMed]
5. Richman PB, Dinowitz S, Nashed A, Eskin B, et al. Prevalence of smokers and nicotine-addicted patients in a suburban emergency department. Acad Emerg Med. 1999;6:807–810. [PubMed]
6. Statistics NCH. Healthy people 2000 final review. Hyattsville, Maryland: Public Health Service; 2001.
7. Bernstein SL, Becker BM. Preventive care in the emergency department: diagnosis and management of smoking and smoking-related illness in the emergency department: a systematic review. Acad Emerg Med. 2002;9:720–729. [PubMed]
8. Elkins GR, Rajab MH. Clinical hypnosis for smoking cessation: preliminary results of a three-session intervention. Int J Clin Exp Hypn. 2002;52:73–81. [PubMed]
9. Covino NA, Bottari M. Hypnosis, behavioral theory, and smoking cessation. J Dent Educ. 2001;65:340–347. [PubMed]
10. Ahijevych K, Yerardi R, Nedilsky N. Descriptive outcomes of the American Lung Association of Ohio hypnotherapy smoking cessation program. Int J Clin Exp Hypn.2000;48:374–387. [PubMed]
11. Green JP, Lynn SJ. Hypnosis and suggestion-based approaches to smoking cessation: an examination of the evidence. Int J Clin Exp Hypn. 2000;48:195–224. [PubMed]
12. Bayot A, Capafons A, Cardena E. Emotional self-regulation therapy: a new and efficacious treatment for smoking. Am J Clin Hypn. 1997;40:146–156. [PubMed]
13. Hughes JA SL, Dunne JA, Tarpey J, Vickers MD. Reducing smoking. Anesthesia.1994;49:126–128.
14. Myles PS. Cessation of smoking following tape suggestion under anesthesia. Anesth and Int Care. 1992;20:540–541.
15. Myles PS, Richardson HM, Layher Y, et al. Double-blind, randomized trial of cessation of smoking after audiotape suggestion during anesthesia. Brit Jour Anesth. 1996;76:694–698.
16. Boudreaux ED, Clark S, Camargo CA., Jr Telephone follow-up after the emergency department visit: experience with acute asthma. On behalf of the MARC Investigators.Ann Emerg Med. 2000;35:555–563. [PubMed]
17. Richman PB DS, Nashed AH, Eskin B, et al. The Emergency department as a potential site for smoking cessation intervention: a randomized, controlled trial. Acad Emerg Med.2000;7:348–353. [PubMed]
18. Valbo A, Eide T. Smoking cessation in pregnancy: the effect of hypnosis in a randomized study. Addict Behav. 1996;21:29–35. [PubMed]
19. Abbot NC, Stead LF, White AR, et al. Hypnotherapy for smoking cessation. Cochrane Database of Systematic Reviews. 2000;(2):CD001008.
20. Law M TJ. An analysis of the effectiveness of interventions intended to help people stop smoking. Arch Intern Med. 1995;155:1933–1941. [PubMed]
21. Jorenby DE ES, Nides MA, Rennard SI, Johnston JA. A controlled trial of sustained-release Bupropion, a nicotine patch, or both for smoking cessation. New Eng J Med.1999;340:685–691. [PubMed]
22. Barber J. Freedom from smoking: integrating hypnotic methods and rapid smoking to facilitate smoking cessation. Int J Clin Exp Hypn. 2001;49:257–266. [PubMed]
23. Rodriguez RM, Kreider W, Baraff LJ. Need and desire for preventive care measures in ED patients. Ann Emerg Med. 1995;26:615–620. [PubMed]
24. Chernow SM, Iserson KV. Use of the emergency department for hypertension screening: a prospective study. Ann Emerg Med. 1987;16:180–182. [PubMed]
25. Rodriguez RM, Baraff L. Emergency department immunization of the elderly with pneumococcal and influenza vaccines. Ann Emerg Med. 1993;22:1729–1732. [PubMed]
26. Hogness CG, Engelstad LP, Linck LM, Schorr KA. Cervical cancer screening in an urban emergency department. Ann Emerg Med. 1992;21:933–939. [PubMed]
27. Burns RB, Stoy DB, Feied CF, et al. Cholesterol screening in the emergency department. J Gen Intern Med. 1991;6:210–215. [PubMed]
28. Moscovitz H, Brookoff D, Nelson L. A randomized trial of bromocriptine for users presenting to the emergency department. J Gen Int Med. 1993;8:1–4.


